The Veterans Health Administration and Medical Education: In Brief
In the wake of World War II, an influx of veterans requiring medical care threatened to overwhelm the capacity of the Department of Veterans Affairs (VA) to provide such care. In 1946, the VA began entering into affiliations with medical schools as one strategy to increase capacity—both in the short term and in the long term. In the short term, some trainees—in particular, those in the later years of training—may provide direct care to patients, thereby increasing provider capacity and patient access. In the long term, training physicians at the VA creates a pipeline for recruiting physicians as VA employees. Current concerns about the VA’s capacity to provide access to care have returned attention to the role of medical training at the VA.
The VA is the largest provider of medical training in the United States and is involved in training at all levels: medical students, medical residents, and medical fellows. VA’s physician training programs are conducted primarily through its affiliations with medical schools and, in some instances, with teaching hospitals. In general, the purpose of these affiliation agreements is to enhance patient care and education, but some may also include medical research. Under these affiliation agreements, the VA and the relevant educational institution share responsibility for the academic program. The affiliation agreement promotes common standards for patient care, medical student and resident education, research, and staff appointments.
Generally, the VA is not the primary sponsor of medical education. Specifically, the VA does not operate its own medical school, but medical students from an affiliated institution may do a clinical rotation at an affiliated VA facility. Similarly, the VA does not typically operate its own residency programs (called graduate medical education or GME); instead, residents would apply to the medical school or teaching hospital that is the primary sponsor of the residency program and then would spend a portion of their residency training at the VA. The exception to this model is fellowship level training, which occurs after a medical school graduate has completed a residency program. In limited instances, the VA directly operates fellowship training programs in subspecialties that are of high importance to the VA.
The majority of VA facilities and the majority of U.S. medical schools (both allopathic and osteopathic) have affiliation agreements to train physicians.
The VA is the second largest federal payer for medical training after Medicare’s GME payments. Medicare GME payments were $11.2 billion in FY2013, compared with VA’s spending of approximately $1.5 billion in GME training in FY2015. Funds appropriated for the VA health care system are divided into two major components: General Purpose funding and Specific Purpose funding, both of which support some aspects of physician training.
General purpose funds are distributed at the start of the fiscal year to the Veterans Integrated Service Networks (VISNs) and are used in part to fund administrative costs of residency training programs.
Specific purpose funds are generally administered centrally and are provided to VA medical facilities to fund, among other things, residents’ stipends and fringe benefits.
The Veterans Health Administration and Medical Education: In Brief
Contents
- Background
- The VA's Involvement in Medical Training
- Academic Affiliations
- VA Funding of Physician Training
- Ongoing GME Expansion
Figures
Tables
Appendixes
Background
Training health care professionals—including physicians1—is part of the VA's statutory mission.2 It does so to provide an adequate supply of health professionals overall and for the VA's health system. This mission began in 1946, when the VA began entering into affiliations with medical schools as one strategy to increase capacity.3 Some trainees—in particular, those in the later years of training—may provide direct care to patients, thereby increasing provider capacity and patient access. In the long term, training physicians at the VA creates a pipeline for recruiting physicians as VA employees.4 In 2014, the Veterans Access, Choice, and Accountability Act of 2014 (VACAA, P.L. 113-46, as amended) initiated an expansion of the VA's medical training by requiring the VA to increase the number of graduate medical education positions at VA medical facilities by 1,500 positions over a five-year period beginning July 1, 2015, through 2019.5 P.L. 114-315 extended this time period to 10 years (i.e., through FY2024).
The VA's Involvement in Medical Training
The VA is the largest provider of medical training in the United States and is involved in training at all levels: medical students, medical residents, and medical fellows (see Table 1).6
|
Trainee Type |
Description |
Number in Training |
|||
|
VA |
U.S. Total |
||||
|
Medical Students |
The VA serves as a site for clinical rotations during medical school; this is also called undergraduate medical education.a |
24,683 |
|
||
|
Medical Residents |
Through affiliations with hospitals and academic medical centers, the VA serves as a training site for medical residents; this is also called graduate medical education (GME). |
|
|
||
|
Fellows |
Through affiliations with hospitals and academic medical centers, the VA serves as a training site for fellows (individuals who have completed residency training and are pursuing additional training in order to subspecialize.) |
|
|
||
Sources: VA data from U.S. Department of Veterans Affairs. Office of Academic Affiliations, "2017 Statistics: Health Professions Trainees," https://www.va.gov/OAA/docs/OAA_Statistics_Short_2017.pdf. Medical school enrollment data from the Association of American Medical Colleges, "Table B-1.2: Total Enrollment at U.S. Medical School and Sex, 2013-2014 through 2075-2018," and American Association of Colleges of Osteopathic Medicine, "Preliminary Enrollment Report Fall 2017"; these data are totaled to determine the total number of medical students. Medical Resident and Fellow data from Sarah E. Brotherton and Sylvie I. Etzel, "Graduate Medical Education, 2016-2017," Journal of the American Medical Association, vol. 318, no. 23 (December 19, 2017), pp. 2368-2387.
a. In general, medical education consists of four years of college education leading to a bachelor's degree followed by four years of medical school (also known as undergraduate medical education). Medical students during their first two years are generally receiving classroom instruction and not clinical training; therefore, they would not be eligible to rotate to any type of a facility for clinical instruction.
b. The total number of medical students is composed of medical students enrolled in allopathic schools of medicine (i.e., MD granting schools) and osteopathic schools of medicine (i.e., DO granting schools). Medical school graduates who complete their education at foreign medical schools may also spend a portion of their residency at VA facilities.
c. These data indicate the number of residents or fellows in training at programs accredited by the Accreditation Council for Graduate Medical Education (ACGME) or those jointly accredited by the ACGME and the American Osteopathic Association (AOA). The two systems are merging to create a single accreditation system that should be fully in effect in 2020. During the 2015-2016 academic year, there were 6,745 residents and fellows in programs accredited by the American Osteopathic Association. See American Osteopathic Association, "OMP Report: Postdoctoral Training," http://www.osteopathic.org/inside-aoa/about/aoa-annual-statistics/Pages/osteopathic-postdoctoral-training.aspx.
Academic Affiliations
The VA's physician training programs are conducted primarily through its affiliations with medical schools and, in some instances, with teaching hospitals. In general, the purpose of these affiliation agreements is to enhance patient care and education, but some may also include medical research. Under these affiliation agreements, the VA and the relevant educational institution share responsibility for the academic program. The affiliation agreement promotes common standards for patient care, medical student and resident education, research, and staff appointments.7 In 2017, the VA's physician education program included affiliations with 144 of 149 allopathic medical schools and all 34 osteopathic medical schools.8 Under affiliation agreements, VA clinicians may, at the discretion of the academic institution, be granted academic appointments to medical school faculty. Approximately 70% of VA staff clinicians have a faculty appointment at an affiliated school of medicine.9 VA staff clinicians may be jointly employed by the VA and the affiliated medical center, may volunteer their time as faculty, or the VA may contract with the academic affiliate for faculty.
Generally, the VA is not the primary sponsor of medical education.10 Specifically, the VA does not operate its own medical schools, but medical students from affiliated institutions may do one or more clinical rotations at affiliated VA facilities. Similarly, the VA does not typically operate its own residency programs. Instead, residents apply to the medical school or teaching hospital that is the primary sponsor of the residency program and then spend a portion of their residency training at the VA. The exception to this model is fellowship level training, where the VA directly operates fellowship training programs in subspecialties that are of high importance to the VA.11
VA Funding of Physician Training
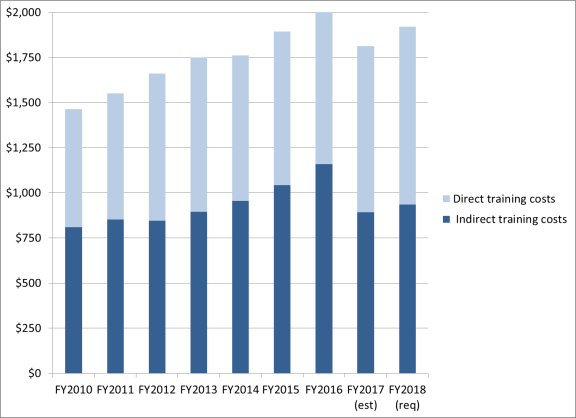
The VA is the second-largest federal payer for medical training after Medicare, which subsidizes graduate medical education (GME) at teaching hospitals. Medicare GME payments totaled $11.2 billion in FY2013.12 Between FY2010 and FY2017 (est.), the VA has spent $13.9 billion on health professionals training, including but not limited to physician training (see Figure 1).13 Funds appropriated for training are divided into direct training costs and indirect training costs, both of which support some aspects of physician training. Direct training costs are generally administered centrally and are provided to VA medical facilities to fund, among other things, residents' stipends and fringe benefits. Indirect training costs are used in part to fund administrative costs of residency training programs such as salaries of VA instructors in the GME and associated health professional training programs, and space and equipment needs.14
Ongoing GME Expansion
The Veterans Access, Choice, and Accountability Act of 2014 (P.L. 113-146, as amended) required an increase in the number of GME positions by up to 1,500 over a 10-year period,15 beginning July 1, 2015, through 2024, with an emphasis on primary care, mental health, and other specialties the VA Secretary deems appropriate. As part of this expansion, the VA has allocated 547 new VA positions for residents; 70% were in primary care or mental health. The remaining new positions were in a specialty designated as a "critical need" by the VA Secretary.16 The legislation also required that the expansion focus on creating new programs at VA facilities where there had not previously been GME training and the new positions be awarded for training in rural or otherwise underserved areas. As part of the GME expansion, VA's OAA identified VA facilities without GME programs and has worked to establish, or begin the planning process to establish, GME programs at all but 4 of the 22 sites that the VA identified as not having GME.17 The VA's objective is to add an additional 953 additional GME positions by 2025.18
Appendix. VA Health Professional Training
The Veteran's Health Administration facilities are the largest sites for health professional training in the United States. Physicians, including medical students, residents, and fellows, are the largest type of health professionals trained, but the VA trains over 40 types of health professionals. In doing so, it partners with over 1,800 unique colleges and universities, including those that serve racial and ethnic minority groups who are traditionally underrepresented in the health professions (such as Historically Black Colleges and Universities, and Tribal colleges).
The table below presents eight years of data on VA's health professional training and shows a 7% increase in total health professionals trained over the time period with the number trained increasing in nearly all fields.
|
2009 |
2010 |
2011 |
2012 |
2013 |
2014 |
2015 |
2016 |
2017a |
|
|
Advanced Fellows (Medicine) |
175 |
239 |
288 |
297 |
253 |
311 |
387 |
452 |
463 |
|
Associated Healthb |
23,483 |
23,871 |
24,608 |
25,122 |
26,121 |
26,454 |
26,135 |
26.932 |
25,428 |
|
Dental Residents & Students |
1,280 |
1,267 |
1,231 |
1,195 |
1,397 |
1,398 |
986 |
1,044 |
849 |
|
Physician Residents |
36,410 |
36,745 |
36,816 |
37,809 |
40,420 |
41,697 |
43,013 |
43,768 |
43,565 |
|
Medical Students |
20,245 |
20,516 |
21,502 |
20,218 |
21,541 |
23,031 |
24,283 |
25,707 |
24,683 |
|
Nursing Traineesc |
33,092 |
32,662 |
32,349 |
32,859 |
29,067 |
28,086 |
28,389 |
28,845 |
27,549 |
|
Non-Health Professionalsd |
N/A |
N/A |
N/A |
N/A |
N/A |
359 |
359 |
463 |
412 |
|
Total |
114,685 |
115,300 |
116,794 |
117,500 |
118,799 |
121,345 |
123,552 |
127,211 |
122,949 |
Source: U.S. Department of Veterans Affairs. Office of Academic Affiliations, "2017 Statistics: Health Professions Trainees," https://www.va.gov/OAA/docs/OAA_Statistics_Short_2017.pdf.
Notes: The VA aggregates these data based on information it receives from the "Health Services Training Report," which each facility completes at the conclusion of each fiscal year. Data are not unduplicated (i.e., it is possible, though unlikely, for trainees to have trained at more than one VA facility and therefore be counted more than once in these data).
a. To improve the accuracy of its data collection, beginning in 2017, the VA changed its data collection from fiscal years to academic year time frame.
b. Includes all health disciplines that are not medicine, dentistry, or nursing (e.g., psychologists, pharmacists, and social workers).
c. Includes graduate and undergraduate level trainees.
d. Includes individuals in professions such as engineering, information technology, or finance.
Over the past six years, the VA has also expanded its mental health training. Specifically, since 2012, the VA has supported an additional 750 trainees in various mental health professions. This represents facilities with existing programs that grew in program size and new facilities that commenced mental health training. Trainees were added in a variety of fields, including
- clinical pastoral education,
- licensed professional mental health counseling,
- marriage and family counseling,
- mental health nursing,
- occupational therapy,
- pastoral counseling,
- pharmacy,
- physician assistant,
- psychiatry,
- psychology, and
- social work.
Author Contact Information
Footnotes
| 1. |
This report focuses on physician training; information on the full complement of VA health professional training is available in this report's appendix. |
| 2. |
38 U.S.C. §7302. |
| 3. |
See U.S. Department of Veterans Affairs, Policy Memorandum No. 2, Subject: Policy in Association of Veteran's Hospitals with Medical Schools, Washington, DC, January 30, 1946, http://www.va.gov/oaa/Archive/PolicyMemo2.pdf. |
| 4. |
The VA reports that nearly 60% of VA physicians had trained at the VA prior to their employment. U.S. Department of Veterans Affairs (VA). Office of Academic Affiliations, "Mission of the Office of Academic Affiliations," https://www.va.gov/oaa/oaa_mission.asp. |
| 5. |
CRS Report R43704, Veterans Access, Choice, and Accountability Act of 2014 (H.R. 3230; P.L. 113-146), by [author name scrubbed] et al. |
| 6. |
U.S. Department of Veterans Affairs (VA). Office of Academic Affiliations, "About Medical & Dental Education Programs," https://www.va.gov/oaa/gme_default.asp#GMEPrograms. |
| 7. |
Drawn from a sample copy of VA Form 10-0094a, "Medical Education Affiliation Agreement Between Department of Veterans Affairs (VA), and A School Of Medicine and its Affiliated Participating Institutions." |
| 8. |
Allopathic medical schools grant a Doctor of Medicine degree (M.D.); osteopathic medical schools grant a Doctor of Osteopathic Medicine degree (D.O.). The 34 osteopathic medical schools operate programs at 49 locations; for more information, see American Association of Colleges of Osteopathic Medicine, "U.S. College of Osteopathic Medicine," http://www.aacom.org/become-a-doctor/us-coms. |
| 9. |
Department of Veterans Affairs, 20 Reasons Doctors Like Working for the Veterans Health Administration, https://www.va.gov/HEALTH/docs/20ReasonsVHA_508_IB10935.pdf. |
| 10. |
The VA reports that 99% of its graduate medical education training programs are sponsored by an affiliate. See U.S. Department of Veterans Affairs, Office of Academic Affiliations, "Medical and Dental Education Program," http://www.va.gov/oaa/gme_default.asp. |
| 11. |
For more information, see U.S. Department of Veterans Affairs, Office of Academic Affiliations, "Advanced Fellowships and Professional Development," http://www.va.gov/oaa/specialfellows/default.asp. |
| 12. |
See CRS Report R44376, Federal Support for Graduate Medical Education: An Overview, coordinated by [author name scrubbed]. |
| 13. |
Department of Veterans Affairs, FY2018 Congressional Budget Submission, Medical Programs and Information Technology Programs, vol. 2 of 4. May 2017, p. VHA-136. |
| 14. |
Until the FY2018 Congressional Budget Submission, the VA presented "direct" and "indirect" training costs as specific purpose funding and general purpose funding respectively under the Veterans Equitable Resource Allocation (VERA) allocation methodology. Beginning with the FY2018 Congressional Submission funding is depicted as "direct" and "indirect" training costs. |
| 15. |
The 2014 Veterans Access, Choice, and Accountability Act of 2014 (P.L. 113-146) initially included a five-year period, that was extended to a ten-year period in 2016 under P.L. 114-315 (i.e., through FY2024). |
| 16. |
U.S. Department of Veterans Affairs, Veterans Health Administration, Office of Academic Affiliations, "Congressional Report: Veterans Access, Choice, and Accountability Act Section 301(b): Increase of Graduate Medical Education Residency Positions at Medical Facilities," September 2017. |
| 17. |
Ibid. |
| 18. |
U.S. Government Accountability Office, Veterans Health Administration: Better Data and Evaluation Could Help Improve Physician Staffing, Recruitment, and Retention Strategies, GAO 18-124, October 19, 2017, p. 8. |