VA Maintaining Internal Systems and Strengthening Integrated Outside Networks Act of 2018 (VA MISSION Act; P.L.115-182)
On June 6, 2018, the John S. McCain III, Daniel K. Akaka, and Samuel R. Johnson VA Maintaining Internal Systems and Strengthening Integrated Outside Networks Act of 2018, or the VA MISSION Act of 2018 (S. 2372; P.L. 115-182; H.Rept. 115-671), was signed into law. The Department of Veterans Affairs Expiring Authorities Act of 2018 (S. 3479; P.L. 115-251), enacted on September 29, 2018, made some changes and technical amendments to the VA MISSION Act. This act, as amended, broadly addresses four major areas.
First, it establishes a new permanent Veterans Community Care Program (VCCP), replacing the current Veterans Choice Program (VCP). The VA MISSION Act stipulates that the new program must be operational when regulations are published by the Department of Veterans Affairs (VA) no later than one year after the date of enactment (June 6, 2018), or when the VA determines that 75% of the amounts deposited in the Veterans Choice Fund (VCF) have been exhausted.
Second, it expands the current Program of Comprehensive Assistance for Family Caregivers, in two phases, to all eligible veterans who served prior to September 11, 2001.
Third, it establishes an asset and infrastructure review process by establishing an Asset and Infrastructure Review Commission. The purpose of the commission is to examine the VA’s assets and to make recommendations for modernizing and realigning medical facilities.
Fourth, it provides various statutory authorities to the Veterans Health Administration (VHA) of the VA to recruit and retain health care providers.
Veterans Community Care Program (VCCP)
The VA MISSION Act establishes a new permanent discretionary community care program known as VCCP. The act provides conditions under which the VA is required to provide care in the community once the program is established. Generally, all veterans enrolled in the VA health care system would be able to qualify when (1) the VA does not offer the care or service required by the veteran; or (2) the veteran resides in a state without a full-service VA medical facility; or (3) the veteran previously qualified under the 40-mile criterion of the VCP; or (4) the VA cannot provide the veteran with care and services that comply with designated access and quality standards; or (5) the veteran and the veteran’s primary care provider agree that it is in the best interest of the veteran to receive care in the community. In addition, the VA is required to enter into contracts to build a network of private community providers.
Expansion of Comprehensive Assistance for Family Caregivers
The VA MISSION Act expands the Program of Comprehensive Assistance for Family Caregivers to pre-9/11 veterans in two phases. Under the first phase, veterans with serious service-connected injuries incurred on or before May 7, 1975, would qualify for benefits over a two-year period beginning on the date when the VA certifies to Congress that it has fully implemented the information technology system required for this program. Under the second phase, those with serious service-connected injuries incurred between May 7, 1975, and September 11, 2001, would qualify for the Comprehensive Assistance for Family Caregivers program two years after implementation of the first phase.
Capital Asset Review
The VA MISSION Act establishes a process for realigning and modernizing facilities of the VHA. Under this process, the VA will develop criteria for selecting VHA facilities to dispose of, modernize, or acquire, so as to better meet the health care needs of veterans. VA must then create a list of recommendations based on those criteria and submit it to a newly created Asset Infrastructure Review (AIR) Commission. The AIR Commission shall review the VA’s recommendations but may not alter them, unless it determines that one or more recommendations are inconsistent with the criteria. The commission shall submit the list of recommendations to the President, who shall either approve the list in its entirety or send it back to the AIR Commission. The AIR Commission may change the recommendations and resubmit a revised list to the President for reconsideration. The President may approve or disapprove of the revised list. If the President approves of the original or revised list, then VA must begin implementation of the recommendations within three years, unless Congress passes a joint resolution of disapproval, in which case the asset review process terminates.
Recruiting and Retaining Health Care Providers in the VHA
The VA MISSION Act authorizes or expands several programs, with the intention of recruiting and retaining health care providers in the VHA. Among other things, the act
increases the maximum amount of student loan debt that may be reduced under VA’s Education Debt Reduction Program (EDRP);
authorizes designated scholarships for physicians and dentists under the VA Health Professional Scholarship Program (HPSP);
establishes the VA specialty education loan repayment program to incentivize VHA employees to pursue education and training in medical specialties for which VA determines there is a shortage;
establishes a pilot Veterans Healing Veterans Medical Access and Scholarship Program; and
extends eligibility for VA’s EDRP to clinical staff working at Vet Centers.
The act also requires the VHA to establish a program to deploy mobile health teams to serve in underserved VA medical facilities.
Lastly, the VA MISSION Act authorizes and appropriates $5.2 billion in mandatory funding for the VCP until the VCCP is operational.
VA Maintaining Internal Systems and Strengthening Integrated Outside Networks Act of 2018 (VA MISSION Act; P.L.115-182)
Jump to Main Text of Report
Contents
- Introduction
- Brief Legislative History of Community Care
- Background and Legislative History of the VA MISSION Act
- Budgetary Impact
- Provisions in the VA MISSION Act of 2018
- Title I: Caring for Our Veterans
- Subtitle A: Developing an Integrated High-Performing Network
- Section 100. Short Title
- Section 101. Establishment of the Veterans Community Care Program (VCCP)
- Section 102. Authorization of Agreements Between Department of Veterans Affairs and Nondepartment Providers
- Section 103. Authorizing State Veterans Homes to Enter into VCAs
- Section 104. Access Standards and Standards for Quality
- Section 105. Access to Walk-In Care
- Section 106. Strategy Regarding the VA High-Performing Integrated Health Care Network.
- Section 107. Applicability of Directive of Office of Federal Contract Compliance Programs
- Section 108. Prevention of Certain Health Care Providers from Providing Non-VA Health Care Services to Veterans
- Section 109. Remediation of Medical Service Lines
- Section 111. Prompt Payment to Providers
- Section 112. Authority to Pay for Authorized Care Not Subject to an Agreement
- Section 113. Improvement of Authority to Recover the Cost of Services Furnished for Nonservice-Connected Disabilities
- Section 114. Processing of Claims for Reimbursement Through Electronic Interface
- Section 121. Education Program on Health Care Options
- Section 122. Training Program for Administration of Non-VA Health Care
- Section 123. Continuing Medical Education for Non-VA Medical Professionals
- Section 131. Establishment of Processes to Ensure Safe Opioid Prescribing Practices by Non-VA Health Care Providers
- Section 132. Improving Information Sharing with Community Providers
- Section 133. Competency Standards for Non-VA Health Care Providers
- Section 134. VA Participation in National Network of State-Based Prescription Drug-Monitoring Programs
- Section 141. Plans for Use of Supplemental Appropriations
- Section 142. Veterans Choice Fund Flexibility
- Section 143. Sunset of Veterans Choice Program
- Subtitle B: Improving VA Health Care Delivery
- Section 151. Licensure of Health Care Professionals of the VA Providing Treatment Via Telemedicine
- Section 152. Authority for the VA Center for Innovation for Care and Payment
- Section 153. Authority for Operations on Live Donors for the Purposes of Conducting Transplant Procedures for Veterans
- Subtitle C: Family Caregivers
- Section 161. Expansion of Family Caregiver Program of the VA
- Section 162. Implementation of Information Technology System of the VA to Assess and Improve the Family Caregiver Program
- Section 163. Modification to Annual Evaluation Report on Caregiver Program of the VA
- Title II: VA Asset and Infrastructure Review
- Subtitle A: Asset and Infrastructure Review
- Section 201. Short Title
- Section 202. The Commission
- Section 203. Procedure for Making Recommendations
- Section 204. Actions Regarding Infrastructure and Facilities of the VHA
- Section 205. Implementation
- Section 206. Department of Veterans Affairs Asset and Infrastructure Review Account
- Section 207. Congressional Consideration of Commission Report
- Section 208. Other Matters
- Section 209. Definitions
- Subtitle B: Other Infrastructure Matters
- Section 211. Improvement to Training of Construction Personnel
- Section 212. Review of Enhanced Use Leases
- Section 213. Assessment of Health Care Furnished by the VA to Veterans Who Live in U.S. territories
- Title III: Improvements to Recruitment of Health Care Professionals
- Section 301. Designated Scholarships for Physicians and Dentists Under the VA Health Professional Scholarship Program
- Section 302. Increase in Maximum Amount of Debt That May Be Reduced Under Education Debt Reduction Program (EDRP) of the VA
- Section 303. Establishing the VA Specialty Education Loan Repayment Program
- Section 304. Veterans Healing Veterans Medical Access and Scholarship Program
- Section 305. Bonuses for Recruitment, Relocation, and Retention
- Section 306. Inclusion of Vet Center Employees in Education Debt Reduction Program (EDRP) of the VA
- Title IV: Heath Care in Underserved Areas
- Section 401. Development of Criteria for Designation of Certain Medical Facilities of the VA as Underserved Facilities and Plan to Address Problem of Underserved Facilities.
- Section 402. Pilot Program to Furnished Mobile Deployment Teams to Underserved Facilities
- Section 403. Pilot Program on Graduate Medical Education and Residency
- Title V: Other Matters
- Section 501. Annual Report on Performance Awards and Bonuses Awarded to Certain High-Level Employees
- Section 502. Role of Podiatrists in the VA
- Section 503. Definition of Major Medical Facility Project
- Section 504. Authorization of Certain Major Medical Facility Projects
- Section 505. VA Personnel Transparency
- Section 506. Program on Establishment of Peer Specialists in Patient-Aligned Care Team Settings Within VAMCs
- Section 507. VA Medical Scribe Program
- Section 508. Extension of VA Home Loan Guarantee Fees
- Section 509. Extension of Reduction in VA Pensions for Certain Medicaid-Covered Veterans in Nursing Facilities
- Section 510. Appropriation of Funds
- Section 512. Budgetary Effects
Figures
Summary
On June 6, 2018, the John S. McCain III, Daniel K. Akaka, and Samuel R. Johnson VA Maintaining Internal Systems and Strengthening Integrated Outside Networks Act of 2018, or the VA MISSION Act of 2018 (S. 2372; P.L. 115-182; H.Rept. 115-671), was signed into law. The Department of Veterans Affairs Expiring Authorities Act of 2018 (S. 3479; P.L. 115-251), enacted on September 29, 2018, made some changes and technical amendments to the VA MISSION Act. This act, as amended, broadly addresses four major areas.
First, it establishes a new permanent Veterans Community Care Program (VCCP), replacing the current Veterans Choice Program (VCP). The VA MISSION Act stipulates that the new program must be operational when regulations are published by the Department of Veterans Affairs (VA) no later than one year after the date of enactment (June 6, 2018), or when the VA determines that 75% of the amounts deposited in the Veterans Choice Fund (VCF) have been exhausted.
Second, it expands the current Program of Comprehensive Assistance for Family Caregivers, in two phases, to all eligible veterans who served prior to September 11, 2001.
Third, it establishes an asset and infrastructure review process by establishing an Asset and Infrastructure Review Commission. The purpose of the commission is to examine the VA's assets and to make recommendations for modernizing and realigning medical facilities.
Fourth, it provides various statutory authorities to the Veterans Health Administration (VHA) of the VA to recruit and retain health care providers.
Veterans Community Care Program (VCCP)
The VA MISSION Act establishes a new permanent discretionary community care program known as VCCP. The act provides conditions under which the VA is required to provide care in the community once the program is established. Generally, all veterans enrolled in the VA health care system would be able to qualify when (1) the VA does not offer the care or service required by the veteran; or (2) the veteran resides in a state without a full-service VA medical facility; or (3) the veteran previously qualified under the 40-mile criterion of the VCP; or (4) the VA cannot provide the veteran with care and services that comply with designated access and quality standards; or (5) the veteran and the veteran's primary care provider agree that it is in the best interest of the veteran to receive care in the community. In addition, the VA is required to enter into contracts to build a network of private community providers.
Expansion of Comprehensive Assistance for Family Caregivers
The VA MISSION Act expands the Program of Comprehensive Assistance for Family Caregivers to pre-9/11 veterans in two phases. Under the first phase, veterans with serious service-connected injuries incurred on or before May 7, 1975, would qualify for benefits over a two-year period beginning on the date when the VA certifies to Congress that it has fully implemented the information technology system required for this program. Under the second phase, those with serious service-connected injuries incurred between May 7, 1975, and September 11, 2001, would qualify for the Comprehensive Assistance for Family Caregivers program two years after implementation of the first phase.
Capital Asset Review
The VA MISSION Act establishes a process for realigning and modernizing facilities of the VHA. Under this process, the VA will develop criteria for selecting VHA facilities to dispose of, modernize, or acquire, so as to better meet the health care needs of veterans. VA must then create a list of recommendations based on those criteria and submit it to a newly created Asset Infrastructure Review (AIR) Commission. The AIR Commission shall review the VA's recommendations but may not alter them, unless it determines that one or more recommendations are inconsistent with the criteria. The commission shall submit the list of recommendations to the President, who shall either approve the list in its entirety or send it back to the AIR Commission. The AIR Commission may change the recommendations and resubmit a revised list to the President for reconsideration. The President may approve or disapprove of the revised list. If the President approves of the original or revised list, then VA must begin implementation of the recommendations within three years, unless Congress passes a joint resolution of disapproval, in which case the asset review process terminates.
Recruiting and Retaining Health Care Providers in the VHA
The VA MISSION Act authorizes or expands several programs, with the intention of recruiting and retaining health care providers in the VHA. Among other things, the act
- increases the maximum amount of student loan debt that may be reduced under VA's Education Debt Reduction Program (EDRP);
- authorizes designated scholarships for physicians and dentists under the VA Health Professional Scholarship Program (HPSP);
- establishes the VA specialty education loan repayment program to incentivize VHA employees to pursue education and training in medical specialties for which VA determines there is a shortage;
- establishes a pilot Veterans Healing Veterans Medical Access and Scholarship Program; and
- extends eligibility for VA's EDRP to clinical staff working at Vet Centers.
The act also requires the VHA to establish a program to deploy mobile health teams to serve in underserved VA medical facilities.
Lastly, the VA MISSION Act authorizes and appropriates $5.2 billion in mandatory funding for the VCP until the VCCP is operational.
Introduction
Policymakers and other stakeholders may hold a variety of views regarding the appropriate role of the private sector in meeting the health care needs of eligible veterans. Some believe that the best course for veterans is to provide all needed care in facilities under the direct jurisdiction of the Department of Veterans Affairs (VA), Veterans Health Administration (VHA), health care system. On the other hand, some see the use of private sector providers as important in ensuring veterans' access to a comprehensive slate of services (in particular, to specialty services that are needed infrequently), or in addressing geographic or other access barriers, such as long wait times for an appointment. In addition, those who believe that all needed care should be provided by VA providers in VA-owned facilities express concern that private sector options for providing care to veterans may dilute the quality of care in the VA health care system, and could fail to leverage key strengths of the VA health care network.
Furthermore, studies have shown that private sector community providers may not have the necessary training and skills to provide "complex and specialized multidisciplinary care including integrated behavioral health services that many veterans require."1 Some are concerned that if veterans leave the VA health care system for the private sector, some VHA sites and specialized medical services may be eliminated from the VA health care system, if comparable care is provided in the private sector.2 However, some propose that over the long term, having private sector options could improve the quality of services within the VA health care system through competition. Reaching the correct balance between providing care through VHA's health care system and through non-VA community providers has been an issue for policymakers, as well as for the VA and other stakeholders, for many years. On June 6, 2018, President Donald Trump signed into law the John S. McCain III, Daniel K. Akaka, and Samuel R. Johnson VA Maintaining Internal Systems and Strengthening Integrated Outside Networks Act of 2018, or the VA MISSION Act of 2018 (S. 2372; P.L. 115-182; H.Rept. 115-671). The Department of Veterans Affairs Expiring Authorities Act of 2018 (S. 3479; P.L. 115-251), enacted on September 29, 2018, made some changes and technical amendments to the VA MISSION Act. Section 101 of this act, establishing the Veterans Community Care Program, or VCCP, is a legislative outcome of this long-standing policy debate on the role of the private sector in the delivery of health care to the nation's veterans.
To understand the key amendments made by the VA MISSION Act with respect to care provided through private sector community providers, this report begins with a brief history of key legislative changes to community care passed by Congress from the 1920s onwards. It should be noted that over the years, care provided through private sector providers has been known by many names, including "Hometown Medical Program," "Non-VA Fee Care," "Fee-Basis Care," "Purchased Care," "Preauthorized Care," and the "Fee-Care Program," among others.3 In this report, such care is referred to as the Veterans Community Care Program, or VCCP, as established by the VA MISSION Act. Following the brief legislative history of VA provided community care, the report describes the background and legislative history leading up to the enactment of the VA MISSION Act. This is followed by summaries of the major provisions in the VA MISSION Act by title. The report concludes with an appendix providing implementation and reporting deadlines contained in the VA MISSION Act.
Brief Legislative History of Community Care
Since the early 1920s, Congress has authorized the VA to contract for care in the community. For instance, the World War Veterans Act of 1924 (P.L. 68-242), enacted on June 7, 1924, included language that authorized the Director of the then Veterans Bureau to contract with private facilities in exceptional cases:
In the event Government hospital facilities are insufficient or inadequate the director may contract with State, municipal, or in exceptional cases, with private hospitals for such medical, surgical, and hospital services and supplies as may be required, and such contracts may be made for a period of not exceeding three years and may be for the use of a ward or other hospital unit or on such other basis as may be in the best interest of the beneficiaries under this Act.4
VA's Hometown Medical Care Program, which was also known as the fee-basis care program, was established by the VA in FY1946, and under this program the VA entered into contracts with state medical societies, or with designated agencies for authorized services, and was reimbursed based on a VA fee schedule.5 Generally, the Hometown Medical Program was used to provide out-patient care—including dental care for veterans who were in need of treatment for a service-connected disability—because at that time outpatient care was generally authorized for treatment of service-connected disabilities.6 According to VA's annual report from FY1950:
This program has saved veterans many hours they would otherwise have been required to use in traveling to and from VA clinics, some of which would have been lost from their work. The convenience of treatment in their own hometown, together with the privilege of being treated by a doctor of their own choice, has made this [program] highly acceptable to veteran-patients.7
In June 1957, Congress passed the Veterans' Benefit Act of 1957 (P.L. 85-56), which provided the VA the authority to contract with private facilities "in order to provide hospital care (i) in emergency cases for persons suffering from service-connected disabilities or from disabilities for which such persons were discharged or released from the active military, naval, or air service; (ii) for women veterans of any war; or (iii) for veterans of any war in a Territory, Commonwealth, or possession of the United States."8
The Veterans Health Care Expansion Act of 1973 (P.L. 93-82) broadly expanded out-patient care to nonservice-connected veterans, and by 1976, to address the "patient and staff complaints generated by the overcrowded conditions in outpatient programs and ambulatory care services at VA health care facilities across the Nation."9 Congress passed the Veterans Omnibus Health Care Act of 1976 (P.L. 94-581). This law made several changes to the fee-basis program. It added current (38 U.S.C. §1703) statutory language stating that "when facilities [Departmental] are not capable of furnishing economical care because of geographical inaccessibility or of furnishing the care or services required" and further limited fee-basis or contract care to specific categories of veterans. These included veterans receiving hospital care or medical services for the treatment of a service-connected disability or a disability for which a veteran was discharged or released from the active military, naval, or air service, among other categories.
Further changes made by the Veterans' Health Care Amendments of 1979 (P.L. 96-22) provided authority for fee-basis care for veterans with nonservice-connected disabilities and in receipt of increased pension or other additional compensation who are in need of regular aid and attendance or who are housebound. The Consolidated Omnibus Budget Reconciliation Act of 1985 (Veterans' Health-Care Amendments of 1986; P.L. 99-272) clarified the definition of the term "Veterans' Administration facilities" and authorized the VA to contract for medical care in private facilities. These and other legislative changes in subsequent Congresses eventually became codified at Title 38 United State Code (U.S.C.) section 1703. This section was completely amended by the VA MISSION Act (S. 2372; P.L. 115-182; H.Rept. 115-671; and P.L. 115-251).
Over time, Congress has authorized additional programs to provide care through non-VA community providers or entities, each with their own unique requirements. In general, the VA MISSION Act amends the legal framework around several existing veterans care programs: the Veterans Choice Program (38 U.S.C. §1701 note), Traditional VA Care in the Community (38 U.S.C. §1703), Project ARCH (Access Received Closer to Home) (38 U.S.C. §1703 note), community nursing home and adult health day care, home health care services, respite care, and hospice care (38 U.S.C. §§1720; 1720B and 1720C). It also creates a new program for walk-in care (38 U.S.C. §1725A). However, it leaves intact other statutory provisions for emergency care for nonservice-connected conditions to certain veterans (38 U.S.C. §1725), authority to provide reimbursement for emergency care for service-connected veterans (38 U.S.C. §1728), authority to share health care resources with the Department of Defense (38 U.S.C. §8111), health care sharing and contracting authority (38 U.S.C. §8153), and agreements with Indian Health Service and tribal health program providers (25 U.S.C. §1645).
Background and Legislative History of the VA MISSION Act
In response to the allegations of wait time manipulation and access issues at many VHA hospitals and clinics across the country, which were brought to the attention of congressional committees in the spring and summer of 2014,10 the Veterans Access, Choice and Accountability Act of 2014 (VACAA; P.L. 113-146, as amended) was enacted. This act, among other things, established the temporary Veterans Choice Program (VCP), which authorized veterans meeting certain criteria, such as wait times for appointments and distance from the nearest VA medical facility, to access care in the community.11 In addition, Section 802 of VACAA established the Veterans Choice Fund (VCF) and provided $10 billion in mandatory appropriations.
Significant challenges surrounding the implementation of the VCP are documented in several VA Office of Inspector General (OIG) and Government Accountability Office (GAO) reports, as well as congressional hearings.12
Acknowledging these implementation challenges associated with VCP, as well as the confusing and complex community care landscape created by the various statutory authorities, coupled with pilot programs such as Project Access Received Closer to Home (ARCH)13 and Patient-Centered Community Care (PC3),14 Congress passed the Surface Transportation and Veterans Health Care Choice Improvement Act of 2015 (P.L. 114-41) and mandated the VA to provide a plan to consolidate existing community care programs. This plan was submitted to Congress on October 30, 2015.15 Numerous hearings were held during the 114th Congress, and several measures were introduced to incorporate many of the concepts addressed in the VA's Plan to Consolidate Programs of Department of Veterans Affairs to Improve Access to Care, such as the Improving Veterans Access to Care in the Community Act (S. 2633) and the Veterans Choice Improvement Act of 2016 (S. 2646). However, at the end of the 114th Congress, no major legislative action occurred to revamp and consolidate veterans community care programs.
At the beginning of the 115th Congress, once again Congress faced implementation issues regarding the VCP, including its expiration in August 2017 and funding shortfalls. In response to this, Congress passed P.L. 115-26 (unofficially referred to as the Veterans Choice Program Improvement Act), eliminated the August 7, 2017, sunset date, and allowed the VCP to continue until all funds in the VCF were expended. Later in 2017, as VCF funding was diminishing, Congress passed the VA Choice and Quality Employment Act of 2017 (P.L. 115-46), and P.L. 115-96, and provided additional funding of $4.2 billion to continue VCP.
In the meantime, on October 6, 2017, the VA submitted to the House and Senate Veterans' Affairs Committees another plan to consolidate and streamline community care programs to replace the VCP. This plan, known as the Veterans Coordinated Access & Rewarding Experiences (CARE) plan, made additional enhancements to the initial plan that was provided in October 2015. More specifically, it focused on eligibility criteria for veterans to access care in the community, with criteria based on clinical need, quality of care, and convenience—which had not been specifically addressed in the October 2015 plan.16 The House Veterans' Affairs Committee (HVAC) held a hearing on the CARE plan and other legislative proposals on October 24, 2017.17 Based on major concepts in this plan and other legislative proposals,18 the Senate and House Veterans' Affairs Committees began drafting legislation. On November 3, 2017, the VA Care in the Community Act (H.R. 4242) was introduced, and the measure was marked up by the HVAC and ordered reported as amended on December 19, 2017. It was subsequently reported with an amendment by the HVAC (H.Rept. 115-585) on March 5, 2018. On November 29, 2017, the Senate Veterans' Affairs Committee (SVAC) marked up a draft measure, and it was reported to the Senate on December 5, 2017, entitled the Caring for Our Veterans Act of 2017 (S. 2193; S.Rept. 115-212). However, no further action occurred at the close of the first session of the 115th Congress.
At the beginning of the second session of the 115th Congress, combining various provisions of the VA Care in the Community Act (H.R. 4242; H.Rept. 115-585), the VA Asset and Infrastructure Review Act of 2017 (H.R. 4243), and the Caring for Our Veterans Act of 2017 (S. 2193; S.Rept. 115-212), HVAC Chairman Dr. Phil Roe introduced the VA Maintaining Internal Systems and Strengthening Integrated Outside Networks Act of 2018, or the VA MISSION Act of 2018 (H.R. 5674), on May 3, 2018. The HVAC marked up the legislation on May 8. The measure was reported by the HVAC on May 11 (H.Rept. 115-671, Part 1). The text of H.R. 5674 was then substituted as an amendment to S. 2372 and modified to include a new short title known as the John S. McCain III, Daniel K. Akaka, and Samuel R. Johnson VA Maintaining Internal Systems and Strengthening Integrated Outside Networks Act of 2018. The House passed S. 2372 on May 16. The Senate began consideration of the House amendment to S. 2372 on May 17, and it passed the measure by concurring to the House amendment to S. 2372 on May 23. President Donald Trump signed the VA MISSION Act to law (S. 2372; P.L. 115-182) on June 6, 2018.19 The Department of Veterans Affairs Expiring Authorities Act of 2018 (S. 3479; P.L. 115-251) made amendments and technical corrections to the VA MISSION Act.
Budgetary Impact20
The VA MISSION Act of 2018 (P.L. 115-182) provides $5.2 billion in direct or mandatory appropriations for the VCF established by Section 802 of the VACAA (P.L. 113-146, as amended). The Congressional Budget Office (CBO) estimates that this amount would continue to provide funding for the current VCP until about the first half of calendar year 2019.21 Excluding this direct appropriation, the CBO estimates that implementing all the provisions of the VA MISSION Act would cost approximately $46.5 billion over the FY2019-FY2023 time frame, subject to discretionary appropriations from Congress. This estimate includes a cost of $21.4 billion for the new Veterans Community Care Program (VCCP) and $6.7 billion for the provisions related to expansion of the Program of Comprehensive Assistance for Family Caregivers to those veterans injured or disabled during military service on or before September 11, 2001. The $6.7 billion estimate excludes any long-term implementation costs of this expansion, since the expansion would happen in two stages.22 The CBO estimates that the VA MISSION Act would increase the deficit by $5.2 billion over six years (FY2018-FY2023) and almost $4.5 billion over 11 years (FY2018-FY2028).23
Provisions in the VA MISSION Act of 2018
This report summarizes the major provisions of the John S. McCain III, Daniel K. Akaka, and Samuel R. Johnson VA Maintaining Internal Systems and Strengthening Integrated Outside Networks Act of 2018 (VA MISSION Act; P.L. 115-182, H.Rept. 115-671), including amendments made by the Department of Veterans Affairs Expiring Authorities Act of 2018 (S. 3479; P.L. 115-251). It does not analyze every provision in the act, but instead provides brief outlines of the matters addressed.
Subsequent sections of the report are organized as follows: a summary is provided for each title of the act, followed by a summary of the provisions under that respective title. Relevant background is provided for context, where applicable, at the title level or subtitle level.
Throughout this report, unless otherwise stated, the Secretary means the Secretary of Veterans Affairs, and the VA means the U.S. Department of Veterans Affairs. In addition, this section refers to matters addressed under that specific section of the act. This report uses a number of acronyms,
|
Acronyms |
|
|
CBO |
Congressional Budget Office |
|
CBOC |
Community Based Outpatient Clinic |
|
C.F.R. |
Code of Federal Regulations |
|
CMS |
Centers for Medicare & Medicaid Services |
|
DOD |
Department of Defense |
|
DME |
Durable Medical Equipment |
|
EDRP |
Education Debt Reduction Program |
|
FQHC |
Federally Qualified Health Center |
|
GAO |
Government Accountability Office |
|
GME |
Graduate Medical Education |
|
GSA |
General Services Administration |
|
HAC |
House Appropriations Committee |
|
HHS |
Department of Health and Human Services |
|
HPSP |
Health Professional Scholarship Program |
|
HPSA |
Health Professional Shortage Areas |
|
HVAC |
House Committee on Veterans' Affairs |
|
IHS |
Indian Health Service |
|
OIG |
VA Office of Inspector General |
|
PDMP |
State Prescription Drug Monitoring Program |
|
SAC |
Senate Appropriations Committee |
|
SVAC |
Senate Committee on Veterans' Affairs |
|
U.S.C. |
United States Code |
|
VA |
Department of Veterans Affairs |
|
VACAA |
Veterans Access, Choice, and Accountability Act of 2014 (P.L. 113-146, as amended; 38 U.S.C. §1701 note) |
|
VAMC |
VA Medical Center |
|
VCA |
Veterans Community Care Agreements |
|
VCCP |
Veterans Community Care Program |
|
VCF |
Veterans Choice Fund |
|
VCP |
Veterans Choice Program |
|
VHA |
Veterans Health Administration |
|
VISN |
Veterans Integrated Services Networks |
|
VSO |
Veterans Service Organization |
Title I: Caring for Our Veterans
This title amends current law (codified at 38 U.S.C. §1703) that provided the Secretary the authority—whether under a contract or an individual authorization—to provide care under certain circumstances
- care of a service-connected disability;
- care for a disability for which a veteran was discharged or released from the active military, naval, or air service;
- care of a disability of a veteran who has a total disability permanent in nature from a service-connected disability;
- care of a disability associated with and held to be aggravating a service-connected disability;
- care of a disability of a veteran participating in a rehabilitation program under 38 U.S.C. Chapter 31;
- hospital care for women veterans;
- outpatient dental care for certain veterans; and
- when there is a need for hospital care for reasons set forth in VA regulations (38 C.F.R. §17.52).
Title I liberalizes the VA's current community care program by establishing a new Veterans Community Care Program (VCCP), which amends the above-mentioned statutory hierarchy and provides greater flexibility to all enrolled veterans in accessing care in the community, for hospital care, medical services, and extended care services, at their election. Under the new VCCP, eligibility will apply more broadly to all enrolled veterans and service-connected disability will not be a major factor for eligibility for care in the community. In addition, this title would eventually sunset the current Veterans Choice Program (VCP) one year after the date of enactment of the VA MISSION Act (i.e., on June 6, 2019).
This title requires the Secretary to establish access and quality standards for medical care and extended care services. It authorizes the VA to enter into Veteran Care Agreements (VCAs) that are not subject to the contracting requirements generally required under federal contracting regulations. In addition, the VA is authorized to enter into VCAs with State Veterans Homes, thereby eliminating the need for contractual agreements with the VA. These VCAs will not be considered federal contracts with the United States; however, State Veterans Homes will still have to comply with all other applicable federal laws concerning employment and hiring practices. Title I also requires the Secretary to conduct a quadrennial market area assessment of VA health services, and to develop a broad-ranging quadrennial review of the VHA. It also expands eligibility for veterans to access walk-in care from private community providers. Moreover, this title amends VA's prompt payment standards for all community care providers. It also requires the Secretary to develop and administer a program to educate veterans about the interaction between health insurance programs such as Medicare, Medicaid, and TRICARE and the services provided by the VA health care system. Title I also requires the Secretary to improve information sharing with community providers and to ensure the competency of private community providers. It also provides VA clinicians access to State Prescription Drug Monitoring Programs (PDMPs).
This title also provides authority for VA providers to provide a telemedicine episode of care without regard to where the veteran patient and VA provider are located within the United States and U.S. territories. Furthermore, it establishes a VA Innovation for Care and Payment Center, and provides the Secretary with authority to conduct pilot programs to develop innovative payment and health care delivery models.
Lastly, Title I liberalizes eligibility for the Program of Comprehensive Assistance for Family Caregivers to pre-9/11 veterans under two phases. Under the first phase, veterans with serious service-connected injuries incurred on or before May 7, 1975, will qualify for benefits over a two-year period beginning on the date when the VA certifies to Congress that it has fully implemented the information technology system required for this program. Under the second phase, those with serious service-connected injuries incurred between May 7, 1975, and September 11, 2001, will qualify for the Comprehensive Assistance for Family Caregivers program two years after the implementation of the first phase.
Subtitle A: Developing an Integrated High-Performing Network
Section 100. Short Title
This section provides the title as the "Caring for Our Veterans Act of 2018."
Section 101. Establishment of the Veterans Community Care Program (VCCP)
This section amends current law (38 U.S.C. §1703) and establishes a new Veterans Community Care Program (VCCP) to provide hospital care, medical services, and extended care services to eligible veterans through specified non-VA health care providers. Once VCCP is implemented by the Secretary, it would entirely replace current provisions in Section 1703 that provide authority for hospital care and medical services in non-VA facilities. In the following paragraphs, this section means the newly amended Section 1703 and its subdivisions.
Care Coordination
This section requires the Secretary to coordinate care provided through the VCCP to eligible veterans. This care coordination must include at least the following: (1) timely scheduling of medical appointments, including the establishment of a mechanism to receive medical records from non-VA providers; (2) ensuring the continuity of care and services; (3) coordinating among regional networks if the eligible veteran accesses care and services in a different network than the regional network in which the veteran resides; and (4) ensuring that eligible veterans do not experience a lapse in care or an unusual or excessive burden in accessing care because of errors or delays by the VA or its contractors.
Eligible Veterans
This section stipulates that any veteran enrolled in the VA health care system,24 or any veteran who is not enrolled in the VA health care system but is entitled to hospital care, medical services, and extended care services, is eligible for care through the VCCP.25
Specified Community Health Care Providers
This section requires that eligible veterans be provided care through the following non-VA health care providers: (1) any physician or practitioner or health care provider participating in the Medicare program,26 (2) DOD medical facilities,27 (3) IHS medical facilities,28 (4) any FQHCs,29 or (5) any other health care provider that meets criteria established by the Secretary.
Eligibility for Community Care
This section stipulates two major provisions under which the Secretary
- is required to authorize care, subject to the availability of annual appropriations, to eligible veterans through VCCP; or
- may authorize care through VCCP to eligible veterans.
These provisions are further delineated below (see Figure 1 and Figure 2).
Conditions under which care is required to be provided by the VA through VCCP:
An eligible veteran can elect to receive care if he or she meets one of the five major conditions:
- 1. the VA does not offer the care or services the veteran requires; or
- 2. the VA does not operate a full-service VA medical facility in the state the veteran resides; or
- 3. the veteran was eligible for care under the 40-mile distance eligibility criteria under the previous Veterans Choice Program (VCP)30 on the day before the date of enactment of the Caring for Our Veterans Act of 2018 (i.e., the veteran was eligible on June 5, 2018); and continues to reside in the same location that qualifies the veteran under the 40-mile distance eligibility criteria; and
(a) resides in one of the five states with the lowest population density based on data from the 2010 decennial census or
(b) resides in a state other than the five states with the lowest population density and
- received care or services through the VA within one year before the enactment of the Caring for Our Veterans Act of 2018 (i.e., June 6, 2018) and
- is seeking care or services within two years of the date of the enactment of the Caring for Our Veterans Act of 2018 (i.e., June 6, 2018); or
- 1. the VA is unable to provide care or services that is requested by the veteran in a manner that meets designated access standards for care or services as developed by the Secretary; or
- 2. the veteran's referring clinician agrees, after consultations with the eligible veteran, that care and services through VCCP would be in the best medical interest of the veteran based on criteria established by the Secretary (see text box below).
|
Factors to Be Considered by the VA Secretary when Developing Criteria to Be Used by a Referring Clinician The Secretary is required to consider the following factors when developing criteria to be used by an eligible veteran's clinician to refer the veteran for care through VCCP:
|
Election of the Veteran
This section stipulates that the decision to receive care or services authorized by the Secretary through VCCP by an eligible veteran will be at the election of that veteran.
|
Figure 1. Conditions Under Which Care Is Required to Be Provided Through the Veterans Community Care Program (VCCP) (38 U.S.C. §1703(d)) |
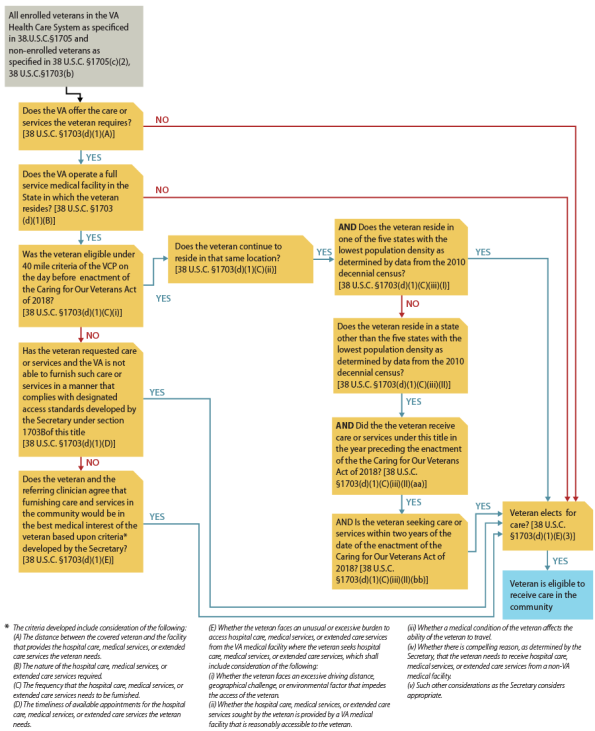 |
|
Source: Figure developed by CRS based on statutory language in Section 101(a) of P.L. 115-182. Notes: This pathway may be subject to changes based on regulations to be published by the Department of Veterans Affairs. |
Conditions under which care may be authorized by VA to be provided through VCCP:
This section authorizes the Secretary to provide care through the VCCP to an eligible veteran if a VA medical service line (defined as a clinic within a VAMC) required by the veteran fails to comply with access and quality standards. The Secretary is required to develop access and quality standards, and is required to consider the following factors when developing those quality standards:
- compare the timeliness of a VA medical service line at two VA facilities, and
- compare the quality of care of a VA medical service line at one VA facility with two or more distinct and appropriate quality measures at non-VA medical service lines in the community.
This section limits the number of medical service lines that the Secretary could compare at any one VA facility to no more than three; it limits the total number of medical service lines nationwide to no more than 36. The care provided under this authorization would end when the deficient medical service line has been remedied. A veteran is eligible to receive care through VCCP under this provision until the completion of an episode of care, and the Secretary is required to ensure the coordination of such care through VCCP.
|
Figure 2. Conditions Under Which the VA May Authorize Care to be Provided Through the Veterans Community Care Program (VCCP) (38 U.S.C. §1703(e)) |
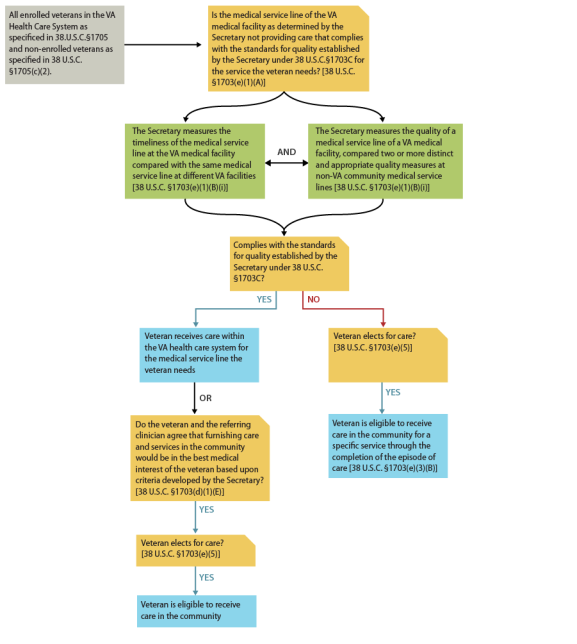 |
|
Source: Figure developed by CRS based on statutory language in Section 101 (a) of P.L. 115-182. Notes: This pathway may be subject to changes based on regulations to be published by the Department of Veterans Affairs. |
Federal Register Publication
This section requires the Secretary to publish a notice in the Federal Register, at least once a year, stating (1) the time period during which such care and services will be available, (2) the location or locations where such care and services will be available, and (3) the clinical services available at each location.
Review of VCCP Authorization Decisions
This section states that eligible veterans who disagree with authorization of care decisions determined through VCCP may appeal such decisions through VHA's internal clinical decision appeals process and cannot file an appeal with the Board of Veterans' Appeals (BVA).
Tiered Network
This section authorizes the Secretary to develop a tiered network of eligible providers based on criteria established by the Secretary. However, the Secretary is prohibited from prioritizing providers in one tier over those in another tier in a manner that limits the choice of an eligible veteran to select an eligible VCCP health care provider.
Contracts to Establish Networks of Health Care Providers31
This section requires the Secretary to enter into consolidated, competitively bid contracts to establish networks of health care providers, including any physician or practitioner or health care entity participating in the Medicare program32 and any other health care provider that meets criteria established by the Secretary. The section stipulates that it does not restrict the Secretary's authority to modify a contract after entering into such a contract.
Appointments Using Advanced Technology
This section requires the Secretary to ensure that eligible veterans are able to make their own appointments using advanced technology.
Responsibility for the Scheduling of Appointments
This section requires the Secretary to be responsible for the scheduling of appointments for eligible veterans.
Termination of Contracts
This section authorizes the Secretary to terminate contracts intended to establish networks of health care providers. When the Secretary notifies an entity of his or her intention to terminate the contract, the Secretary is required to notify the SVAC and HVAC that the entity failed to meet, at a minimum, at least one of the following provisions:
- comply substantially with the provisions of the contract or with VCCP regulations established by the Secretary; or
- comply with the access standards or the standards for quality established by the Secretary; or
- be excluded from participation in a federal health care program; or
- be identified as an excluded source on the list maintained in the System for Award Management, or any successor system; or
- have been convicted of a felony or other serious offense under federal or state law, and the continued participation of the entity would not be in the best interests of veterans or the VA.
The Secretary may also terminate a contract if it is no longer needed based on the health care needs of veterans, or if there are other contracts or sharing agreements. This section also requires the Secretary to submit a report to SVAC and HVAC regarding contract terminations.
Whenever the Secretary notifies a contractor that it is failing to meet contractual obligations required by the Secretary in the respective contract, the Secretary shall submit to SVAC and HVAC a report on such failure. The report must include the following:
- an explanation of the reasons for providing a notice to a contractor for terminating a contract;
- a description of the effect of the contractor's failure to meet contractual obligations, including with respect to cost, schedule, and requirements;
- a description of the actions taken by the Secretary to mitigate failures by the contractor to meet its contractual obligations;
- a description of the actions taken by the contractor to address failures in meeting its contractual obligations; and
- a description of any effect on the community provider market for veterans in the affected area.
Interim Recognition of Credentials and Qualifications33
This section requires the Secretary to instruct an entity that was awarded a contract to establish networks of health care providers to recognize and accept, on an interim basis, the credentials and qualifications of health care providers who are authorized to furnish care to veterans under a community care program prior to the establishment of the VCCP. These include providers under the Patient-Centered Community Care Program (PCCC)34 and the Veterans Choice Program (VCP).
Systems for Monitoring the Quality of Care
This section requires the Secretary to establish a system to monitor the quality of care provided through a network, or networks, of providers prior to contract renewal for such a network.
Payment Rates for Care and Services
This section stipulates that, with some exceptions, the rate paid for care or services through VCCP may not exceed the rate paid to providers under the Medicare program under Title XVIII of the Social Security Act, set by the Centers for Medicare & Medicaid Services (CMS), including rates paid under Medicare for Durable Medical Equipment (DME). However, the Secretary may negotiate and pay a higher rate than the established Medicare rate for eligible veterans in highly rural areas. Furthermore, in the state of Alaska, the VA will be able to reimburse providers under the VA Alaska Fee Schedule; in states with an All-Payer Model agreement, the VA will calculate Medicare payments based on payment rates under such agreements.35 When a given type of care or service is not payable under Medicare rates, or is payable under Medicare but does not have established pricing at the national or local level, those services are required to be paid based on rates established by the Secretary. The Secretary may also use alternative value-based reimbursement models to promote high-quality care through VCCP.
Treatment of Veterans Other Health Insurance
This section requires the Secretary to collect or recover reasonable charges for the cost of medical care or services furnished to an eligible veteran under VCCP for a nonservice-connected disability if the veteran has third-party health insurance coverage. The VA's right to recovery and collections is limited to the same extent as when the veteran or community care provider would otherwise be eligible to receive payment for such medical care or services from a third-party payer, such as a private medical insurer, if the care or services had not been furnished by the VA.
Veterans Out-of-Pocket Expenses
This section stipulates that an eligible veteran's copayments under VCCP will be the same as the copayments paid for the same nonservice-connected care or services provided at a VA medical facility.
Authority for Organ Transplant Coverage
This section requires the Secretary to authorize organ or bone marrow transplants to eligible veterans at non-VA facilities. An eligible veteran under this section is a (1) veteran who requires an organ or bone marrow transplant, and (2) based on the veteran's primary care provider's opinion, has a medical necessity to travel outside the Organ Procurement and Transplantation Network (OPTN)36 region in which the veteran resides.
Monitoring and Assessing of Care Provided Through VCCP
This section requires the Secretary to submit a report to the SVAC, HVAC, SAC, and HAC on the types and frequency of care provided under VCCP. The first report is due no later than 540 days after the enactment of the Caring for Our Veterans Act of 2018, and annually thereafter. The report must include the following data elements, among others: (1) the top 25% of types of care and services most frequently provided under VCCP because the VA is not providing such care and services; (2) the frequency of care and services that were sought by eligible veterans under VCCP; (3) an analysis of why the VA was not able to provide care and services sought by eligible veterans; (4) steps the VA took to provide care and services at a VA medical facility; and (5) the cost of care and services provided under VCCP.
This section also requires the Secretary to compile various data elements, gap analysis, and assessments of care provided under VCCP. These include, among others, (1) data on the types of care and services and the number of veteran patients using each type of care; (2) gaps in care and services provided through VCCP community care networks; (3) identification of ways in which those gaps can be fixed; (4) assessment of the total amounts spent by the VA to provide care to eligible veterans through VCCP community care networks; (5) assessment of the timeliness of VA referrals to VCCP community care networks; and (6) assessment of the timeliness of VCCP community care networks in accepting referrals and scheduling appointments. Furthermore, the Secretary is required to report on the number of VA medical service lines not providing care under standards developed by the Secretary, and to assess the use of academic affiliates and other federal health care facilities under VCCP. The Secretary is required to provide a report on all the above information to SVAC and HVAC no later than 540 days after the date of the enactment, and annually thereafter.
Prohibition on Limiting Medical Care and Services
This section prohibits the Secretary from limiting hospital care, medical services, or extended care services under VCCP if it is in the best interest of the eligible veteran, as determined by the veteran and the veteran's health care provider.
No Changes in Eligibility Criteria
This section states that no changes are made to a veteran's eligibility criteria for hospital care, medical services, or extended care services under VCCP (i.e., if a veteran is not eligible under current law for a specific care or service, he or she is not eligible for that specific care or service under VCCP).
Effective Date of VCCP and Publication of Regulations to Implement VCCP
This section stipulates that the effective date of VCCP implementation would be the later of (a) a date that is 30 days after the date the Secretary submits a final report to Congress in which the Secretary determines that 75% of the amounts deposited in the Veterans Choice Fund, established under the Veterans Access, Choice, and Accountability Act of 2014 (P.L. 113-146; as amended), have been exhausted, or (b) on the date when the Secretary is required to promulgate regulations implementing VCCP, which is one year after the date of the enactment (i.e., June 6, 2019).
Continuity of Existing Community Care Agreements
This section requires the Secretary to continue all existing contracts, memorandums of understanding, memorandums of agreement, and other arrangements between the VA and the American Indian and Alaska Native health care systems and Native Hawaiian health care systems.
Section 102. Authorization of Agreements Between Department of Veterans Affairs and Nondepartment Providers
This section amends current law to add a new 38 U.S.C. §1703A, which authorizes the Secretary to enter into agreements with community providers. In the following paragraphs, "this section" means the newly amended §1703A and its subdivisions.
Authorization of Community Care Agreements
This section authorizes the Secretary to enter into agreements known as Veterans Care Agreements (VCAs) if care cannot be feasibly delivered through VA facilities, VCCP community care networks, or other statutory authorities to provide care in the community. When authorizing care under VCAs, the Secretary is required to consider factors that would make the use of a VA facility or a community care network facility impracticable or inadvisable for the eligible veteran, such as a veteran's medical condition, the travel involved, the nature of the care or services required, or a combination of these factors.
The Review of Each VCA
This section requires the Secretary to review each VCA of material size that has been entered into for at least six months by the date of review. The reviews are required within the first two years after going into effect, and not less than every four years thereafter. For VCAs used for the purchase of extended care services in FY2019 and after, the material size will be defined as those exceeding $5 million annually.
Entities and Providers Eligible to Enter into VCAs
This section stipulates which entities and providers are eligible to enter into VCAs. These include (1) any provider of services that has enrolled and entered into a provider agreement under Medicare, and any physician or other supplier who has enrolled and entered into a participation agreement under Medicare; (2) any provider participating under a State Medicaid program; (3) an Aging and Disability Resource Center, an area agency on aging, or a state agency (as defined in Section 102 of the Older Americans Act of 1965); (4) a center for independent living (as defined in Section 702 of the Rehabilitation Act of 1973); and (5) any other entity or provider as determined by the Secretary.
Certification of Eligible VCA Entities and Providers
This section requires the Secretary to develop a certification process through the promulgation of regulations. The regulations at a minimum must (1) set deadlines for applications for certification; (2) provide standards for approval or denial of certification; (3) require the denial of certification if an entity or provider is excluded from participation in a federal health care program such as Medicare and Medicaid;37 and (4) establish procedures for screening providers or entities for the risk of fraud, waste, and abuse.
Reimbursement Rates Under VCAs
This section requires that rates paid by the VA for hospital care, medical services, and extended care services provided under VCAs be similar to rates paid under the VCCP. (Rates paid for care or services through VCCP may not exceed rates paid to providers under the Medicare program, set by CMS, including rates paid under Medicare for Durable Medical Equipment [DME].)
Requirements for Providers and Entities Entering into VCAs
This section requires the Secretary to promulgate regulations that define the terms under which providers and entities could enter into to VCAs with the VA. VCAs will be required to accept payments at the rates established through regulations, to accept payments in full, and to not hold a veteran liable for any care provided through a VCA authorization. In addition, entities are not allowed to bill a veteran's third-party health insurance provider for any care or service that is furnished or paid for by the VA, and entities are required to meet all other terms and conditions, including quality of care standards specified in regulations.
Discontinuation or Nonrenewal of a VCA
This section authorizes the Secretary to discontinue a VCA based on the following factors: (1) it is determined that the eligible entity or provider failed to comply with the requirements of the VCA; (2) it is determined that the eligible entity or provider is excluded from participation in a federal health care program; (3) it has been ascertained that the eligible entity or provider has been convicted of a felony or other serious offense, or the provider's continued participation would be detrimental to the best interests of veterans or the VA; or (4) it has been determined that it is reasonable to terminate the agreement based on the health care needs of the veteran.
Monitoring Quality of Care of VCAs
This section requires the Secretary to establish a system for monitoring the quality of care provided to veterans through VCAs, and to use such information when determining whether to renew VCAs.
Exclusion of VCAs from Federal Laws Governing Federal Contracts
This section stipulates that VCAs are not subject to competitive procedures associated with federal contracts for the acquisition of goods or services, and that VCAs are exempt from any provisions in law similar to those provisions that exempt Medicare providers. Entities that enter into VCAs would not be considered federal contractors or subcontractors. However, entities and providers that enter into VCAs with the VA are subject to all federal laws regarding integrity, ethics, and fraud, as well as all laws that protect against employment discrimination or that otherwise ensure equal employment opportunities.
Definition of Covered Individuals under VCAs38
This section defines those eligible to receive care through VCAs as any individual eligible for hospital care, medical services, or extended care services under any law administered by the VA.
Parity of Treatment
This section requires that care and services provided to veterans through VCAs should be similar and be subject to the same terms as care provided in a VA facility.
Section 103. Authorizing State Veterans Homes to Enter into VCAs
This section amends current law 38 U.S.C. §1745 to authorize the VA to enter into VCAs with State Veterans Homes. These VCAs, similar to Medicare providers, are exempt from certain federal contracting laws and are not subject to competitive procedures associated with federal contracts for the acquisition of goods or services, including any provisions in law similar to those provisions that exempt Medicare providers. State Veterans Homes that enter into VCAs are not considered federal contractors or subcontractors. However, State Veterans Homes that enter into VCAs with the VA are subject to all federal laws regarding integrity, ethics, and fraud, as well as laws that protect against employment discrimination or that otherwise ensure equal employment opportunities.
Section 104. Access Standards and Standards for Quality
This section amends current law to add two new sections (38 U.S.C. §1703B and §1703C) that require the Secretary to develop access and quality standards for furnishing hospital care, medical services, or extended care services to eligible veterans under the VCCP. In the following paragraphs, this section means the newly amended Section 1703B and Section 1703C and their respective subdivisions.
Access Standards
This section requires the Secretary to establish access standards for hospital care, medical services, and extended care services furnished by the VA and health care providers under the VCCP. It also requires the Secretary to ensure that the access standards established by the VA are clear, useful, and timely so that veterans, employees of the VA, and health providers in the VCCP have relevant comparative information upon which to make informed and responsible decisions. It also requires the Secretary to consult DOD, HHS, CMS, private sector entities, and other nongovernmental entities when establishing access standards. The Secretary is required to submit a report detailing the access standards to SVAC, HVAC, SAC, and HAC no later than 270 days after enactment. Prior to this, the Secretary is required to provide the first update no later than 120 days after enactment. No later than 540 days after the Secretary implements access standards, the Secretary is required to submit a report to SVAC, HVAC, SAC, and HAC detailing the implementation. The Secretary is also required to review the access standards on a periodic basis. The first review is required three years after the access standards are first established, and not less than every three years thereafter. It requires the Secretary to publish the established access standards in the Federal Register and on the VA website. This section stipulates that an eligible veteran could contact the VA at any time and request care through the VCCP, provided that a VA facility is unable to provide care or services based on access standards established by the VA.
Standards for Quality
This section requires the Secretary to establish standards of quality for hospital care, medical services, and extended care services provided by the VA and the VCCP, and requires the Secretary, when establishing standards for quality, to consider existing health quality measures in both the private and public health care systems in order to provide veterans relevant comparative information. The Secretary is required to consult with DOD, HHS, CMS, and other entities in developing these standards. The Secretary is required to submit a report detailing the standards for quality to SVAC, HVAC, SAC, and HAC no later than 270 days after enactment, and to provide periodic updates to SVAC, HVAC, SAC, and HAC prior to submitting the quality standards report. The first update is due 120 days after enactment. Moreover, no later than two years after the Secretary establishes quality standards, the Secretary is required to seek public comment and make any changes to quality measures.
Section 105. Access to Walk-In Care
This section amends current law to add a new 38 U.S.C. §1725A, which requires the Secretary to develop procedures to allow certain veterans to access walk-in care through community providers. All veterans enrolled in the VA health care system, and who have received VA care or services within 24 months prior to accessing a walk-in care clinic, are eligible. Both requirements must be satisfied for eligibility under this provision. Walk-in clinics that have entered into contracts or other agreements with the VA, including FQHCs, are eligible to participate in the walk-in care clinic program. Under this section, walk-in care means nonemergent care provided by qualifying non-VA providers or entities that furnish episodic care and not longitudinal management of conditions, and as defined by the Secretary in regulations.
Copayments
This section requires veterans to pay certain copayments when receiving care through a walk-in clinic or facility. If a veteran is required to pay a copayment for care at a VA facility, then the veteran may be required to pay a copayment when accessing walk-in care. If a veteran is not required to pay a copayment at a VA facility, then the first two visits in a calendar year will be free, and any additional visits after the first two visits may require copayments, as determined by the Secretary in regulations. If a veteran is required to pay a copayment for care at a VA facility, then the veteran would be required to pay the same regular copayment amount for the first two walk-in care visits in a calendar year. For any additional visits, a higher copayment amount, as determined by the Secretary in regulations, may be required.
Effective Date
The Secretary is required to publish regulations no later than one year after the date of enactment, and the effective date for walk-in care is the date when the final regulations pertaining to walk-in care take effect.
Section 106. Strategy Regarding the VA High-Performing Integrated Health Care Network.
This section amends current law to add a new 38 U.S.C. §7330C, which requires the Secretary to conduct a quadrennial market area assessments regarding VHA health care services. The assessment must assess the demand for VA health care; the VA's health care capacity; the capacity of VCCP providers; and the capacity of academic affiliates and other federal partners that provide health care to veterans, among other factors. The Secretary is required to use this assessment data when developing the President's annual budget request to Congress. This section requires the VA to submit the quadrennial market area assessments to SVAC, HVAC, SAC, and HAC.
Strategic Plan to Meet Health Care Demand
This section requires the Secretary to submit to SVAC, HVAC, SAC, and HAC a strategic plan that provides a four-year forecast of (1) the demand for VA health care, (2) the health care at each VAMC, and (3) the health care capacity to be provided through community care providers. The first plan is required one year after the enactment, and then once every four years.
Section 107. Applicability of Directive of Office of Federal Contract Compliance Programs
This section stipulates that the Office of Federal Contract Compliance Programs' (OFCCP) moratorium, which is currently applicable to all health care entities that participate in the TRICARE program as subcontractors under a prime contract between DOD and the TRICARE Management Activity, will be applicable in a similar manner to VCAs throughout the duration of the moratorium.39
Section 108. Prevention of Certain Health Care Providers from Providing Non-VA Health Care Services to Veterans
This section requires the Secretary to deny and revoke the eligibility of certain previous VA health care providers from providing health care services to veterans in the community. Such providers include those who have been removed from VA employment due to conduct that violated VA policies pertaining to the safe delivery of health care to veterans, or those who violated their medical licensing requirements and lost their medical license to practice. This section stipulates that no later than two years after enactment, the GAO must submit a report to Congress regarding the Secretary's implementation of this provision.
Section 109. Remediation of Medical Service Lines
This section amends current law to add a new 38 U.S.C. §1706A, which requires the Secretary to take steps to improve a medical service line that fails to meet the quality standards established by the Secretary. These steps include, among others things, increasing personnel; utilizing special hiring incentives, such as the Education Debt Reduction Program (EDRP) and recruitment, relocation, and retention incentives; utilizing direct hiring authority; providing improved training for staff; purchasing improved equipment; and making structural modifications to the VAMC. This section requires the Secretary to submit an annual report to Congress analyzing the remediation actions taken by the Secretary to improve the VA medical service line.
Section 111. Prompt Payment to Providers
This section amends current law to add a new 38 U.S.C. §1703D, which delineates prompt payment standards that the Secretary is required to follow for care provided to eligible veterans in the community. This section requires the Secretary to pay health care providers and entities for care furnished to veterans within 45 calendar days of receiving a clean paper claim, or within 30 calendar days of receiving a clean electronic claim. In addition, if the Secretary denies a paper claim, the Secretary must within 45 calendar days notify the entity regarding the reasons for denial and request additional information to process the claim. If an electronic claim is denied, the Secretary has 30 days to notify an entity and request additional information.
Submittal of Claims by Health Care Entities and Providers
This section requires a community health care provider or entity to submit a claim for payment to the VA no later than 180 days after the date in which care or services were provided to an eligible veteran.
Fraudulent Claims
This section stipulates that penalties and civil action applicable to false or fraudulent claims for payment or approval as delineated in 31 U.S.C. §§3729-3733 will be applicable in the same manner to entities and providers submitting false or fraudulent claims to the Secretary.
Overdue Claims
This section stipulates that any claim that has not been denied by the Secretary and for which payment is pending for more than 45 calendar days following the receipt of a clean paper claim, or more than 30 calendar days of receiving a clean electronic claim, will be deemed an overdue claim. Such overdue claims may be subject to the Prompt Payment Act (31 U.S.C. Chapter 39) requirements.
Overpayment40
This section stipulates that the Secretary may deduct overpayments to a health care provider or entity after reasonable steps have been taken to resolve the dispute. The Secretary may also use other means as authorized by federal law to correct or recover overpayments.
Information and Documentation Required
This section requires the Secretary to provide all relevant documentation to community health care providers and entities in order for them to generate clean claims.
Processing of Claims
The sections authorizes the Secretary to contract with the entity contracted to develop the VCCP network, or another private medical claims processor, to process community care medical claims.
Report on Encounter Data System
This section requires the Secretary to submit a report to SVAC, SAC, HVAC, and HAC on the feasibility and advisability of adopting a funding mechanism similar to other federal agencies that use a fiscal intermediary (a private insurance company) to serve as the federal government's agents in the administration of a health care program, including the payment of medical claims. This report is due no later than 90 days after enactment.
Section 112. Authority to Pay for Authorized Care Not Subject to an Agreement
This section amends current law to add a new U.S.C. §8159, which authorizes the Secretary to compensate for care provided to a veteran, even if the provider or entity does not have a contract or agreement with the VA. The Secretary is required take reasonable steps to enter into a contract or other arrangement with such an entity or provider so that future care provided to a veteran will be subject to an agreement, contract, or other reimbursable arrangement.
Section 113. Improvement of Authority to Recover the Cost of Services Furnished for Nonservice-Connected Disabilities
This section amends current law 38 U.S.C. §1729, which authorizes the Secretary to recover the cost of care for nonservice-connected conditions of veterans, and expands it to include care furnished by the VA to nonveterans requiring emergency services as well. It also authorizes the Secretary to seek collections in the event that the VA pays for care, rather than just furnishes it. This section also authorizes the Secretary to recover the cost of care of a nonservice-connected disability incurred by an individual who is entitled to care, or payment for the expenses of care, under a private health insurance plan.
Section 114. Processing of Claims for Reimbursement Through Electronic Interface
This section authorizes the Secretary to enter into an agreement with a third party to process medical claims using an electronic method.
Section 121. Education Program on Health Care Options
This section requires the Secretary to develop and conduct an education program to teach veterans about their health care options through the VA health care system, as well as VCCP eligibility criteria and any financial obligations they may have for their nonservice-connected care. It also requires that veterans be taught about the interaction between Medicare, Medicaid, TRICARE, tribal health programs, and VA health care.
Section 122. Training Program for Administration of Non-VA Health Care
This section requires the Secretary to develop and implement a training program to educate VA employees and contractors about VCCP, reimbursement for non-VA community emergency room services, and safe opioid prescription management, and how to administer these programs. This section also requires the Secretary to develop a method to evaluate the training program, and to submit a report to Congress each year regarding the findings from the most recent evaluation.
Section 123. Continuing Medical Education for Non-VA Medical Professionals
This section requires the Secretary to establish a continuing medical education program to provide education material to non-VA medical professionals. These education materials must include, among other things, information on identifying and treating mental and physical conditions of veterans, as well as the VA health care system. The materials provided to non-VA community care providers must be the same as those provided to VA health care providers. The Secretary is required to determine the curriculum of the program and the credit hour requirements, to develop a method to evaluate the continuing medical education program, and to provide a report to Congress about its effectiveness. A non-VA medical professional is defined in this section as "any individual who is licensed by an appropriate medical authority in the United States and is in good standing, is not an employee of the Department of Veterans Affairs, and provides care to veterans or family members of veterans under the laws administered by the Secretary of Veterans Affairs."
Section 131. Establishment of Processes to Ensure Safe Opioid Prescribing Practices by Non-VA Health Care Providers
This section requires the Secretary to ensure that all non-VA, nonfederal community providers are knowledgeable about opioid-prescribing practices described in the "Opioid Safety Initiative of the Department of Veterans Affairs." It further requires the Secretary to create a process to ensure that VA, non-VA, and nonfederal community providers share all medication and medical history of an eligible veteran. The VA is responsible for monitoring an eligible veteran's prescriptions, as described in the "Opioid Safety Initiative of the Department of Veterans Affairs."
Section 132. Improving Information Sharing with Community Providers
This section amends current law 38 U.S.C. §7332 regarding the confidentiality of certain medical records and adds a new subparagraph. This amended section authorizes the Secretary to share a veteran's confidential VA medical records with non-VA entities, including private entities and other federal agencies, for the purposes of providing health care, as well as with third-party insurance providers, for the purposes of recovering charges for care provided to a veteran with a nonservice-connected condition.
Section 133. Competency Standards for Non-VA Health Care Providers
Establishment of Standards and Requirements
This section requires the Secretary to establish standards and requirements for non-VA community providers to follow when providing care to eligible veterans. Specifically, these standards and requirements must focus on clinical areas for which the VA has special expertise, including post-traumatic stress disorder, military sexual trauma-related conditions, and traumatic brain injuries.
Condition for Eligibility to Furnish Care
Each non-VA community provider must meet the standards and training requirements specified by the Secretary before providing care to an eligible veteran in the clinical areas for which the VA has special expertise, including post-traumatic stress disorder, military sexual trauma-related conditions, and traumatic brain injuries.
Effective Date
This section will take effect one year after the date of the enactment.
Section 134. VA Participation in National Network of State-Based Prescription Drug-Monitoring Programs41
This section amends current law to add a new 38 U.S.C. §1730B. It requires the VA to enter into an agreement with a national network of prescription drug-monitoring programs (PDMPs) or any state or regional prescription drug-monitoring program, to allow licensed VA health care providers to query controlled substance prescriptions (21 U.S.C. §802(6)) written in participating states or regions. It requires VA health care providers practicing in states that do not have a PDMP to join the nearest state or regional PDMP.
Section 141. Plans for Use of Supplemental Appropriations
Whenever the Secretary requests from Congress supplemental appropriations or any other type of appropriation outside the annual congressional appropriations process, this section requires the Secretary to submit to Congress a justification detailing how the Secretary intends to use the requested appropriation and the expected duration of the supplemental appropriations.
Section 142. Veterans Choice Fund Flexibility
This section authorizes the Secretary, beginning on March 1, 2019, to use the remaining funds in the VCF for care in the community programs provided at non-VA facilities. However, the Secretary is prohibited from using the remaining VCF funds for VCCP.
Section 143. Sunset of Veterans Choice Program
This section amends VACAA and stipulates that the Secretary may not authorize care under the VCP program one year after the date of enactment (i.e., on June 6, 2019).
Subtitle B: Improving VA Health Care Delivery
In general, VA providers are able to practice across state lines in VA health care facilities with clinical privileging and a single, unrestricted, active state license.42 However, these providers cannot practice in non-VA health care facilities located in states where they are not licensed. For that reason, according to the VA, some VA providers were concerned that their state licensing boards might take action against their licenses if they provided telehealth services in non-VA health care facilities in states where they were not licensed.43 To address this issue, on May 11, 2018, the VA finalized a rule to exempt its providers that deliver care via telemedicine from certain state licensing laws and regulations.44 The VA's final rule became effective on June 11, 2018. The passage of the VA MISSION Act codified the core elements of VA's final rule in statute. The rule provides the details of how VA will implement the provisions contained in the new law.
Section 151. Licensure of Health Care Professionals of the VA Providing Treatment Via Telemedicine
This section amends current law to add a new 38 U.S.C. §1730B, which removes all geographical barriers to telemedicine, therefore allowing a telemedicine episode of care to be delivered without regard to where a veteran patient and VA provider are located within the United States and U.S. territories, and without regard to whether the veteran patient is located in a non-VA health care facility.45 It also protects VA providers against possible liability issues stemming from state licensure laws by prohibiting states from denying or revoking the licenses, registrations, or certifications of VA providers that practice under this authority.
This section also requires the Secretary, not later than one year after enactment, to submit an annual report to Congress outlining the effectiveness of the agency's use of telemedicine. The report must contain six elements: (1) incurred savings; (2) veteran patients' satisfaction in receiving telemedicine; (3) VA providers' satisfaction in providing telemedicine; (4) the types of telemedicine services delivered; (5) the number of telemedicine episodes of care delivered, by medical facility; and (6) outcome measurements, such as accessibility to and the frequency of use of telemedicine services by veteran patients.
Section 152. Authority for the VA Center for Innovation for Care and Payment
This section amends current law to add a new 38 U.S.C. §1703E, which establishes within the VA a Center for Innovation for Care and Payment. The Secretary may implement appropriate pilot programs to develop innovative approaches to testing payment and service delivery models, with the goal of reducing expenditures and enhancing the quality of care for veterans. However, the Secretary is prohibited from testing payment and service delivery models that would allow the VA to bill or recover charges from Medicare, Medicaid, or TRICARE for health care services provided to veterans eligible under those programs. In implementing this section, the Secretary may waive certain requirements. However, the Secretary is required to notify Congress before waiving such requirements.
Section 153. Authority for Operations on Live Donors for the Purposes of Conducting Transplant Procedures for Veterans
This section amends current law to add a new 38 U.S.C. §1788, which, subject to the availability of appropriations, requires the Secretary to furnish to any live donor, regardless of whether the donor is a veteran, any care or services that may be required in connection with such procedure before and after conducting the transplant procedure for an eligible veteran. The Secretary could provide for the operation on a live donor and furnish to the live donor the care and services at a VA or Non-VA facility.
Subtitle C: Family Caregivers
In recognition of the significant role that family caregivers play in providing personal care services and other supports to veterans, the Caregivers and Veterans Omnibus Health Services Act of 2010 (P.L. 111-163) was signed into law on May 5, 2010. The law requires the Secretary to establish the following two programs:
- Program of General Caregiver Support Services, which includes caregiver programs for veterans of all eras.
- Program of Comprehensive Assistance for Family Caregivers (Comprehensive Care Program), which provides additional supports and services, including financial compensation in the form of a caregiver stipend, to family caregivers of eligible veterans or servicemembers seriously injured in the line of duty on or after September 11, 2001 (post-9/11 veterans).
Subtitle C expands the VA's Comprehensive Care Program over time to include veterans of all eras (pre-9/11 veterans) and makes certain modifications to the services and assistance to family caregivers in such program. These provisions also require the VA to implement an information technology (IT) system that supports the Comprehensive Care Program and to amend the requirements for VA's annual evaluation report.
Section 161. Expansion of Family Caregiver Program of the VA
Eligibility
This section amends 38 U.S.C. §1720G(a)(2) to expand eligibility for the Comprehensive Caregiver Program to pre-9/11 veterans, beginning on the date when the Secretary submits to Congress the certification that the VA has fully implemented the IT system (described in Section 162), herein referred to as the certification date. Beginning on the certification date, the Comprehensive Caregiver Program is extended over a two-year period to pre-9/11 veterans who have a serious injury incurred or aggravated in the line of duty in the active military, naval, or air service on or before May 7, 1975. Two years after the certification date, the Comprehensive Care Program is extended to all pre-9/11 veterans, covering veterans of all eras. It requires the Secretary, no later than 30 days after the date the Secretary submits to Congress the above certification, to publish the certification date in the Federal Register.
It also amends 38 U.S.C. §1720G(a)(2) to expand the eligibility criteria for the Comprehensive Caregiver Program to include those veterans in need of personal care services because of a need for regular or extensive instruction or supervision, without which the ability of the veteran to function in daily life would be seriously impaired, among other existing criteria.
Caregiver Assistance
This section amends 38 U.S.C. §1720G(a)(3) to expand the types of assistance available to family caregivers under the Comprehensive Care Program to include financial planning services and legal services relating to the needs of injured veterans and their caregivers. It further amends this subsection regarding the monthly stipend determination to specify that in determining the amount and degree of personal care services provided to an eligible veteran whose need is based on a need for supervision or protection, as specified, or regular instruction or supervision, as specified, the determination must take into account (1) the assessment by the family caregiver; (2) the extent to which the veteran can function safely and independently without supervision, protection, or instruction; and (3) the amount of time required for the family caregiver to provide supervision, protection, or instruction.
It also adds new language under 38 U.S.C. §1720G(a)(3) that in providing instruction, preparation, and training to each approved family caregiver, the Secretary is required to periodically evaluate the needs of the eligible veteran and the skills of the family caregiver to determine if additional support is necessary. It amends 38 U.S.C. §1720(a)(5) to require the Secretary to evaluate each application submitted jointly by an eligible veteran in collaboration with the primary care team for the eligible veteran to the maximum extent practicable.
It further adds a new paragraph under 38 U.S.C. §1720(a) that in providing assistance to family caregivers of eligible veterans, the Secretary may enter into contracts or agreements with specified entities to provide family caregivers such assistance. The Secretary is required to provide such assistance only if it is reasonably accessible to the family caregiver and is substantially equivalent or better in quality to similar services provided by the VA. It authorizes the Secretary to provide fair compensation to federal agencies, states, and other entities that provide such assistance.
It amends the definition of personal care services under 38 U.S.C. §1720(d)(4) to include services that provide the veteran with (1) supervision or protection based on symptoms or residuals of neurological or other impairment or injury, and (2) regular or extensive instruction or supervision without which the ability of the veteran to function in daily life would be seriously impaired.
Section 162. Implementation of Information Technology System of the VA to Assess and Improve the Family Caregiver Program
This section requires the Secretary to implement an IT system, no later than October 1, 2018, with certain specified elements that fully supports the Comprehensive Caregiver Program and allows for data assessment and program monitoring. No later than 180 days after implementing the IT system, the Secretary is required, through the Under Secretary for Health, to conduct an assessment of how key aspects of the Comprehensive Caregiver Program are structured and carried out using data from the IT system and any other relevant data. The Secretary is required to use the IT system to monitor and assess program workload, and to implement certain modifications necessary to ensure program functioning and timeliness of services.
It also requires the Secretary, no later than 90 days after enactment, to submit an initial report to the SVAC, HVAC, and GAO on the status of the planning, development, and deployment of the IT system. The initial report must include an assessment of the needs of family caregivers of veterans eligible for the Comprehensive Program solely due to a serious injury incurred or aggravated in the line of duty in the active military, naval, or air service before September 11, 2001; the resource needs for including such family caregivers; and any changes necessary to ensure successful program expansion. The GAO is required to review the initial report and notify SVAC and HVAC with respect to the progress of the Secretary in fully implementing the required IT system, as well implementation of a process to monitor, assess, and modify the program as necessary. No later than October 1, 2019, the Secretary is required to submit a final report to SVAC, HVAC, and the GAO on system implementation, including program monitoring, assessment, and modification, as specified.
Section 163. Modification to Annual Evaluation Report on Caregiver Program of the VA
This section amends 38 U.S.C. §1720G note to add certain reporting requirements to VA's submission of the annual evaluation report to the SVAC and HVAC regarding program implementation. With respect to both caregiver programs, it requires the annual evaluation report to describe any barriers to accessing and receiving care and services under such programs. With respect to the Comprehensive Caregiver Program, it adds new reporting language to evaluate the sufficiency and consistency of the training provided to family caregivers under such programs.
Title II: VA Asset and Infrastructure Review
The VHA operates in approximately 5,670 buildings and another 1,648 leased facilities.46 The last major comprehensive review of VA real property and medical facilities throughout the country was done under the Capital Asset Realignment for Enhanced Services (CARES) program. In October 2000, the VA established the CARES program with the goal of evaluating the projected health care needs of veterans over the next 20 years and of realigning VA's infrastructure to better meet those needs. In August 2003, VA's then-Undersecretary for Health issued a preliminary Draft National CARES Plan (DNCP). The DNCP, among other things, recommended that seven VA health care facilities close and that duplicative clinical and administrative services delivered at over 30 other VHA facilities be eliminated. The sites slated to be closed were in the following locations: Canandaigua, NY; Pittsburgh, PA (Highland Drive Division); Lexington, KY (Leestown Division); Cleveland, OH (Brecksville Unit); Gulfport, MS; Waco, TX; and Livermore, CA. Patients currently receiving services at these VHA facilities would have been provided care at other nearby sites. The DNCP recommended that new major medical facilities be built in Las Vegas, NV, and East Central, FL. Furthermore, the DNCP recommended significant infrastructure upgrades at numerous sites including, at or near locations where the VA proposed to close facilities. In addition, the draft plan called for the establishment of 48 new high-priority Community Based Outpatient Clinics (CBOCs).
Following the release of the DNCP, the then-VA Secretary Anthony Principi appointed a 16-member independent commission to study the draft plan. The commission was composed of individuals from a wide variety of backgrounds outside of the federal government. The CARES Commission developed and applied six factors in the review of each proposal in the DNCP: (1) impact on veterans' access to health care, (2) impact on health care quality, (3) veteran and stakeholder views, (4) economic impact on the community, (5) impact on VA missions and goals, and (6) cost to the government. The commission conducted 38 public hearings and 81 site visits throughout 2003 and submitted its recommendations to the Secretary in February 2004. After reviewing the recommendations, the then Secretary announced the final details of the CARES plan in May 2004 (Secretary's CARES Decision). The final plan called for consolidating several facilities, as well as building new hospitals in Orlando and Las Vegas; adding 156 new CBOCs, four new spinal cord injury centers, and two blind rehabilitation centers; and expanding mental health outpatient services nationwide. However, critics of the CARES plan contended that closures were considered without assessing what kind of facilities would be needed for long-term care and mental health care in the future. Also, some believed that the CARES plan did not focus enough on future nursing home needs, would leave the VA short of beds in a few decades, and, as a result, would leave the VA with no choice but to privatize some parts of the health care system. Moreover, some veterans' groups believed that CARES was only about closing "surplus" hospitals and did not believe that CARES would result in the building of new and modern facilities. Finally, the closure of some VA medical facilities raised serious concern among some Members of Congress who felt that they had little control over the CARES process.47
The Independent Assessment required by Section 201 of VACAA found that
[c]urrent facilities, whether they have been maintained adequately or not, often do not match current models of care. The overwhelming majority of VHA hospitals were designed when care was focused more heavily around inpatient hospital treatments. Over the past eight years, Veteran inpatient bed days of care have declined nearly ten percent while outpatient clinic workload has increased more than 40 percent. Space for outpatient care is typically housed in converted inpatient spaces or VHA's growing number of clinics. As a result, VHA's capital needs fall into a broad range of categories, including ensuring adequate facility condition, providing sufficient and appropriate space for Veteran care, and upgrading infrastructure. As facilities age further and care continues to shift to the outpatient setting, the size of the capital need could continue to grow.48
Furthermore, the Commission on Care was established by VACAA "to examine the access of veterans to health care from the Department of Veterans Affairs and strategically examine how best to organize the [VHA], locate health resources, and deliver health care to veterans."49 In its final report, it recommended that the VA "develop and implement a robust strategy for meeting and managing VHA 's facility and capital asset needs."50
Within this context, the HVAC began to examine VA's capital asset program in the summer of 2017. At a hearing held on July 12, 2017, the then-VA Secretary who was involved in the CARES plan testified that "under CARES there was no requirement for Congress to adopt or reject the commission's final recommendations as a package. As a result, recommendations for some needed new hospitals and outpatient clinics were accepted. Most of those to change, realign, or maybe close the mission of other facilities were rejected."51
Based on input and recommendations from various stakeholders, on November 3, 2017, the VA Asset and Infrastructure Review Act of 2017 (H.R. 4243) was introduced; it was ordered reported on November 8 (without a written report). Provisions from H.R. 4243 were then incorporated as Title II of the VA MISSION Act.
Subtitle A: Asset and Infrastructure Review
This title establishes a process for realigning and modernizing facilities of the VHA. Under this process, the VA will develop criteria for selecting VHA facilities to dispose of, modernize, or acquire, so as to better meet the health care needs of veterans. The VA must then create a list of recommendations based on those criteria and submit it to a newly created Asset Infrastructure Review Commission (the Commission). This nine-member commission reviews the VA's recommendations but may not alter them, unless it determines that one or more recommendations are inconsistent with the criteria. The Commission submits the list of recommendations to the President, who either approves the list in its entirety or sends it back to the Commission with the reasons for disapproval. The Commission shall take into account the reasons for disapproval and submit a second report to the President with recommendations for realignment and modernization of VHA facilities. The President may approve or disapprove of the revised list. If the President approves of the original or revised list, then VA must begin implementation of the recommendations within three years, unless Congress passes a joint resolution of disapproval, in which case the process terminates.
Section 201. Short Title
This section provides the title as the "VA Asset and Infrastructure Review Act of 2018."
Section 202. The Commission
Establishment
This section establishes an independent commission to be known as the "Asset and Infrastructure Commission" (the Commission).
Duties
This section requires the Commission to carry out the duties specified for it in this subtitle.
Appointment
This section establishes a nine-member Asset and Infrastructure Review Commission. All nine members are to be appointed by the President, with the advice and consent of the Senate. The President is required to consult with House and Senate leadership, along with congressionally chartered, membership-based veterans organizations (VSOs), when selecting individuals to nominate to the Commission. The President shall designate one nominee to serve as Chair of the Commission and one nominee to serve as Vice Chair.
In nominating individuals, the President shall ensure that the Commission adequately represents the current demographics of veterans. In addition, the Commission must include at least one member with experience working for a private integrated health care system with annual gross revenues of more than $50 million; at least one member with experience with capital asset management for the federal government and who is familiar with trades related to building and real property; and at least three members who represent congressionally chartered, membership-based VSOs.
Nominations must be submitted to the Senate no later than May 31, 2021.
Meetings
The Commission shall meet only during calendar years 2022 and 2023, and all of its proceedings are required to be open to the public.
Vacancies
A vacancy shall be filled in the same manner as the original appointment, but the individual appointed shall serve only for the unexpired portion of the term for which the individual's predecessor was appointed.
Pay
Members of the Commission shall serve without pay. Members who are officers or employees of the United States shall serve without compensation in addition to that received for serving as officers or employees of the United States.
Director and Staff
The Commission shall appoint a Director who has not served as an employee of the Department of Veterans Affairs in the one-year period preceding the date of such appointment, and who is not otherwise barred or prohibited from serving as Director under federal ethics laws and regulations. The Director shall be paid at the rate of basic pay established for Level IV of the Executive Schedule.
The Director may, with the approval of the Commission, appoint and fix the pay of additional personnel. Not more than two-thirds of the personnel employed by or detailed to the Commission may be on detail from the VA. A person may not be detailed from the VA if, within the previous six months, that person participated substantially in the development of recommendations regarding VHA facilities. The head of any federal department or agency may provide detailees to the Commission.
Other Authority
To the extent funds are available, the Commission may (1) procure the temporary or intermittent services of experts or consultants, and (2) lease real property and acquire personal property, either on its own accord or in consultation with the General Services Administration (GSA).
Termination
The Commission shall terminate on December 31, 2023.
Prohibition Against Restricting Communications
No person may restrict a VA employee in communicating with the Commission, except for communications that are unlawful.
Section 203. Procedure for Making Recommendations
Selection Criteria
Not later than February 1, 2021, after consulting with VSOs, the Secretary is required to publish in the Federal Register and transmit to SVAC and HVAC the criteria the VA will use in making recommendations for the modernization and realignment of VHA facilities. There is a 90-day public comment period on the proposed criteria, and the VA must publish the final criteria in the Federal Register and transmit them to HVAC and SVAC no later than May 31, 2021.
Recommendation of the Secretary
The VA is required to consult with VSOs when developing its recommendations, which must be published in the Federal Register and transmitted to HVAC and SVAC no later than January 31, 2022. The VA must take into account the following factors when developing the list of recommendations:
- The degree to which any health care delivery or other site for providing services to veterans reflects the metrics of VA regarding market area health system planning.
- The provision of effective and efficient access to high-quality health care and services for veterans.
- The extent to which the real property that no longer meets the needs of the federal government could be reconfigured, repurposed, consolidated, realigned, exchanged, outleased, replaced, sold, or disposed.
- The need of VHA to acquire infrastructure or facilities that will be used for the provision of health care and services to veterans.
- The extent to which the operating and maintenance costs are reduced through consolidating, colocating, and reconfiguring space, and through realizing other operational efficiencies.
- The extent and timing of potential costs and savings, including the number of years such costs or savings will be incurred, beginning with the date of completion of the proposed recommendation.
- The extent to which the real property aligns with the VA's mission.
- The extent to which any action would affect other missions of the VA (including education, research, or emergency preparedness).
- Local stakeholder inputs and any factors identified through public field hearings.
- Commercial market assessments.
- The extent to which the VHA has appropriately staffed the medical facility, including determinations regarding insufficient resource allocation or deliberate understaffing.
- Any other such factors that the VA deems appropriate.
The VA is required to assess the capacity of each Veterans Integrated Service Network (VISN) and medical facility to furnish hospital care or medical services to veterans. Each assessment must
- identify gaps in furnishing care or services and how those gaps can be filled by (1) entering into contracts or agreements with network providers or other entities; (2) making changes in the way care and services are furnished, such as by extending hours of operation, adding personnel, or expanding space through the construction, leasing, or sharing of health care facilities; and (3) the building or realignment of VA resources or personnel;
- forecast the short-term and long-term demand in furnishing care and services and how such demand affects the need to use these providers;
- include a commercial health care market assessment of designated catchment areas conducted by a nongovernmental entity; and
- consider the ability of the federal government to retain a presence in an area otherwise devoid of commercial health care providers or from which such providers are at risk of leaving.
The VA is required to consult with VSOs and veterans served by each VISN and medical facility affected by an assessment and submit the assessments, along with the recommendations, to HVAC and SVAC. The VA must also
- submit a summary of the selection process that resulted in the recommendation for each facility, including a justification for each recommendation to HVAC and SVAC;
- consider all VHA facilities equally, without regard to whether the facility has been previously considered or proposed for reuse, closure, modernization, or realignment; and
- make all information used by the VA to prepare the recommendations available to the Commission and the Comptroller General.
Review and Recommendation by the Commission
The Commission must conduct public hearings on the VA's recommendations, including regions affected by a recommendation to close a facility. The Commission must also, to the greatest extent possible, hold hearings in regions affected by a recommendation to modernize or realign a facility. The witnesses at each public hearing must include a veteran identified by a local VSA who is enrolled in the VA health care system, and a local elected official.
The Commission must transmit its recommendations to the President, along with a review and analysis of the Commission's findings and conclusions, not later than January 31, 2023. The Commission's recommendations may deviate from the VA's recommendations only if the Commission
- determines that the VA deviated substantially from the final criteria;
- determines that the change is consistent with the final criteria;
- publishes a notice of the proposed change in the Federal Register not less than 45 days before transmitting its recommendations to the President; and
- conducts public hearings on the proposed change.
In addition, the Commission shall justify and explain in its report to the President any recommendations it makes that are different from the VA's recommendations. The Commission is also required to submit a copy of the report to HVAC and SVAC on the same date that it is transmitted to the President, and to promptly provide, upon request, to any Member of Congress, the information used by the Commission in making its recommendations.
Review by the President
Not later than February 15, 2023, the President is required to transmit to the Commission and to Congress a report containing the President's approval or disapproval of the Commission's recommendations. If the President approves all the recommendations of the Commission, the President must transmit a copy of the Commission's recommendations to Congress, together with a certificate of approval. If the President disapproves of the Commission's recommendations, in whole or in part, the President must transmit to the Commission and to Congress, not later than March 1, 2023, the reasons for that disapproval. The Commission, after considering the President's reasons for disapproval, must transmit to the President, not later than March 15, 2023, a report containing (1) the Commission's findings and conclusions based on a review and analysis of the President's reasons for disapproval, and (2) recommendations that the Commission determines are appropriate. If the President approves all the revised recommendations, the President must transmit a copy of those recommendations and a certificate of approval to Congress. If the President does not transmit an approval and certification to Congress for the initial or revised Commission recommendations by March 23, 2023, the process for modernizing or realigning VHA facilities shall terminate.
Section 204. Actions Regarding Infrastructure and Facilities of the VHA
This section requires the VA to begin implementing the recommendations not later than three years after the date on which the President transmits the report containing the recommendations to Congress. The VA may not carry out any facility modernization or realignment project identified in a report transmitted by the President if a joint resolution of disapproval is enacted in accordance with Section 207 of the act.
Section 205. Implementation
This section authorizes the VA to take any action necessary to implement the Commission's recommendation transmitted by the President (absent a congressional resolution of disapproval). It authorizes the Secretary to modernize or realign any facility—including through alteration, lease, acquisition, construction, or disposal of property—as well to carry out environmental mitigation, abatement, or restoration. The VA is authorized to reimburse other federal agencies for any work performed at the VA's request. In addition, the VA is required to carry out environmental abatement, mitigation, and restoration, as well as comply with historic preservation requirements, on any properties that exceed VA's needs as a result of modernization or realignment.
Management and Disposal of Property
To transfer or dispose of surplus real property or infrastructure located at any VHA facility to be modernized or realigned, the Secretary may exercise the authorities under subchapters I and II of 38 U.S.C. §81, or the GSA's delegated authorities.
Prior to disposing of any surplus real property, the VHA must consult with the governor of the state and the heads of the local governments concerned for the purpose of considering any plan for the use of the property by the local community. Similarly, the VHA must consult with the governor of the state and heads of local governments to ensure that the continued availability of any roads used for public access around a facility recommended for closure or realignment.
The Secretary may transfer the title of a VHA facility approved for closure or realignment to the redevelopment authority for the facility if the redevelopment authority agrees to lease a portion of the property to a federal department or agency. The lease shall be for a term not to exceed 50 years, but the term may be renewed or extended. The lease may not require rental payments by the United States.
The provisions of Section 120(h) of the Comprehensive Environmental Response, Compensation, and Liability Act of 1980 (42 U.S.C. §9620(h)) applies to any transfer of VA real property. Additionally, the McKinney-Vento Act (42 U.S.C. §11301 et seq.) applies to the closure of VA facilities.
Applicability of National Environmental Policy Act of 1969
The provisions of the National Environmental Policy Act of 1969 (42 U.S.C. §4321 et seq.) shall apply to VA actions under this subtitle only during the processes of (1) real property disposal and (2) relocating functions from a VHA facility being closed or realigned to another facility.
Waiver
This section allows the Secretary to close or realign any VHA facility without regard to (1) any provision of law restricting the use of funds for those purposes included in any appropriation or authorization act, and (2) the restrictions of 38 U.S.C. §8110.
Transfer Authority in Connection with Payment of Environmental Remediation Costs
The Secretary may enter into an agreement to transfer by deed a VHA facility to any person who agrees to perform all required environmental restoration, waste management, and environmental compliance activities. Such transfer may be made only if the costs of compliance activities otherwise to be paid by the Secretary are equal to or greater than the fair market value of the property to be transferred, or if compliance costs are lower than fair market value of the facility and the recipient of the transfer agrees to pay the difference.
Section 206. Department of Veterans Affairs Asset and Infrastructure Review Account
Establishment
This section establishes a VA Asset and Infrastructure Review Account, which is to be administered by the VA.
Credits to the Account
The account is authorized to receive appropriated funds and proceeds realized from lease, transfer, or disposal of any VHA property closed or realigned under this subtitle.
Use of Account
The VA may use the funds to carry out recommendations—including costs associated with the disposal and construction of facilities—and other purposes that the VA determines support the mission and operations of the department.
Consolidated Budget Justification Display for Account
The VA is required to establish a consolidated budget justification display that provides details on the credits to, and expenditures from, the account in the preceding fiscal year. The VA must provide this information to Congress in its budget submission.
Closure of Account; Treatment of Remaining Funds
The account shall be closed at the time and in the manner provided for appropriations accounts under 31 U.S.C. §1555, except the unobligated funds in the account shall be held by the Secretary of the Treasury until transferred by the VA Secretary after the final report on the account is received by SVAC and HVAC.
Section 207. Congressional Consideration of Commission Report
This section defines the expedited procedures for congressional consideration of the commission report. The procedures have the same force and effect as standing House and Senate rules and exempt the joint resolution of disapproval from many of the time-consuming steps and obstacles that apply to most measures Congress considers. Specifically, the procedure dictates when a joint resolution may be introduced, specifies its text, structures committee and floor consideration of the measure, prohibits amendments and other motions, and establishes an automatic "hook-up" of joint resolutions passed by both chambers. Significantly, because consideration is limited on the joint resolution of disapproval, a simple majority of the Senate may call up and reach a final vote on the measure without having to first assemble 60 votes to limit debate through the cloture process.52
Introduction and Referral
Ordinarily, Members of the House and Senate may introduce legislation at any time that their chamber is in session during the two-year Congress. Under the commission procedure, however, a qualifying joint resolution of disapproval must be submitted within a five-day period beginning on the date the President transmits a certified commission report to Congress.53 Joint disapproval resolutions may be introduced by any Member in his or her respective chamber. In the Senate, such resolutions are referred to the SVAC. A joint resolution submitted in the House is to be referred under the chamber's standing procedures, which would likely result in a referral to HVAC, but could also include referral to additional House committees. There is no limit to the number of disapproval resolutions that can be introduced; multiple disapproval resolutions aimed at the same commission report could be submitted. Notably, submission of a disapproval resolution is not mandatory. It is possible that no Member will submit a disapproval resolution during the five-day period, and if so, the Secretary would implement the commission recommendations at the conclusion of the 45-day layover period described above.54
Text of the Joint Resolution of Disapproval
Provisions in the act specify the text of the disapproval resolution. These provisions are meant to make it clear exactly which legislation is eligible to be considered under the expedited procedures. The joint resolution of disapproval may not contain a preamble.55 The title of the measure is to read: ''Joint resolution disapproving the recommendations of the VHA Asset and Infrastructure Review Commission.''56 The text of the joint resolution after the resolving clause is to read: ''that Congress disapproves the recommendations of the VHA Asset and Infrastructure Review Commission as submitted by the President on ___'' (with the appropriate date filled in the blank).57
Committee Action
With certain exceptions—for example, when time limits are placed by the Speaker on a House sequential referral of a bill58—Congress generally does not mandate that a committee act on a bill referred to it within a specified time frame or at all. The commission procedure, however, places deadlines on the House and Senate committees of referral to act and creates a mechanism to remove the joint resolution from committee if they do not. These expediting provisions are intended to make it impossible for a joint resolution of disapproval to be long delayed or blocked outright in committee.
As noted, upon introduction, a Senate joint resolution of disapproval is to be referred to the SVAC and a House joint resolution to the relevant House committees of jurisdiction. A committee may choose to mark up and report such a joint resolution, but it may not report amendments to it. If a House or Senate committee does not report a referred joint resolution of disapproval within 15 legislative days59 in the House or 15 session days60 in the Senate after the date of its introduction, the committee is automatically discharged from further consideration of the joint resolution, and the measure is placed directly on the chamber's appropriate calendar.61
Calling Up the Joint Resolution on the Floor
After the third legislative day following the day that each House committee of referral has reported a joint resolution of disapproval or been discharged from its further consideration, any Member may move to proceed to consider the measure on the House floor. All points of order are waived against the motion to proceed. The motion is not debatable and cannot be made if the House has already disposed of a motion to proceed to consider a joint resolution proposing to disapprove the same commission package of recommendations. This ensures that the House may only vote on one motion to consider a disapproval resolution (even if multiple such resolutions have been submitted or if the House has already declined to consider such a joint resolution). Should the motion to proceed be adopted, the House would immediately consider the joint resolution of disapproval. All points of order against the joint resolution and its consideration are waived, and a motion to reconsider the vote on the motion to proceed is not in order.
After the third session day following the day on which the SVAC has reported a joint resolution of disapproval or been discharged of its further consideration, it is in order for any Senator to move to consider the measure on the Senate floor. In the Senate, under most circumstances, a motion to proceed to the consideration of a measure is debatable. Under the commission procedure, however, the motion to proceed to the consideration of the joint resolution of disapproval is not debatable, and it may not be postponed. A motion to reconsider the vote on the motion to proceed is not in order. Unlike in the House, this motion to proceed can be made in the Senate even if an identical motion has previously been defeated. This provision serves as incentive for the chamber to get to a vote on the underlying joint resolution of disapproval; if a motion to proceed is defeated, supporters can simply reoffer it until it passes or force the chamber to expend time and energy disposing of repeated motions.
If the motion to proceed is adopted, the Senate will immediately consider the joint resolution. Once taken up, consideration of the joint resolution is "locked in," that is, the measure is to remain the unfinished business of the Senate until disposed of. All points of order against the resolution and its consideration are waived.
In the absence of a special rule dictating otherwise, the standing rules of the House of Representatives generally provide that measures are debated in the House under the one-hour rule.62 In the Senate, debate is usually unlimited, except by unanimous consent, by the invocation of cloture, or by some other special procedure, such as the statutory rules governing the consideration of budgetary legislation. In keeping with its "fast track" nature, floor consideration of a commission joint resolution of disapproval is limited in both houses. Debate in a chamber on the joint resolution, and all debatable motions and appeals connected with it, is limited to not more than two hours, equally divided in the House between a proponent and an opponent, and in the Senate between the majority and minority leaders or their designees. All debatable motions and appeals in relation to consideration of the resolution would fall under the two-hour time cap, and all appeals are to be decided without debate. A nondebatable motion to further limit debate is in order in the Senate.
The commission procedure limits Members' ability to delay consideration of a joint resolution of disapproval by barring amendments and motions that would ordinarily be permissible under the House and Senate standing rules. Amendments to the joint resolution, a motion to postpone its consideration, or motions to proceed to the consideration of other business are not permitted. A motion to recommit the joint resolution of disapproval is not in order in either chamber.63
Voting
It is extremely difficult from a parliamentary standpoint to avoid a final vote on a joint disapproval resolution once a chamber has decided to take it up. At the conclusion of debate, a chamber is to immediately vote on passage of the joint resolution of disapproval.64 A motion to reconsider the vote on passage of the measure in not permitted. As noted above, because debate is limited by the act, it is not necessary for the Senate to invoke cloture on the question of calling up or on reaching a final vote on the joint resolution; all votes under the procedure are simple majority votes.
Automatic Legislative "Hook-Up"
If, before voting upon its own disapproval resolution, either chamber receives a joint resolution passed by the other chamber, that engrossed joint resolution is not referred to committee. Instead, the second chamber may proceed to consider its own joint resolution, as laid out above, up until the point of final disposition, when the second chamber will lay it aside, take up the joint resolution received from the first chamber, and vote on it. This provision is included to avoid the need to expend time choosing whether ultimately to act upon the House or Senate joint resolution.
If the Senate does not introduce or consider its own joint resolution, a House joint resolution of disapproval is entitled to expedited floor procedures in the Senate. If, following passage of a joint resolution in the Senate, the Senate receives a companion measure from the House, the House measure is to be treated as nondebatable in the Senate.
Presidential Consideration and Subsequent Action
For a joint resolution of disapproval to become law, it must be signed by the President, enacted over his veto, or become law without his signature. In the event a disapproval resolution is subsequently vetoed by the President,65 a two-thirds vote in each chamber would then be required to override the veto. The commission procedure does not include expedited provisions governing House and Senate consideration of a joint resolution of disapproval vetoed by the President. Such a veto message would be considered pursuant to the normal procedures of each house.66
Either Chamber May Alter the Expedited Procedure
The fact that an expedited legislative procedure is contained in statute does not mean that another law must be enacted to alter its application. Article I, Section 5, of the Constitution gives each chamber of Congress the power to determine the rules of its proceedings; as a result, statutory expedited procedures such as those governing the Commission can (like all rules of the House or Senate) be set aside, altered, or amended by either chamber at any time. As several House Parliamentarians have observed, a chamber may "change or waive the rules governing its proceedings. This is so even with respect to rules enacted by statute."67 These changes can be accomplished in the House, for example, by the adoption of a special rule from the House Committee on Rules, by suspension of the rules, or by unanimous consent agreement. In fact, in most cases in which a measure is made privileged by statute, the House still brings the measure in question to the chamber floor under the terms of a special rule reported by the House Committee on Rules and adopted by the House. In the Senate, the statutory procedures could be waived or altered by unanimous consent or suspended entirely using the suspension of the rules procedure.
In a sense, then, the expedited procedures in the statute establish a default set of parliamentary ground rules for consideration of a disapproval resolution; these provisions can be tailored by either chamber to meet specific situations or for their convenience.
Section 208. Other Matters
Online Publication of Communications
The VA shall publish online any information transmitted or received by VA, the Commission, or the President regarding the act within 24 hours.
Continuation of Existing Construction Projects and Planning
The VA may not stop, due to implementation of approved recommendations, (1) VHA construction or lease projects, (2) long-term planning of VHA infrastructure, or (3) VHA budgetary processes.
Recommendation for Future Asset Reviews
The VA may, after consulting with VSOs, include in its budget submissions after the termination of the commission recommendations other capital asset realignment and management processes.
Section 209. Definitions
This section defines the following terms for this title:
Facility. Land, building, structure, or infrastructure under the jurisdiction of VA, under the control of VHA, and not under the control of GSA.
Infrastructure. Improvements to land other than buildings or structures.
Modernization. Any action required to align the form and function of VHA facility to the provision of modern health care. Includes construction purchase, lease, sharing, or closure. Also includes realignments, disposals, exchanges, and collaborations between VA and federal or nonfederal entities, including tribal organizations.
Realignment. Any action that changes the numbers or relocates services, functions, and personnel positions; disposals or exchanges between VA and other federal entities; and strategic collaborations between VA and nonfederal entities, including tribal organizations.
Redevelopment authority. The entity responsible for developing the redevelopment plan or directing implementation of it.
Redevelopment plan. A plan for the closure or realignment of a VHA facility that is agreed to by the local redevelopment authority and provides for the reuse of the real and personal property of the facility.
Subtitle B: Other Infrastructure Matters
Section 211. Improvement to Training of Construction Personnel
This section requires the VA to implement training and certification programs for construction and facilities management personnel, and for staff who award construction and maintenance contracts.
Section 212. Review of Enhanced Use Leases
This section requires the Office of Management and Budget to review all proposed VA-enhanced use leases to ensure they are compliant with federal law.
Section 213. Assessment of Health Care Furnished by the VA to Veterans Who Live in U.S. territories68
This section requires the VA to submit a report to Congress, within 270 days of enactment, that assesses the ability of the department to provide veterans in U.S. territories with hospital care, medical services, mental health services, geriatric services, and extended care. The report must also assess the feasibility of establishing a medical facility in any U.S. territory that does not already have such a facility. U.S. territories are defined as American Samoa, Guam, the Northern Mariana Islands, Puerto Rico, and the U.S. Virgin Islands.
Title III: Improvements to Recruitment of Health Care Professionals
This title aims to address VHA clinical workforce shortages by amending and creating new programs that provide scholarships, loan repayments, and bonuses to VA personnel in hard-to-recruit fields as determined by the Inspector General (IG), who is required to publish annual reports on staffing shortages.69 One provision amends the VA's Health Professional Scholarship Program (38 U.S.C. §7611)70 to prioritize recruiting physicians and to extend the program's authorization, which was set to terminate on December 31, 2019. Another three provisions amend the VA's Education Debt Reduction Program, which provides loan repayment to VHA clinical employees in hard-to-recruit and hard-to-retain specialties. One provision increases the annual and cumulative limits, the second makes new provider types eligible for the program, and the third adds Vet Centers to the locations where they can fulfill their service commitment. Other provisions create a new pilot program to recruit veterans into medical schools in exchange for their commitment to provide clinical care at the VHA, and to increase the amount of bonus payment that the VA can award in certain years.
Section 301. Designated Scholarships for Physicians and Dentists Under the VA Health Professional Scholarship Program
This section amends 38 U.S.C. §7612(b) to make a number of changes to the Health Professional Scholarships program. First, it requires the VA to ensure that of the scholarships awarded (under this subchapter), not less than 50% are awarded each year to individuals who are enrolled (or accepted for enrollment) in a training program in medicine or dentistry. This requirement will remain in effect until the Secretary determines that the staffing shortage of physicians and dentists is less than 500. Second, it specifies that if this requirement is met, the Secretary is required to ensure that the number of awards of Health Professional Scholarships made to individuals in training to become physicians and dentists is not less than 10% of the VHA staffing shortages in these professions. Third, it specifies that physicians and dentists who enter into such Scholarship Program agreements must serve as a full-time VHA employee for 18 months for each school year or part of school year that they received scholarship support. It specifies that the support received may range from two to four years of scholarship support and permits the Secretary to give preference to Veteran applicants when awarding scholarships. Finally, it requires the Secretary to provide information annually to medical and dental schools about the availability of this scholarship program.
This section also amends 38 U.S.C. §7617 regarding the situations in which a scholarship participant would be considered to have breached an agreement to add that physician scholarships participants who fail to successfully complete their post-graduate (i.e., residency) training are considered to have breached their agreement.
Finally, the section amends 38 U.S.C. §7619 to extend the authority for the Health Professional Scholarships program to December 31, 2033.
Section 302. Increase in Maximum Amount of Debt That May Be Reduced Under Education Debt Reduction Program (EDRP) of the VA
This section amends 38 U.S.C. §7683 to increase the maximum total and annual amounts that may be forgiven under the EDRP. The new maximum total is $200,000, and the new annual amount is $40,000. The section also requires the VA, within one year of enactment, to examine the demand for loan repayment through this program, the staffing needs of the VA, the total number of VHA vacancies whose applicants are eligible for the EDRP, and the overall U.S. demand for medical professionals, and to report these findings to SVAC and HVAC.
Section 303. Establishing the VA Specialty Education Loan Repayment Program
This provision creates new 38 U.S.C. §§7691-7697, which authorize the Secretary to create, as part of the VA's Educational Assistance Program, a new program called the "Department of Veterans Affairs Specialty Education Loan Repayment Program." The purpose of the new program is to assist—via an incentive program—in recruiting physicians who are practicing in certain hard-to-recruit medical specialties to work at the VHA. The provision specifies the program's eligibility, funding preferences, covered costs, total and annual maximum amount of payments, and service requirements, among other program elements. The provision makes conforming and technical amendments to Title 38 U.S.C. and requires that the Secretary, when determining whether to make awards through the newly authorized program, to consider the VHA's anticipated staffing needs two to six years in the future. It also requires the Secretary, when determining awarding preference, to assess whether a VA facility is considered underserved based on the criteria developed in Section 401 of the act, and specifies the VA's awarding deadlines and the steps it may take to publicize the new program.
Section 304. Veterans Healing Veterans Medical Access and Scholarship Program
The section requires the Secretary to establish a pilot program that provides funding for 18 eligible veterans who are enrolled in medical school, with two veterans enrolled at each eligible medical school. The section specifies that eligible veterans must have been discharged from the Armed Forces not more than 10 years before they apply to the program, and must not be entitled to other education benefits under Title 38 U.S.C. Chapters 30, 31, 32, 33, 34, or 35 or Title 10 U.S.C. Chapters 1606 or 1607. They must apply for admission for medical school beginning in 2019 in one of the covered medical schools71 and indicate that they would like to be considered for one of the school's two covered slots. They must also meet the school's minimum admission criteria and agree to fulfill a service commitment to the VA. Covered medical schools may opt to participate in this program. If they do so, they are required to reserve two seats in the 2019 entering class for eligible veterans with the highest admissions rankings for the applicant class.
The section specifies the expenses that the program covers for eligible veterans and the procedures to be followed if two or more eligible veterans do not apply for admission at one of the covered medical schools. In exchange for receiving support, eligible veterans are required to complete medical school while maintaining an acceptable level of academic standing, as determined by the Secretary; complete residency training leading to board eligibility in a specialty that is applicable to the VA, as determined by the Secretary; and obtain a medical license. Upon completing training, the eligible veteran must serve as a full-time clinical practice employee at the VA for four years.
The section specifies penalties for breaching an agreement. The section specifies that the provision does not prevent a covered medical school from accepting more than two eligible veterans for the 2019 entering class. It also requires a report evaluating the pilot program, including certain specified elements. The report is required to be submitted to Congress not later than December 31, 2020, and annually thereafter for the next three years.
Section 305. Bonuses for Recruitment, Relocation, and Retention
This section amends VACAA §705(a) to increase the aggregate amount of bonuses that can be paid to employees, from $230,000,000 to $250,000,000 for FY2017 and FY2018 and from $225,000,000 to $290,000,000 for FY2019 and FY2021, and specifies that in each of those years not less than $20,000,000 must be used for recruitment, relocation, and retention bonuses.
Section 306. Inclusion of Vet Center Employees in Education Debt Reduction Program (EDRP) of the VA
This section requires the Secretary to ensure that Vet Center clinical staff are eligible to participate in the VA's Education Debt Reduction Program established in 38 U.S.C. §§7681-7684. It also requires the Secretary to submit a report on the number of participants in the debt reduction program who work at Vet Centers to the HVAC and SVAC not later than one year after enactment.
Title IV: Heath Care in Underserved Areas
The provisions in this title aim to increase health services to veterans in underserved areas –– areas where there are access issues or shortages of health professionals. It does so by developing a process to designate VA facilities as underserved and reporting requirements around that process. It also includes two provisions that aim to address staffing issues at these underserved facilities: the first by developing mobile teams that can be deployed to provide clinical services at underserved facilities, and the second to establish a medical residency training program at certain VA and non-VA facilities, including facilities operated by the Indian Health Service (IHS) or an Indian Tribe or tribal organization.
Prior to enactment of the VA MISSION Act of 2018, the VA did not have a process to designate its facilities as underserved and thereby to direct resources to facilities with greater need. In contrast, the Department of Health and Human Services (HHS) designates facilities that serve the general population, Indian Tribes, or prisoners as being underserved if they meet certain criteria, including a low ratio of providers to population and high rates of certain health conditions.72 HHS uses this designation to direct resources, including loan repayment for providers and higher reimbursement rates in certain programs to facilities that have this designation. HHS does not designate whether VA-operated facilities are underserved.
The VA has a long-term historical role in supporting and directly training medical residents (among other types of health professionals). Generally, its support for medical residency training (called graduate medical education, or GME)73 is through partnerships with non-VA hospitals and medical schools that operate programs where residents spend a period of time training at a VA facility. Generally, the VA does not operate these programs, but it pays for resident training costs (including faculty support) during the time that a resident is at the VA.74 The VA has not paid for costs when a resident is training at non-VA facilities, because these costs are generally covered by other federal programs.75
The VACAA required an increase in the number of GME positions by up to 1,500 over a 10-year period, beginning July 1, 2015, through 2024, with an emphasis on primary care, mental health, and other specialties the VA Secretary deems appropriate. The VACAA also required that the expansion focus on creating new programs at VA facilities where there had not previously been GME training, and that the new positions be awarded for training in rural or otherwise underserved areas. As of September 2017, the VA had allocated about one-third of these new positions; it has not completed the expansion. Instead, the VA's objective is to complete the expansion by 2025.76
The VA, like other sources of GME support, tends to focus on hospital-based training that generally does not occur in rural areas. The GAO, among others, has raised a number of concerns about medical residency training, noting in particular that more training should occur in rural areas and outpatient settings.77 HHS, through the Teaching Health Center GME Program, does fund training in outpatient settings, particularly at federally qualified health centers (FQHCs), which are outpatient primary care based facilities that are required to be located in an underserved area or to serve an underserved population. The Teaching Health Center GME Program is approximately 1% of federal GME funding.78 The Choice GME expansion did prioritize training rural or underserved areas, but it did not require that training be in outpatient settings. Under a pilot program in this title, the VA is required to establish GME programs at community-based facilities, including those operated by an FQHC, IHS, or Indian Tribes, or at underserved VA facilities. Under the program, the VA would pay for costs associated with developing a program and would pay for residents' time when they are not in training at VA facilities.
Section 401. Development of Criteria for Designation of Certain Medical Facilities of the VA as Underserved Facilities and Plan to Address Problem of Underserved Facilities.
The section requires the Secretary, not later than 180 days after enactment, to develop criteria to designate certain medical centers, ambulatory care facilities, and CBOCs as underserved facilities. When developing this criteria, the Secretary is required to consider the following: (1) the ratio of veterans to VA health care providers standardized for the geographic area that surrounds the VA facility, including separate ratios for general practitioners and specialists; (2) the range of clinical specialties covered by providers in the geographic area; (3) whether the surrounding community is medically underserved; (4) the type, number, and age of open consults; (5) whether the facility is meeting the wait-time goals of the department; and (6) any other criteria developed by the Secretary to determine which facilities are not adequately serving veterans.
The section also requires the VISN directors, not less frequently than each year, to determine which facilities within their VISN meet the newly developed criteria as underserved facilities. The section further requires the Secretary to submit an annual plan to Congress to address the newly designated underserved facilities. The first plan is due not later than one year after enactment. The plan must include certain specified elements related to personnel, including the use of mobile deployment teams, special hiring incentives, direct hire authority, and improved training opportunities for facility staff.
Section 402. Pilot Program to Furnished Mobile Deployment Teams to Underserved Facilities
The section requires the Secretary to carry out a three-year pilot program that will furnish mobile deployment teams to underserved facilities. When furnishing these teams, the Secretary is required to consider a number of specified elements related to the staffing of these teams and program oversight. The Secretary is required to use the annual plans developed under Section 401 of the act to form mobile deployment teams that are composed of the medical personnel most needed by underserved facilities.
The section requires the Secretary to report to Congress, not later than one year after enactment, on the implementation of the pilot program. The section also requires the Secretary to submit a final report on the pilot program not later than the termination of the program that includes recommendations about the feasibility and advisability of extending and expanding the pilot program, including making the pilot program permanent.
Section 403. Pilot Program on Graduate Medical Education and Residency
This section requires the Secretary to establish a pilot program to create the medical residency positions authorized under the VACAA at covered facilities. Covered facilities are defined as a facility operated by the IHS or by Indian Tribes, an FQHC, a DOD facility, or another facility that the Secretary deems appropriate. To carry out the pilot program, the Secretary is authorized to enter into agreement with entities that operate a covered facility where the Secretary places medical residents. When selecting participating covered facilities, the Secretary is required to consider certain elements of the area where the facility is located, including the ratio of veterans to providers in the geographic area surrounding the facility, the specialty of providers in the surrounding geographic area, and whether the area is considered to be a HPSA by HHS, among others. During the pilot program, the Secretary is required to place no fewer than 100 residents in covered facilities operated by IHS, an Indian Tribe, or tribal organization, or at facilities located in areas that the Secretary has designated as underserved under Section 401 of the act.
Under the pilot program, the Secretary is authorized to pay resident stipends and benefits regardless of whether the resident has been assigned to a VA facility. In the event that a covered facility establishes a new residency program, the Secretary is required to reimburse the facility for associated costs, including curricula development, faculty salaries, faculty and resident recruitment, costs associated with the program becoming accredited, and resident educational expenses. The Secretary is required to report to Congress annually, beginning within one year of enactment, on multiple aspects of the pilot program. The section requires that the pilot program terminate on August 7, 2024.
Title V: Other Matters
This title aims to address broad topics within the VA. It requires the Secretary to submit an annual report on performance awards and bonuses awarded to certain high-level employees of the VA, including Regional Office Directors, VAMC Directors, VISN Directors, and other senior executives. It also amends current law and authorizes podiatrists with a doctor of podiatric medicine qualification to be appointed to any supervisory position similar to a physician with a doctor of medicine qualification. This title also requires the VA to publicize staffing and vacancy information on its website. It also amends current law and raises the dollar threshold for congressional authorization of a major medical facility project from $10 million to $20 million, and it authorizes the VA to carry out major medical facility projects, including the East Bay CBOC and the Central Valley Engineering and Logistics support facility. This title also establishes two pilot programs. One of the pilot programs involves adding peer specialists onto patient-aligned care teams (PACTs) within VAMCs. The other pilot program requires the Secretary to increase the use of medical scribes at VAMCs. The title also includes provisions postponing the VA Home Loan guarantee fee reductions on housing loans, thereby increasing some of the VA Home Loan guarantee fees that VA charges some veterans until 2028. It also extends until September 30, 2028, the $90 per month limit on a VA pension for certain veterans covered by Medicaid who receive nursing care in a Medicaid-approved nursing facility. These provisions are included as offsets for the costs of the VA MISSION Act. Lastly, it authorizes and appropriates $5.2 billion for VCF to continue VCP.
Section 501. Annual Report on Performance Awards and Bonuses Awarded to Certain High-Level Employees
This section amends current law to add a new 38 U.S.C. §726 that requires the Secretary to submit an annual report to SVAC, HVAC, SAC, and HAC on performance awards and bonuses awarded to certain high-level employees, including Regional Office Directors, VAMC Directors, VISN Directors, and other senior executives. The annual report must include, among other things, the amount of each award or bonus, the job title of the individual who obtained the award or bonus, and the location where the individual works.
Section 502. Role of Podiatrists in the VA
This section amends current law to add a new 38 U.S.C. §7413 that authorizes the Secretary to appoint a podiatrist with a doctor of podiatric medicine (DPM) qualification to any supervisory position in the VHA similar to allopathic physicians (MD's) and osteopathic physicians (DO's) appointed by the VHA. This section also requires the Secretary to establish standards to ensure that specialists appointed to supervisory positions within the VHA do not provide direct clinical oversight, such as peer review or practice evaluation, for providers of other clinical specialties. Lastly, this section amends current law (38 U.S.C. §7404(b)) and includes podiatrists within the VHA physician and dentist pay schedule.
Section 503. Definition of Major Medical Facility Project
This section amends current law 38 U.S.C. §8101(3) to define a major medical facility as
any facility or part thereof which is, or will be, under the jurisdiction of the Secretary, or as otherwise authorized by law, for the provision of health-care services (including hospital, outpatient clinic, nursing home, or domiciliary care or medical services), including any necessary building and auxiliary structure, garage, parking facility, mechanical equipment, trackage facilities leading thereto, abutting sidewalks, accommodations for attending personnel, and recreation facilities associated therewith.
It also amends current law 38 U.S.C. §8104(a) to increase the dollar threshold for congressional authorization of major medical facility projects from $10 million to $20 million. Any major medical facility project involving construction, alteration, or acquisition of a medical facility where the total expenditure is more than $20 million will require congressional authorization prior to appropriation of funds.
Section 504. Authorization of Certain Major Medical Facility Projects
This section authorizes the Secretary to carry out the following major medical facility projects in Livermore, CA. These include the construction of the new East Bay CBOC and all associated site work, utilities, parking, and landscaping; the construction of the Central Valley Engineering/Logistics support facility; and enhanced flood plain mitigation at the Central Valley and East Bay CBOCs. (Central Valley CBOC was authorized and funded in FY2016.) The Secretary is required to submit a report listing information about facility projects, including expenditures related to construction management and future amounts budgeted for the above projects, and it is required to do so no later than 90 days after the enactment. An amount not to exceed $117.3 million is authorized for these projects.
Section 505. VA Personnel Transparency
This section requires Secretary to publish on the VA website, no later than 90 days after enactment, the following information broken down by VAMC: the number of actually occupied (filled) positions, the number of accessions and separation actions processed during the quarter, the number of vacancies by occupation, and the percentage of new hires who were hired within the time-to-hire target of the Office of Personnel Management. This information must be updated quarterly on the VA's website. This section stipulates that the Secretary may withhold sensitive information, such as that relating to law enforcement and information security, among others. In addition, the Secretary is required to submit an annual report to Congress on steps the VA is taking to achieve full staffing capacity. Lastly, on a semiannual basis, the OIG is required to review the website and provide recommendations.
Section 506. Program on Establishment of Peer Specialists in Patient-Aligned Care Team Settings Within VAMCs
This section requires the Secretary to establish a program to assign not less than two peer specialists to patient-aligned care teams in the VA.79 The purpose of this program is to promote services in relation to mental health, substance use treatment, and behavioral health in a primary care setting. The Secretary is required to carry out this program in at least 15 VAMCs no later than May 31, 2019, and by May 31, 2020, the peer specialist program is required to be established in at least 30 VAMCs.
This section also specifies the selection criteria for selecting VAMCs to establish the peer specialists program. It stipulates that at least 5 of the locations chosen must be polytrauma centers, and at least 10 other locations can be nonpolytrauma centers. In addition, the Secretary must consider the feasibility and advisability of choosing medical centers in rural area, areas that are not in close proximity to an active military installation, and different geographical locations in terms of the census tracts developed by the Census Bureau. It also specifies that female veterans' needs be taken into consideration and to make available female peer specialists.
This section also requires the Secretary to submit a report to Congress on the progress made in establishing the peer specialist program. When the Secretary has carried out the program at the final location, the final report on the program should include recommendations by the Secretary in terms of the feasibility and advisability of expanding the program to additional locations.
Section 507. VA Medical Scribe Program
This section requires the Secretary to establish a two-year pilot program to increase the use of medical scribes. The pilot program must be established in at least 10 VAMCs. Four of the pilot sites must be located in rural areas, four must be in urban areas, and two must be in areas in need of increased access or efficiency.
The section also stipulates that the VA must hire 20 new medical scribes and enter into contracts with appropriate entities for 20 additional medical scribes. It also requires that medical scribes be assigned as follows: four medical scribes must be assigned to each of the 10 medical centers, and of those four, two scribes must be assigned to each of two physicians. In addition, 30% of the medical scribes will be employed in emergency care, while 70% of the medical scribes will be employed in specialty care, specifically those with long patient wait times or low efficiency ratings.
This section also requires the Secretary to submit a report on the pilot program to Congress 180 days after enactment, and every 180 days thereafter. The VA is also required to conduct an analysis on medical scribes under a contract. The analysis should include information on provider efficiency, patient satisfaction, average wait time, the number of patients seen per day by each physician or practitioner, and the amount of time required to hire and train an employee to perform medical scribe functions under the pilot program. The information for the analysis should also include metrics and data for analyzing the effects of the pilot program, including an evaluation of the information above. In addition, not later than 90 days after the termination of the pilot program, the GAO is required to submit a report to Congress on the pilot program, including comparisons with the private sector.
In this section, a medical scribe is defined as an
unlicensed individual hired to enter information into the electronic health record or chart at the direction of a physician or licensed independent practitioner whose responsibilities include the following: (A) Assisting the physician or practitioner in navigating the electronic health record; (B) Responding to various messages as directed by the physician or practitioner; and (C) Entering information into the electronic health record, as directed by the physician or practitioner.
Section 508. Extension of VA Home Loan Guarantee Fees
This section extends the authorization period in which fees are charged from certain veterans for obtaining home-loan guarantees from the VA.
Section 509. Extension of Reduction in VA Pensions for Certain Medicaid-Covered Veterans in Nursing Facilities
This section extends the authorization period until September 30, 2028, that requires the VA pension benefits for veterans and survivors who are residing in Medicaid-approved nursing homes to be reduced to $90 per month to September 30, 2028.
Section 510. Appropriation of Funds
This section authorizes and appropriates $5.2 billion for the VCF established by VACAA. The funds would remain until expended without fiscal year limitation.
Section 512. Budgetary Effects
This section provides that the estimated budgetary effects of the VA MISSION Act are not entered on Pay-As-You-Go (PAYGO) scorecards, thus precluding any possible sequestration as a result of the enactment of this act. The CBO estimated that the act would increase the deficit by $5.2 billion over six years (FY2018-FY2023) and almost $4.5 billion over 11 years (FY2018-FY2028).80 Generally, PAYGO scorecards record the effects on the budget deficit resulting from legislative changes affecting mandatory spending and revenues.81 In particular, a net increase in the deficit on the statutory PAYGO scorecards at the end of the year would require a sequestration (i.e., reduction) of certain mandatory spending by an equivalent amount.82
Appendix. The VA MISSION Act of 2018: Implementation, Reporting Requirements, and Deadlines
Table A-1. The VA MISSION Act of 2018 (P.L. 115-182; as amended by P.L. 115-251):
Major Provisions Pertaining to Implementation, Reporting Requirements, and Deadlines
|
New or Amended Section of 38 U.S.C. |
Section of P.L. 115-182 |
Brief Description |
Implementation and/or Reporting Deadline |
|
Title 1, Chapter 1 Establishing Community Care Programs |
|||
|
38 U.S.C. §1703(e)(4) |
Section 101(a)[creates a new 38 U.S.C. §1703] |
The Secretary is required to publish in the Federal Register and to take all reasonable steps to provide direct notice to eligible veterans stating the time period during which such care and services will be available, the location or locations where such care and services will be available, and the clinical services available at each location provided under the Veterans Community Care Program (VCCP). |
The Secretary is required to publish this notice in the Federal Register at least once a year. |
|
38 U.S.C. §1703(h)(4) |
Section 101(a) |
The Secretary is required to enter into consolidated competitively bid contracts to establish networks of health care providers for purposes of providing access to hospital care, medical services, or extended care services. The Secretary may terminate a contract if the entity fails to meet certain provisions as stipulated by 38 U.S.C. §1703(h)(3)(A) and after notification of Senate and House Appropriations and Veterans' Affairs Committees. |
Whenever the Secretary provides notice to an entity that the entity is failing to meet contractual obligations, the Secretary is required to submit to the Senate and House Committees on Veterans' Affairs a report on such failure. |
|
38 U.S.C. §1703(m)(1)(A) |
Section 101(a) |
The Secretary is required to submit a report to the Senate and House Appropriations and Veterans' Affairs Committees that reviews and provides the types and frequency and the cost of care furnished through the VCCP. |
The first report is due no later than 540 days after enactment (i.e., on November 28, 2019), and subsequent reports are due annually. |
|
38 U.S.C. §1703(m)(3) |
Section 101(a) |
The Secretary is required to submit a report to the Senate and House Veterans' Affairs Committees that provides data on care furnished under VCCP. The report should, among other things, identify how many patients used each type of care and service, identify gaps in care through VCCP and how those gaps may be fixed, and assess total amounts spent by the VA. |
The first report is due no later than 540 days after enactment (i.e., on November 28, 2019), and subsequent reports are due annually. |
|
Section 101(b) |
Stipulates the effective date of the VCCP. |
The VCCP becomes effective on the later of the date that is 30 days after the date on which the Secretary submits a report to the Senate and House Veterans' Affairs Committees indicating that 75% of the amounts deposited in the Veterans Choice Fund have been exhausted, or on the date the Secretary promulgates regulations. |
|
|
Section 101(c)(1) |
The Secretary is required to promulgate regulations to carry out the VCCP. |
No later than one year after the date of the enactment (i.e., on June 6, 2019). |
|
|
Section 101(c)(2) |
Prior to promulgating regulations to carry out the VCCP, the Secretary is required to provide periodic updates to the Senate and House Appropriations and Veterans' Affairs Committees to confirm the progress the Secretary is making toward developing such regulations for the VCCP. |
The first update is required to be provided by no later than 120 days from enactment (i.e., on October 4, 2018). |
|
|
38 U.S.C. §1703A(k) |
Section 102(a) |
The Secretary is required to promulgate regulations to carry out Veterans Care Agreements (VCAs). |
No specific statutory deadline. |
|
38 U.S.C. §1745 |
Section 103(b) |
The Secretary is required to promulgate regulations to carry out VCAs with State Veterans Homes and stipulates the effective date of these VCAs. |
No specific statutory deadline. |
|
38 U.S.C. §1703B(d)(1) |
Section 104(a) |
The Secretary is required to establish access standards for furnishing hospital care, medical services, or extended care services under VCCP. |
Not later than 270 days after enactment (i.e., on March 3, 2019), the Secretary is required to submit a report to the Senate and House Appropriations and Veterans' Affairs Committees detailing the access standards. |
|
38 U.S.C. §1703B(d)(2)(B) |
Section 104(a) |
The Secretary is required to provide periodic updates to the Senate and House Appropriations and Veterans' Affairs Committees on the progress in developing access standards. |
Prior to submitting a report to the Senate and House Appropriations and Veterans' Affairs Committees detailing the access standards, no later than 120 days after enactment (i.e., on October 4, 2018), the Secretary is required to provide a progress update. |
|
38 U.S.C. §1703B(d)(3) |
Section 104(a) |
No later than 540 days after the date the Secretary implements access standards, the Secretary is required to submit a report to the Senate and House Appropriations and Veterans' Affairs Committees on the implementation and compliance of these access standards. |
|
|
38 U.S.C. §1703B(e) |
Section 104(a) |
Not later than three years after the date on which the Secretary establishes access standards, and not less frequently than once every three years thereafter, the Secretary is required to submit to the Senate and House Appropriations and Veterans Affairs' Committees a report on the findings and any modifications to the access standards. |
|
|
38 U.S.C. §1703B(g) |
Section 104(a) |
The Secretary is required to publish the designated access standards in the Federal Register and on an internet VA website. |
No specific statutory deadline. |
|
38 U.S.C. §1703C(a)(5)(A) |
Section 104(a) |
The Secretary is required to establish standards for quality regarding hospital care, medical services, and extended care services furnished by the VA, including through non-VA health care providers. |
Not later than 270 days after enactment (i.e., on March 3, 2019), the Secretary is required to submit a report detailing the standards for quality to the Senate and House Appropriations and Veterans' Affairs Committees. |
|
38 U.S.C. §1703C(a)(5)(B)(ii) |
Section 104(a) |
The Secretary is required to provide periodic updates to the Senate and House Appropriations and Veterans' Affairs Committees on the VA's progress toward developing the standards for quality. |
Not later than 120 days after enactment (i.e., on October 4, 2018), the Secretary is required to provide the first update. |
|
38 U.S.C. §1703C(b)(1) |
Section 104(a) |
The Secretary is required to publish quality ratings of VA medical facilities in the publicly available Hospital Compare website created by the Centers for Medicare & Medicaid Services. |
The Secretary is required to publish the quality ratings not later than one year after the date on which the Secretary establishes standards for quality. The Secretary is required to consider and solicit public comment on potential changes to the measures used not later than two years after the date on which the Secretary establishes standards for quality. |
|
38 U.S.C. §1725A(g) |
Section 105 |
The Secretary is required to develop procedures to ensure that eligible veterans are able to access walk-in care from qualifying non-VA entities or providers. |
Not later than one year after enactment (i.e., on June 6, 2019), the Secretary is required publish regulations to carry out Access to Walk-in Care. The effective date for the program is when final regulations promulgated by the Secretary take effect. |
|
38 U.S.C. §7330C(a)(3)(A) |
Section 106(a) |
The Secretary is required to perform market area assessments regarding the health care services furnished under the laws administered by the Secretary. |
Not less frequently than every four years, the Secretary is required to submit to the Senate and House Appropriations and Veterans' Affairs Committees the market area assessments. |
|
38 U.S.C. §7330C(a)(3)(B) |
Section106(a) |
The Secretary is required to submit an initial market area assessment completed by or performed before the date of enactment (i.e., June 6, 2018). |
No specific statutory deadline. |
|
38 U.S.C. §7330C(b) |
Section 106(a) |
The Secretary is required to submit a strategic four-year plan forecasting the demand for health care from the VA disaggregated by geographic area as determined by the Secretary and the health care capacity to be provided at each VA medical center and the health capacity to be provided through community care providers. |
Not later than one year after enactment (i.e., on June 6, 2019), and not less frequently than once every four years thereafter, the Secretary is required to submit the strategic plan to the Senate and House Appropriations and Veterans' Affairs Committees. |
|
Section 108(a) |
The Secretary is required to deny or revoke the eligibility of a health care provider to provide community care to veterans if the health care provider was removed from VA employment or violated the requirements of a medical license that resulted in the loss of such medical license. |
On or after one year after enactment (i.e., on June 6, 2019), the Secretary is required to implement this requirement. |
|
|
Section 108(d) |
Comptroller General's report on the Secretary's implementation of revocation of certain providers from providing community care. |
Not later than two years after enactment (i.e., on June 6, 2020), the Comptroller General is required to submit a report to Congress. |
|
|
38 U.S.C. §1706A(a) |
Section 109(a) |
The Secretary is required to submit to Congress an assessment of the factors that led the Secretary to determine that a medical service line of the Department is providing care that does not comply with the standards for quality established by the Secretary and a plan with specific actions, and the time to complete them to be taken to comply with such standards for quality. |
Not later than 30 days after determining that a medical service line of the Department is providing care that does not comply with the standards for quality, the Secretary is required to submit to Congress an assessment. Not later than 180 days after submitting an assessment the Secretary is required to submit to Congress a report on the progress of complying with the standards for quality established by the Secretary. Not less frequently than once each year, the Secretary is required to submit to Congress an analysis of the remediation actions with respect to each medical service line. |
|
Title 1, Chapter 2 Paying Providers and Improving Collections |
|||
|
38 U.S.C. §1703D(d)(3) |
Section 111 |
The Secretary is required to submit to Congress a report on payment of overdue claims, disaggregated by paper and electronic claims. |
Not less frequently than annually, the Secretary is required to submit the report. |
|
38 U.S.C. §1703D(h) |
Section 111 |
The Secretary is required to submit a report on the feasibility and advisability of adopting a funding mechanism similar to what is used by other federal agencies to allow a contracted entity to act as a Fiscal Intermediary for the federal government to distribute, or pass through, federal government funds for certain nonunderwritten hospital care, medical services, or extended care services. |
Not later than 90 days after enactment (i.e., September 4, 2018), the Secretary is required to submit the report to the Senate and House Appropriations and Veterans' Affairs Committees. |
|
Title 1, Chapter 3 Education and Training Programs |
|||
|
Section 121(d)(2) |
The Secretary is required to develop and administer an education program that teaches veterans about their health care options and is required to develop a method to evaluate the effectiveness of the education program. |
Not less frequently than once each year, the Secretary is required to submit to Congress a report on the findings of the Secretary with respect to the most recent evaluation conducted by the Secretary. |
|
|
Section 122(b)(3) |
The Secretary is required to develop and implement a training program to train employees and contractors of the VA on how to administer non-VA community health care programs. |
Not less frequently than once each year the Secretary is required to submit to Congress the findings of the Secretary with respect to the most recent evaluation of the training program. |
|
|
Section 123(c) |
The Secretary is required to establish a program to provide continuing medical education material to non-Department medical professionals. |
The Secretary is required to monitor the utilization of the program, evaluate its effectiveness, and report to Congress on utilization and effectiveness not less frequently than once each year. |
|
|
Title 1, Chapter 4 Other Matters Relating to Non-Department of Veterans Affairs Providers |
|||
|
Section 131(c)(3) |
The Secretary is to establish processes to ensure safe opioid prescribing practices by non-VA community healthcare providers. |
Not less frequently than annually, the Secretary is required to submit a report evaluating the opioid prescription compliance of covered health care providers, to the Senate and House Veterans' Affairs Committees. |
|
|
Section 133 |
The Secretary is required to establish standards and requirements for the provision of care by non-VA community health care providers. |
The Secretary is required to establish standards no later than one year after enactment (i.e., on June 6, 2019). |
|
|
Title 1, Chapter 5 Other Non-Department Health Care Matters |
|||
|
Section 141 |
The Secretary is required to submit to Congress a justification for a supplemental appropriations request or any other appropriation outside the standard budget process. |
Not later than 45 days before the date on which such budgetary issue would start affecting a program or service, the Secretary is required to submit to Congress a justification for the request. |
|
|
38 U.S.C. §1701 note |
Section 143 |
The Secretary may not use the authority under Section 101 of VACAA to furnish care and services under the Veterans Choice Program (VCP). |
Not later than one year after enactment (i.e., on June 6, 2019). |
|
Title 1, Chapter 5, Subtitle B Improving Department of Veterans Affairs Healthcare Delivery |
|||
|
38 U.S.C. §1730C(c)(1) |
Section 151(c) |
The Secretary is required to submit to Congress a report on the effectiveness of the use of telemedicine by the VA. |
Not later than one year after earlier of the date on which telemedicine services are provided or regulations are promulgated, the Secretary is required to submit the report to the Senate and House Veterans' Affairs Committees. |
|
38 U.S.C. §1703E |
Section 152 |
The Secretary, acting through the Center for Innovation for Care and Payment, is authorized to carry out pilot programs to develop innovative approaches to testing payment and service delivery models in order to reduce expenditures while preserving or enhancing the quality of care. |
Pilot programs carried out by the Secretary terminate no later than five years after the date of the program's commencement. |
|
Title 1, Chapter 5, Subtitle C Family Caregivers |
|||
|
38 U.S.C. §1720G(a)(2)(B) |
Section 161(a)(1)(A) |
The Secretary is required to expand the Program of Comprehensive Assistance for Family Caregivers to veterans with serious service-connected injuries incurred on or before May 7, 1975. |
During the two-year period beginning on the date on which the Secretary submitted to Congress the certification. |
|
38 U.S.C. §1720G(a)(2)(B) |
Section 161(a)(1)(A) |
The Secretary is required to expand the Program of Comprehensive Assistance for Family Caregivers to veterans with serious service-connected injuries incurred between May 7, 1975, and September 11, 2001. |
After the date that is two years after the date on which the Secretary submits to Congress the certification. |
|
Section 161(a)(1)(B) |
The Secretary is required to certify to Congress that the VA has fully implemented an information technology system that supports the expanded Program of Comprehensive Assistance for Family Caregivers and allows for data assessment and monitoring of the program. |
Not later than 30 days after the Secretary submits the certification to Congress, the Secretary is required to publish in the Federal Register the effective date on which the Program of Comprehensive Assistance for Family Caregivers will be effective. |
|
|
Section 162(a)(1)(A) |
The Secretary is required to implement an information technology system that fully supports the Program of Comprehensive Assistance for Family Caregivers and allows for data assessment and comprehensive monitoring of the program. |
Not later than October 1, 2018. |
|
|
Section 162(b) |
The Secretary is required, through the Under Secretary of Health, to use data from the system and other relevant data to conduct an assessment of how key aspects of the Program of Comprehensive Assistance for Family Caregivers are structured and carried out. |
Not later than 180 days after implementing the system (i.e., March 30, 2019). |
|
|
Section 162(d)(1) |
The Secretary is required to submit to the Senate and House Committees on Veterans' Affairs and the Comptroller General an initial report on the implementation of the information technology system. |
Not later than 90 days after enactment (i.e., on September 4, 2018). |
|
|
Section 162(d)(3) |
The Secretary is required to submit to the Senate and House Committees on Veterans' Affairs and the Comptroller General a final report on the implementation of the information technology system, assessment, and ongoing monitoring and modifications to the Program of Comprehensive Assistance for Family Caregivers. |
Not later than October 1, 2019. |
|
|
Title II, Subtitle A Asset and Infrastructure Review |
|||
|
Section 202 |
The President, with the advice and consent of certain members of Congress, is required to establish a commission of nine members to be known as the Asset and Infrastructure Review Commission (the Commission). |
The President is required to transmit to the Senate the nominations for appointment to the Commission no later than May 31, 2021. The Commission is required to meet only during calendar years 2022 and 2023. The Commission is required to terminate on December 31, 2023. |
|
|
Section 203(a) |
The Secretary is required to provide the criteria proposed to be used by the VA in assessing and making recommendations regarding the modernization and realignment of facilities of the Veterans Health Administration (VHA). |
The Secretary is required, not later than February 1, 2021, to publish in the Federal Register and transmit to the Senate and House Veterans' Affairs Committees the criteria. The Secretary is required to publish in the Federal Register the final criteria no later than May 31, 2021. The Secretary is required to provide an opportunity for public comments on the proposed criteria for at least 90 days. |
|
|
Section 203(b) |
The Secretary is required to include, with the list of recommendations published and transmitted, a summary of the selection process that resulted in the recommendation for each facility of the VHA, including a justification for each recommendation. |
The Secretary is required to, no later than January 31, 2022, and after consulting with veteran service organizations, publish in the Federal Register and transmit to Senate and House Veterans' Affairs Committees and to the Commission a report detailing the recommendations regarding the modernization or realignment of facilities of the VHA on the basis of the final criteria. The Secretary is required to transmit a summary of the selection process that resulted in recommendations for each VA medical facility, seven days after the date of the transmittal (i.e., not later than February 7, 2022) to the Senate and House Veterans Affairs Committees and the Commission of the report detailing the recommendations regarding the modernization or realignment of facilities of the VHA on the basis of the final criteria. |
|
|
Section 203(c) |
The Commission is required to transmit to the President a report containing the Commission's findings and conclusions based on a review and analysis of the recommendations made by the Secretary, together with the Commission's recommendations for modernizations and realignment of facilities of the VHA. |
The Commission is required to, not later than January 31, 2023, transmit to the President along with the Senate and House Veterans' Affairs Committees a report containing the Commission's findings and conclusions. The Commission may change any recommendation made by the Secretary if the Commission publishes a noticed of the proposed change in the Federal Register not less than 45 days before transmitting its recommendations to the President among other requirements. |
|
|
Section 203(d) |
The President is required to approve or disapprove the Commission's recommendations regarding the modernization and realignment of facilities of the VHA. |
The President is required to, not later than February 15, 2023, transmit to the Commission and to the Congress a report containing the President's approval or disapproval of the Commission's recommendations. If the President does not transmit to Congress an approval and certification by March 30, 2023, the process by which facilities of the VHA may be selected for modernization or realignment may be terminated. |
|
|
Section 206(e) |
The Secretary is required to transmit a report containing an account of all the funds credited to and expended from the Department of Veterans Affairs Asset and Infrastructure (VA AIR) Account and any funds remaining in the account. |
Each fiscal year, the Secretary is required to establish a consolidated budget justification in support of the VA AIR Account. Not later than 60 days after the closure of the VA AIR Account, the Secretary is required to transmit a report to the Senate and House Appropriations and Veterans' Affairs Committees. |
|
|
Title II Subtitle B Other Infrastructure Matters |
|||
|
38 U.S.C. §8103(g)(1)(A) |
Section 211(g) |
The Secretary is required to implement a training curriculum and certification program for VA construction personnel. |
Not later than September 30 of the fiscal year following the fiscal year during which the VA Asset and Infrastructure Review Act of 2018 is enacted (i.e., by September 30, 2020), the Secretary is required to ensure that the majority of employees achieve the certification or the appropriate level of certification. |
|
Section 213(a) |
The Secretary is required to submit a report regarding health care furnished by the VA to veterans who live in the Pacific Territories. |
Not later than 270 days after the date of enactment (i.e., March 3, 2019), the Secretary is required submit a report to the Senate and House Veterans' Affairs Committees. |
|
|
Title II Improvements to Recruitment of Healthcare Professionals |
|||
|
Section 302(b) |
The Secretary is required to conduct a study on the demand for education debt reduction under subchapter VII of Chapter 76 of title 38 United States Code. |
Not later than one year after enactment (i.e., June 6, 2019), the Secretary is required to submit to the Senate and House Veterans Affairs' Committees a report on the findings of the Secretary with respect to the study carried out. |
|
|
Section 304(f) |
The Secretary is required to establish a pilot program called the Veterans Healing Veterans Medical Access and Scholarship Program that provides scholarships to veterans to attend certain medical schools in exchange for commitment to practice at a VA facility. |
Not later than December 31, 2020, and annually thereafter for the subsequent three years, the Secretary is required to submit a report to Congress on the pilot program including the number of veterans who received funding under the program who matriculated and an evaluation of the academic progress of such veterans. |
|
|
38 U.S.C. §7681-7684 |
Section 306(b) |
The Secretary is required to ensure that clinical staffs at Vet Centers are eligible to participate in the VA Education Debt Reduction Program. |
Not later than one year after enactment (i.e., on June 6, 2019), the Secretary is required to submit to the Senate and House Veterans' Affairs Committees a report on the number of participants in the Education Debt Reduction Program. |
|
Title IV Healthcare in Underserved Areas |
|||
|
Section 401(d) |
The Secretary is required to develop criteria to designate certain VA medical centers, ambulatory care facilities, and community-based outpatient clinics as underserved facilities. |
Not later than one year after enactment (i.e., on June 6, 2019), and not less frequently than once each year, the Secretary is required to submit to Congress a plan to address the problem of underserved VA facilities. |
|
|
Section 402(d) |
The Secretary is required to carry out a pilot program to furnish mobile development teams of medical personnel to underserved facilities. |
Not later than one year after enactment (i.e., on June 6, 2019), the Secretary is required to submit a progress report to Congress on the implementation of the pilot program. The pilot program will terminate three years after enactment (i.e., on June 6, 2021). Not later than the termination of the pilot program (i.e., before June 6, 2021), the Secretary is required to submit a final report to Congress that includes recommendations on the feasibility and advisability of extending, expanding or making the pilot program permanent. |
|
|
38 U.S.C. §7302 |
Section 403(c) |
The Secretary is required to implement a pilot program to establish medical residency positions authorized under the Veteran Access, Choice, and Accountability Act of 2014 (P.L. 113-146 as amended). |
Not later than one year after enactment (i.e., on June 6, 2019), and not less frequently than once each year thereafter until the termination of the pilot program, the Secretary is required to submit to Congress a report on the implementation of the pilot program. The pilot program shall terminate on August 7, 2024. |
|
Title V Other Matters |
|||
|
38 U.S.C. §726(a) |
Section 501 |
The Secretary is required to submit an annual report on performance awards and bonuses awarded to certain high-level employees, such as the Regional Office Director of the Department, Director of a Medical Center of the Department, Director of a Veterans Integrated Service Network and Senior Executive of the Department. |
Not later than 100 days after the end of each fiscal year, the Secretary is required to submit to the Senate and House Appropriations and Veterans' Affairs Committees an annual report on performance awards and bonuses. |
|
Section 504 |
The Secretary is authorized to carry out certain major medical facility projects and the Secretary is required to submit to Congress a line item account of expenditures relating to construction management carried out by the VA for Livermore, CA, which includes the following elements: future amounts that are budgeted to be obligated for construction management carried out by the VA, and any agreement entered into by the Secretary regarding a non-VA Federal Entity providing management services relating to Livermore, including reimbursement agreements and the costs to the VA for such services. |
Not later than 90 days after enactment (i.e., on September 4, 2018), for the certain major medical facility projects authorized, the Secretary is required to submit to the Senate and House Veterans' Affairs Committees a line item accounting of expenditures relating to construction management. |
|
|
Section 505 |
The Secretary is required to make publicly available on a VA Internet website personnel transparency information displayed by departmental component or, in the case of information relating to VHA positions, by medical facility. |
Not later than 90 days after enactment (i.e., on September 4, 2018), the Secretary is required to make this information public. |
|
|
On a semi-annual basis, the Inspector General of the Department of Veterans affairs is required to review the administration of the website and make recommendations relating to the improvement of such administration. The Secretary is required to submit to Congress an annual report on the steps the VA is taking to achieve full staffing capacity. Each such report is required to include the amount of additional funds necessary to enable the VA to reach full staffing capacity. |
|||
|
Section 506 |
The Secretary is required to carry out a program to establish not fewer than two peer specialists in patient-aligned care teams at VA medical centers. |
Not later than 180 days after enactment (i.e., December 3, 2018) and not less frequently than 180 days thereafter until the Secretary determines that the program is being carried out at the last location to be selected, the Secretary is required to submit to Congress a report on the program. Not later than 180 days after the Secretary determines that the program is being carried out at the last location to be selected, the Secretary is required to submit to Congress a report detailing the recommendation of the Secretary as to the feasibility and advisability of expanding the program to additional locations. |
|
|
Section 507 |
The Secretary is required to carry out a two-year pilot program under which the Secretary is required to increase the use of medical scribes at VA medical centers. |
Not later than 180 days after the commencement of the pilot program required under this section and every 180 days thereafter for this duration of the pilot program, the Secretary is required to submit a Congress a report on the pilot program. Not later than 90 days after the termination of the pilot program, the Comptroller General of the United States is required to submit to Congress a report on the pilot program. Such report is required to include a comparison of the pilot program with similar programs carried out in the private sector. |
|
Source: Table prepared by the Congressional Research Service (CRS) based on statutory language contained in the VA MISSION Act (P.L. 115-182 and P.L. 115-251).
Notes: Certain dates were calculated based on the number of days prescribed in P.L. 115-182 as amended by P.L. 115-251. Where the number of days is dependent upon certain preceding actions, only the number of days as indicated in the statute is presented.
Author Contact Information
Acknowledgments
Christopher M. Davis and Bill Heniff, Analysts on Congress and the Legislative Process in the Government and Finance Division, and Alison M. Smith, Legislative Attorney in the American Law Division, made contributions to this report. Jose P. Ordoveza, Visual Information Specialist, provided graphical assistance, and Sehar F. Minhas, Presidential Management Fellow, on a developmental assignment from the Department of Veterans Affairs, provided invaluable assistance with parts of this report.
Footnotes
| 1. |
Jennifer Daley, "Ensuring Timely Access to Quality Care for US Veterans," The Journal of the American Medical Association, vol. 319, no. 5 (February 6, 2018), p. 440. Also see Terri Tanielian et al., Ready or Not? Assessing the Capacity of New York State Health Care Providers to Meet the Needs of Veterans, RAND Corporation, Santa Monica, CA, 2018, https://www.rand.org/pubs/research_reports/RR2298.html. |
| 2. |
Jennifer Daley, "Ensuring Timely Access to Quality Care for US Veterans," The Journal of the American Medical Association, vol. 319, no. 5 (February 6, 2018), p. 440. |
| 3. |
RAND Corporation, Assessment C (Care Authorities), The MITRE Corporation. A Product of the CMS Alliance to Modernize Healthcare Federally Funded Research and Development Center Centers for Medicare & Medicaid Services (CMS) Prepared For the U.S. Department of Veterans Affairs, September 1, 2015, p. 22. |
| 4. |
World War Veterans Act of 1924 (S. 2257; P.L. 68-242; 43 Stat. 610, c. 320). |
| 5. |
Veterans Administration, Annual Report of the Administrator of Veterans Affairs, Annual Report for Fiscal Year Ending June 30, 1946, Washington, DC, January 6, 1947, p. 3. |
| 6. |
Veterans Administration, Annual Report of the Administrator of Veterans Affairs, Annual Report for Fiscal Year Ending June 30, 1950, Washington, DC, January 4, 1951, p. 30. |
| 7. |
Ibid., p. 33. |
| 8. |
Veterans' Benefits Act of 1957 (H.R. 53, P.L. 85-56; 71 Stat. 110). |
| 9. |
U.S. Congress, Senate Committee on Veterans' Affairs, Veterans Omnibus Health Care Act of 1976, Hearings on S. 2908 and Related Bills, 94th Cong., February 18 and 19, 1976 (Washington: GPO, 1977), p. 104. |
| 10. |
Department of Veterans Affairs, Office of Inspector General (OIG), Administrative Summaries of Investigation Regarding Wait Time, available at https://www.va.gov/oig/publications/administrative-summaries-of-investigation.asp, accessed on July 20, 2018; and U.S. Congress, House Committee on Veterans' Affairs, Scheduling Manipulation and Veteran Deaths in Phoenix: Examination of the OIG'S Final Report, 113th Cong., 2nd sess., September 17, 2014, H.Hrg. 113–87 (Washington: GPO, 2015). |
| 11. |
For more information on the implementation of the Veterans Choice Program (VCP), see CRS Report R44562, The Veterans Choice Program (VCP): Program Implementation. |
| 12. |
Department of Veterans Affairs, Office of the Inspector General, Veterans Health Administration Review of the Implementation of the Veterans Choice Program, 15-04673-333, January 30, 2017; Department of Veterans Affairs, Office of the Inspector General, Accuracy and Timeliness of Payments Made Under the Choice Program Authorized by the Veterans Access, Choice, and Accountability Act, Memorandum to the Secretary of Veterans Affairs, September 12, 2017; U.S. Government Accountability Office, Veterans Choice Program: Improvements Needed to Address Access-Related Challenges as VA Plans Consolidation of its Community Care Programs, GAO-18-281, June 2018; U.S. Congress, House Committee on Veterans' Affairs, Shaping The Future: Consolidating And Improving VA Community Care, 115th Cong., 1st sess., March 7, 2017 (Washington: GPO, 2018). |
| 13. |
Section 403 the Veterans' Mental Health and Other Care Improvements Act of 2008 (P.L. 110-387) required the VA to conduct pilot programs during a three-year period to provide non-VA health care services through contractual arrangements to eligible veterans in in rural areas. The Caregiver and Veterans Omnibus Health Services Act of 2010 (P.L. 111-163) made technical corrections regarding hardship exception and the mileage standard. The program was established in 2011 and was extended by the Veterans Access, Choice, and Accountability Act (VACAA) of 2014 (P.L. 113-46, as amended) and expired on August 7, 2016. Veterans under the ARCH program were then provided care under the VCP using the unusual or excessive burden provision contained VACAA of 2014 (P.L. 113-46, as amended). |
| 14. |
The PC3 program traces its roots to the pilot program known as the Project HERO (Healthcare Effectiveness Through Resource Optimization). The five-year pilot was established in 2007 in response to the conference committee report issued to accompany the FY2006 Military Quality of Life and Veterans Affairs Appropriations Act (P.L. 109-114). Congress intended Project HERO to be implemented in similar manner to private health care and managed care-contracted services models. When the Project HERO pilot ended, the VA awarded a new contract called Patient-Centered Community Care, known as PCCC or PC3, as a regional contracting vehicle to partner with private health care providers. When the VCP was established in 2014 by the by the Veterans Access, Choice, and Accountability Act (VACAA) of 2014 (P.L. 113-46, as amended), VA modified the PC3 contracts, and the two commercial vendors became the third-party administrators of the VCP. |
| 15. |
Department of Veterans Affairs, Plan to Consolidate Programs Department of Veterans Affairs to Improve Access to Care, October 30, 2015, https://www.va.gov/opa/publications/va_community_care_report_11_03_2015.pdf (accessed August 8, 2018). |
| 16. |
Department of Veterans Affairs, "VA Announces Veterans Coordinated Access & Rewarding Experiences ('CARE') Act: Replaces Current '30-day/40-mile' System with Patient/Provider-centric Decision-making," press release, October 16, 2017, https://www.va.gov/opa/pressrel/pressrelease.cfm?id=2963(accessed August 8, 2018). |
| 17. |
U.S. Congress, House Committee on Veterans' Affairs, Legislative Hearing on: Draft legislation to establish a permanent Veterans Choice Program; Draft legislation to modify VA's authority to enter into agreements with State homes to provide nursing home care to veterans, to direct the Secretary to carry out a program to increase the number of graduate medical education residency positions, and for other purposes; Draft legislation, to direct VA to conduct a study of the Veterans Crisis Line; Draft legislation, to direct VA to furnish mental health care to veterans at community or non-profit mental health providers participating in the Veterans Choice Program; the Department of Veterans Affairs' (VA's) legislative proposal, the Veteran Coordinated Access and Rewarding Experiences (CARE) Act; H.R. 1133; H.R. 2123; H.R. 2601; and, H.R. 3642," 115th Cong., 2nd sess., October 24, 2017. |
| 18. |
For an in-depth discussion on the measures introduced and considered by the Senate Veterans Affairs Committee, see U.S. Congress, Senate Committee on Veterans' Affairs, Caring for Our Veterans Act of 2017, Report to Accompany S. 2193, 114th Cong., 2nd sess., March 7, 2018, S.Rept. 115-212 (Washington: GPO, 2018), pp. 1-4. |
| 19. |
Donald J. Trump, Statement by the President on the John S. McCain III, Daniel K. Akaka, and Samuel R. Johnson VA Maintaining Internal Systems and Strengthening Integrated Outside Networks Act of 2018, or the "VA MISSION Act of 2018," https://www.whitehouse.gov/briefings-statements/statement-by-the-president-3/ (accessed August 8, 2018). |
| 20. |
Congressional Budget Office (CBO), Cost Estimate, H.R. 5674, VA Maintaining Internal Systems and Strengthening Integrated Outside, May 14, 2018, https://www.cbo.gov/publication/53871. The House amended S. 2372 to include the text of H.R. 5674, as reported, with "technical and procedural corrections." |
| 21. |
Ibid., p. 18. |
| 22. |
Ibid., p. 8. |
| 23. |
Ibid., p. 21. |
| 24. |
38 U.S.C. §1705 requires the VA to establish a patient enrollment system. A veteran must be enrolled in the VA health care system as a condition for receiving care. Once a veteran is enrolled, the veteran remains in the system and does not have to reapply for enrollment annually. Enrolled veterans do not pay any premiums, deductibles, or coinsurance for their care. Some veterans are required to pay copayments. |
| 25. |
Even if not enrolled in the VA health care system, some veterans are eligible to receive care through the VA health care system. See 38 C.F.R §17.37 for conditions under which enrollment is not required for hospital and outpatient care. |
| 26. |
Title 42 U.S.C.§§1395 et seq. Providers, under Medicare, include patient care institutions such as hospitals, critical access hospitals, hospices, nursing homes, and home health agencies. See https://www.cms.gov/Medicare/Provider-Enrollment-and-Certification/CertificationandComplianc/index.html. |
| 27. |
For more information on military treatment facilities, see CRS In Focus IF10530, Defense Primer: Military Health System. |
| 28. |
For more information on the IHS health care system, see CRS Report R43330, The Indian Health Service (IHS): An Overview. |
| 29. |
As defined in Section 1905(l)(2)(B) of the Social Security Act (42 U.S.C. §1396d(l)(2)(B)). For more information on FQHCs, see CRS Report R43937, Federal Health Centers: An Overview. |
| 30. |
For more information on the 40-mile distance eligibility criteria under VCP, see CRS Report R44562, The Veterans Choice Program (VCP): Program Implementation. |
| 31. |
Amended by the Department of Veterans Affairs Expiring Authorities Act of 2018 (S. 3479; P.L. 115-251). |
| 32. |
Title 42 U.S.C. §§1395 et seq. Providers under Medicare include patient care institutions such as hospitals, critical access hospitals, hospices, nursing homes, and home health agencies. See, https://www.cms.gov/Medicare/Provider-Enrollment-and-Certification/CertificationandComplianc/index.html. |
| 33. |
Amended by the Department of Veterans Affairs Expiring Authorities Act of 2018 (S. 3479; P.L. 115-251). |
| 34. |
The PCCC (PC3) contracts were awarded in September 2013 to provide inpatient and outpatient specialty care and mental health care for eligible veterans when the local VA Medical Center (VAMC) cannot readily provide the services, such as when there is a lack of available specialists, there are long wait times, or there is an extraordinary distance from a veteran's home. |
| 35. |
As amended by the Consolidated and Further Continuing Appropriations Act, 2015 (P.L. 113-235). Maryland operates the nation's only all-payer hospital rate regulation system. Under Section 1814(b)(3) of the Social Security Act, the Centers for Medicare & Medicaid Services (CMS) has exempted certain hospitals in Maryland from reimbursement under the national payment system and has allowed the state to set reimbursement rates payable by Medicare for applicable services that otherwise would be reimbursed under Medicare's Inpatient Prospective Payment System (IPPS) and Outpatient Prospective Payment System (OPPS). On January 10, 2014, CMS and the State of Maryland jointly announced a new initiative to modernize Maryland's unique all-payer rate-setting system for hospital services. In the state of Maryland, the VA will follow this reimbursement system (also see https://innovation.cms.gov/initiatives/Maryland-All-Payer-Model/). |
| 36. |
https://optn.transplant.hrsa.gov/ (accessed August 14, 2018). |
| 37. |
42 U.S.C. §1320a-7b(f) defines "federal health care program" as (1) any plan or program that provides health benefits, whether directly through insurance, or otherwise, that is funded directly, in whole or in part, by the U.S. government (not including health insurance provided to federal government employees), or (2) any state health care program, as defined in Section 1128(h) of the Social Security Act (42 U.S.C. §1320a-7(h)). |
| 38. |
Amended by the Department of Veterans Affairs Expiring Authorities Act of 2018 (S. 3479; P.L. 115-251). |
| 39. |
Office of Federal Contract Compliance Programs (OFCCP) is responsible for enforcing Executive Order (E.O.) 11246, as amended; Section 503 of the Rehabilitation Act of 1973, as amended; and the Vietnam Era Veterans' Readjustment Assistance Act of 1974 (VEVRAA), as amended. Collectively, these laws prohibit federal contractors and subcontractors from discriminating on the basis of race, color, religion, sex, national origin, and status as a qualified individual with a disability or protected veteran. Beginning May 7, 2014, for a period of five years, OFCCP stopped enforcement activities on TRICARE subcontractors. For more details and background, see Department of Labor, Office of Federal Contract Compliance Programs, DIRECTIVE (DIR) 2014-01 https://www.dol.gov/ofccp/regs/compliance/directives/dir2014_01.htm. |
| 40. |
Amended by the Department of Veterans Affairs Expiring Authorities Act of 2018 (S. 3479; P.L. 115-251). |
| 41. |
Amended by the Department of Veterans Affairs Expiring Authorities Act of 2018 (S. 3479; P.L. 115-251). |
| 42. |
VHA, Credentialing and Privileging, VHA Handbook 1100.19, Washington, DC, October 15, 2012. |
| 43. |
VA, "Authority of Health Care Providers to Practice Telehealth," 82 Federal Register 45757, October 2, 2017. |
| 44. |
VA, "Authority of Health Care Providers to Practice Telehealth," 83 Federal Register 21897-21907, May 11, 2018. |
| 45. |
Telemedicine is the electronic delivery of a clinical health care service via a technological method. See Department of Health and Human Services (HHS), Report to Congress: E-health and Telemedicine, August 12, 2016, pp. 4-5, https://aspe.hhs.gov/system/files/pdf/206751/TelemedicineE-HealthReport.pdf. The Department of Veterans Affairs uses the term "telehealth" in its regulations to mean "the use of electronic information or telecommunications technologies to support clinical health care, patient and professional health-related education, public health, and health administration" (38 C.F.R. §17.417). |
| 46. |
Department of Veterans Affairs, FY2019 Congressional Budget Submission, Medical Programs and Information Technology Programs, Volume 2 of 4, February 2018, pp. VHA-251. |
| 47. |
Honorable Bob Graham, "Statements on Introduced Bill and Joint Resolutions," remarks in the Senate, Congressional Record, 108th Congress, vol. 149 (June 18, 2003), p. S8135. |
| 48. |
CMS Alliance to Modernize Healthcare Federally Funded Research and Development Center, MITRE Corporation, Independent Assessment of the Health Care Delivery Systems and Management Processes of the Department of Veterans Affairs, Volume I: Integrated Report, September 1, 2015, pp. K-2. |
| 49. |
The Veterans Access, Choice, and Accountability Act of 2014 (P.L. 113-146, as amended). |
| 50. |
Commission on Care, Final Report of the Commission on Care, June 30, 2016, p.55. |
| 51. |
U.S. Congress, House Committee on Veterans' Affairs, Care Where It Counts: Assessing VA's Capital Asset Needs, 115th Cong., 1st sess., July 12, 2017 (Washington: GPO, 2018), p. 5. |
| 52. |
For more information, see CRS Report 98-425, Invoking Cloture in the Senate, by Christopher M. Davis. |
| 53. |
§207(a). |
| 54. |
The Secretary could not take action during the 45-day layover period because, although no privileged joint resolution might be introduced, Congress could still act during the period to disapprove the recommendations using the regular (nonexpedited) legislative process. |
| 55. |
§207(a)(1). A preamble is introductory language, usually framed as a series of "whereas" clauses, that explains the reasons for, and intent of, a resolution. |
| 56. |
§207(a)(3). |
| 57. |
§207(a)(2). |
| 58. |
Refer the same measure to other committees subject to time limits imposed after the primary committee has reported the measure. |
| 59. |
A legislative day begins when the House meets following an adjournment of any length, and concludes when the House adjourns again. |
| 60. |
A session day is any calendar day on which the Senate meets, including in pro forma session. |
| 61. |
§207(b)(1) and §207(c)(2). In the House, this would likely be the Union Calendar, the calendar reserved for legislation that raises revenue, directly or indirectly appropriates money or property, or authorizes the expenditure of appropriations. In the Senate, the measure would be placed on the Calendar of Business. |
| 62. |
For more information, see CRS Report 98-427, Considering Measures in the House Under the One-Hour Rule, by James V. Saturno. |
| 63. |
In the House, in most cases, the minority leader or her designee is guaranteed the opportunity to offer a motion to recommit with instructions to a bill or joint resolution during its initial House consideration. Under the AIRC procedure, however, the motion is barred, presumably because the adoption of a motion to recommit with instructions could alter the resolution's prescribed text and create the need for the House and Senate to resolve legislative differences before presenting the measure to the President. |
| 64. |
In the Senate, a single quorum call is in order immediately prior to the vote on final passage if requested by any Senator. |
| 65. |
Note that Congress is, in effect, asking the President to enact a joint resolution terminating a list of recommendations that he, himself, recently approved. For this reason, some have argued that if a President is presented with a joint resolution of disapproval, it is a virtual certainty that he would veto it. |
| 66. |
For more information, see CRS Report RS22654, Veto Override Procedure in the House and Senate, by Elizabeth Rybicki. |
| 67. |
William Holmes Brown, Charles W. Johnson, and John V. Sullivan, House Practice, A Guide to the Rules, Precedents, and Procedures of the House (Washington: GPO, 2017), ch. 50, §4, p. 854. |
| 68. |
Amended by the Department of Veterans Affairs Expiring Authorities Act of 2018 (S. 3479; P.L. 115-251). |
| 69. |
See Section 301 in CRS Report R43704, Veterans Access, Choice, and Accountability Act of 2014 (H.R. 3230; P.L. 113-146). |
| 70. |
U.S. Department of Veterans Affairs, "VA Careers, Education Support, Health Professional Scholarship Program," https://www.vacareers.va.gov/why-choose-va/education-support.asp. |
| 71. |
The section specifies that Teague Cranston Act medical schools (Texas A&M College of Medicine, Quillen College of Medicine at East Tennessee State University, Boonshoft School of Medicine at Wright State University, Joan C. Edwards School of Medicine at Marshall University, and University of South Carolina School of Medicine) and four medical schools at Historically Black Colleges and Universities (Charles R Drew University of Medicine and Science, Howard University College of Medicine, Meharry Medical College, and Morehouse School of Medicine) are considered covered medical schools in this section. |
| 72. |
Department of Health and Human Services, Health Resources and Services Administration, "Shortage Designation," https://bhw.hrsa.gov/shortage-designation. |
| 73. |
U.S. Government Accountability Office, Physician Workforce: HHS Needs Better Information to Comprehensively Evaluate Graduate Medical Education Funding, 18-240, March 2018. |
| 74. |
CRS Report R43587, The Veterans Health Administration and Medical Education: In Brief. |
| 75. |
CRS Report R44376, Federal Support for Graduate Medical Education: An Overview. |
| 76. |
CRS Report R43587, The Veterans Health Administration and Medical Education: In Brief. |
| 77. |
U.S. Government Accountability Office, Physician Workforce: Locations and Types of Graduate Training Were Largely Unchanged, and Federal Efforts May Not Be Sufficient to Meet Needs, 17-141, May 2017. |
| 78. |
U.S. Government Accountability Office, Physician Workforce: HHS Needs Better Information to Comprehensively Evaluate Graduate Medical Education Funding, 18-240, March 2018. |
| 79. |
A peer specialist is a "veteran who has recovered or is recovering from a mental health condition; and has been certified by (i) a not-for-profit entity engaged in peer specialist training as having met such criteria as the [VA] Secretary shall establish for a peer specialist position; or (ii) a State as having satisfied relevant State requirements for a peer specialist position" 38 U.S.C. §7402(b)(13). In addition to these basis requirements those applying to be peer specialist must generally have at least one year of "specialized experience is progressively responsible, post-personal mental health recovery experience as a mentor providing counseling to support peers in mental health and/or addiction recovery, a recovery advocate directly involved with consumers of mental health services, a psychiatric therapy aide, or equivalent work involving in-person communication to support others in mental health recovery." VA HANDBOOK 5005/59 p. II-F3-1, July 17, 2012. |
| 80. |
CBO cost estimate, H.R. 5674, VA Maintaining Internal Systems and Strengthening Integrated Outside Networks Act of 2018, as reported by the House Committee on Veterans' Affairs on May 11, 2018 (May 14, 2018). The House amended S. 2372 to include the text of H.R. 5674, as reported, with "technical and procedural corrections." |
| 81. |
For more information on the PAYGO scorecards, see CRS Report R41157, The Statutory Pay-As-You-Go Act of 2010: Summary and Legislative History, and CRS Report RL31943, Budget Enforcement Procedures: The Senate Pay-As-You-Go (PAYGO) Rule. |
| 82. |
Similar provisions have been included in other legislation over the last several years. For more information, see Congressional Distribution Memorandum, "Budgetary Effects Excluded from the Statutory Pay-As-You-Go (Stat-PAYGO) Scorecards," January 25, 2018 (updated), by Bill Heniff Jr. Available from the author upon request. |