Department of Veterans Affairs: Caregiver Support
The conflicts in Iraq and Afghanistan have presented a new challenge for the United States as servicemembers returned from combat with serious injuries that may have been fatal in previous conflicts. These servicemembers require ongoing personal care services, which are often provided by family members and loved ones. In recognition of this significant challenge, Congress enacted the Caregivers and Veterans Omnibus Health Services Act of 2010 (P.L. 111-163), which required the Department of Veterans Affairs (VA) to establish specific supports for caregivers of veterans.
The Veterans Health Administration (VHA), within VA, offers caregiver support through two programs that were established by the act:
a Program of General Caregiver Support Services (general caregivers program); and
a Program of Comprehensive Assistance for Family Caregivers (family caregivers program).
The general caregivers program offers a basic level of support, such as education and training, to caregivers of veterans of all eras enrolled in VA health care. The family caregivers program offers comprehensive supports, such as health care benefits and a monthly stipend, to caregivers of veterans who were seriously injured in the line of duty on or after September 11, 2001 (post-9/11 veterans). VA refers to these two programs collectively as the Caregiver Support Program.
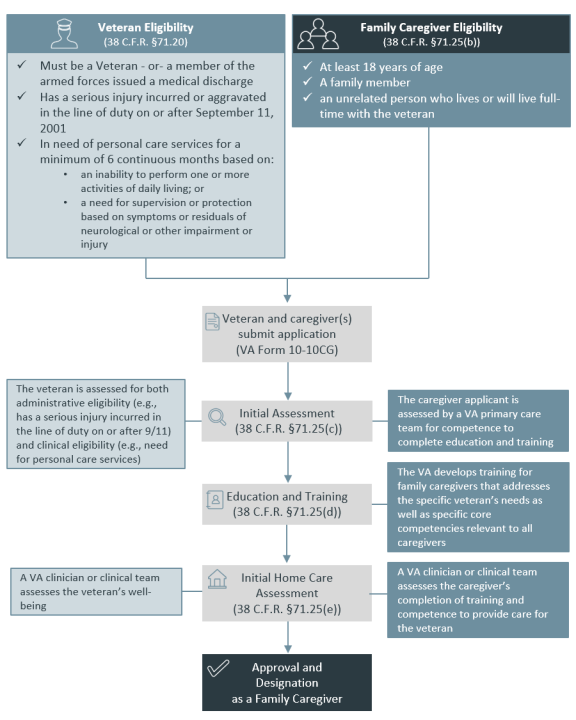
The general caregivers program does not have an application or eligibility determination process. The limited services provided under this program are, generally, available to all caregivers of veterans enrolled in VA health care. Veterans and caregivers who apply for the family caregivers program undergo a multistep eligibility determination process that includes an initial assessment, education, training, and an in-home assessment. VA determines both administrative and clinical eligibility of veterans and caregivers. Caregivers who are eligible and designated as a family caregiver receive a unique suite of comprehensive services and benefits to help them provide care to the veteran.
The VA Maintaining Internal Systems and Strengthening Integrated Outside Networks Act of 2018 (VA MISSION Act; P.L. 115-182, as amended) required VA to expand eligibility for the family caregivers program to caregivers of veterans of all eras. Expansion is being implemented in two phases, as required by the VA MISSION Act. Veterans who were seriously injured in the line of duty before May 7, 1975, are to become eligible first. Two years later, veterans who served and were injured in the line of duty between May 7, 1975, and September 11, 2001, are to become eligible for the program.
This expansion, which has yet to go into effect, is expected to generate a large increase in enrollment and may lead to changes to the underlying structure of the family caregivers program due to a large increase in the number of eligible individuals. Unlike the population currently eligible for the program, this newly eligible population comprises older individuals who may have different disabling conditions that require personal care assistance, which may present a challenge to eligibility determination based on an injury in the line of duty.
Eligibility expansion is contingent on the implementation and certification of a functioning information technology (IT) system required to fully support the program. The VA MISSION Act required that VA complete certification of a system by October 1, 2019. VA did not meet that deadline and has not yet certified an IT system.
VA published a proposed rule to implement the changes required under the VA MISSION Act on March 6, 2020. The public comment period for the proposed rule ends on May 5, 2020.
This report provides an overview of the VA Caregiver Support Program, including
eligibility criteria that veterans and caregivers must meet to qualify for both the family caregivers program and the general caregivers program;
a catalogue of the services and benefits provided under the two programs; and
current issues related to implementation of modifications under the VA MISSION Act.
The Appendix provides background on the program evolution and a legislative history of the program.
Department of Veterans Affairs: Caregiver Support
Jump to Main Text of Report
Contents
- Introduction
- The Caregiver Support Program
- Caregiver Designations and Eligibility for Support
- Eligibility for the General Caregivers Program
- Eligibility for the Family Caregivers Program
- Veteran Eligibility Criteria
- Family Caregiver Eligibility Criteria
- Applying for the Family Caregivers Program
- Ongoing Monitoring and Revocation of Caregiver Status
- Services and Benefits Available to Caregivers
- Services and Benefits for General Caregivers
- Services and Benefits for Secondary Family Caregivers
- Services and Benefits for Primary Family Caregivers
- Caregiver Support Program Administration and Funding
- Caregiver Support Program Administration
- Caregiver Support Program Funding
- Issues for Congress
- IT System Implementation Required for Expansion Is Delayed
- Expansion Is Expected to Increase Costs
Figures
Tables
Summary
The conflicts in Iraq and Afghanistan have presented a new challenge for the United States as servicemembers returned from combat with serious injuries that may have been fatal in previous conflicts. These servicemembers require ongoing personal care services, which are often provided by family members and loved ones. In recognition of this significant challenge, Congress enacted the Caregivers and Veterans Omnibus Health Services Act of 2010 (P.L. 111-163), which required the Department of Veterans Affairs (VA) to establish specific supports for caregivers of veterans.
The Veterans Health Administration (VHA), within VA, offers caregiver support through two programs that were established by the act:
- a Program of General Caregiver Support Services (general caregivers program); and
- a Program of Comprehensive Assistance for Family Caregivers (family caregivers program).
The general caregivers program offers a basic level of support, such as education and training, to caregivers of veterans of all eras enrolled in VA health care. The family caregivers program offers comprehensive supports, such as health care benefits and a monthly stipend, to caregivers of veterans who were seriously injured in the line of duty on or after September 11, 2001 (post-9/11 veterans). VA refers to these two programs collectively as the Caregiver Support Program.
The general caregivers program does not have an application or eligibility determination process. The limited services provided under this program are, generally, available to all caregivers of veterans enrolled in VA health care. Veterans and caregivers who apply for the family caregivers program undergo a multistep eligibility determination process that includes an initial assessment, education, training, and an in-home assessment. VA determines both administrative and clinical eligibility of veterans and caregivers. Caregivers who are eligible and designated as a family caregiver receive a unique suite of comprehensive services and benefits to help them provide care to the veteran.
The VA Maintaining Internal Systems and Strengthening Integrated Outside Networks Act of 2018 (VA MISSION Act; P.L. 115-182, as amended) required VA to expand eligibility for the family caregivers program to caregivers of veterans of all eras. Expansion is being implemented in two phases, as required by the VA MISSION Act. Veterans who were seriously injured in the line of duty before May 7, 1975, are to become eligible first. Two years later, veterans who served and were injured in the line of duty between May 7, 1975, and September 11, 2001, are to become eligible for the program.
This expansion, which has yet to go into effect, is expected to generate a large increase in enrollment and may lead to changes to the underlying structure of the family caregivers program due to a large increase in the number of eligible individuals. Unlike the population currently eligible for the program, this newly eligible population comprises older individuals who may have different disabling conditions that require personal care assistance, which may present a challenge to eligibility determination based on an injury in the line of duty.
Eligibility expansion is contingent on the implementation and certification of a functioning information technology (IT) system required to fully support the program. The VA MISSION Act required that VA complete certification of a system by October 1, 2019. VA did not meet that deadline and has not yet certified an IT system.
VA published a proposed rule to implement the changes required under the VA MISSION Act on March 6, 2020. The public comment period for the proposed rule ends on May 5, 2020.
This report provides an overview of the VA Caregiver Support Program, including
- eligibility criteria that veterans and caregivers must meet to qualify for both the family caregivers program and the general caregivers program;
- a catalogue of the services and benefits provided under the two programs; and
- current issues related to implementation of modifications under the VA MISSION Act.
The Appendix provides background on the program evolution and a legislative history of the program.
Introduction
The Department of Veterans Affairs (VA) Caregiver Support Program was born from a new challenge facing veterans returning from recent conflicts. The conflicts in Afghanistan and Iraq (Operation Enduring Freedom, Operation Iraqi Freedom, and subsequent operations, hereinafter referred to as OEF/OIF)1 led to a growing number of seriously disabled veterans, many of whom require extended care for the remainder of their lives. Some of those seriously injured while serving in these conflicts survived with injuries that would have been fatal in previous conflicts. In the Vietnam Era, five out of every eight seriously injured servicemembers survived. In OEF/OIF, seven out of eight seriously injured servicemembers survived.2
Seriously injured servicemembers returning from OEF/OIF conflicts often sustained polytraumatic injuries3 requiring medically complex care, intensive rehabilitation, and extended or long-term care. Such injuries can include physical injuries (e.g., traumatic brain injuries, amputations, serious burns, spinal cord injuries, and blindness), as well as mental health issues (e.g., posttraumatic stress disorder [PTSD], anxiety, and depression). These types of injuries often have lasting implications for the Department of Defense (DOD) and VA health care and disability systems.
Researchers found that family members and close friends to veterans often shouldered much of the burden in the rehabilitation of returning veterans. Family members and friends relocated for extended periods of time while veterans received treatment in hospital settings.4 Moreover, family and friends often left jobs to act as caregivers for veterans.5
In recognition of this significant challenge to families, Congress enacted the Caregivers and Veterans Omnibus Health Services Act of 2010 (P.L. 111-163), which required VA to establish specific supports for caregivers of veterans. The Veterans Health Administration (VHA), within VA, offers caregiver support through two programs established by the act:
- a Program of General Caregiver Support Services (general caregivers program); and
- a Program of Comprehensive Assistance for Family Caregivers (family caregivers program).
The general caregivers program offers a basic level of support, such as education and training, to caregivers of veterans of all eras enrolled in VA health care. The family caregivers program offers comprehensive supports, such as health care benefits and a monthly stipend, to caregivers of veterans who were seriously injured in the line of duty on or after September 11, 2001. VA refers to these two programs collectively as the Caregiver Support Program.6
The Caregiver Support Program is distinct from other VA programs in that the beneficiary is a nonveteran with some relationship to a living veteran. VA services and benefits are typically provided only to veterans. (VA does provide some services and benefits to families of deceased veterans, with a few exceptions.7) Generally, caregiver services and benefits are available to caregivers only while the veteran receiving care is living.8
After many years of advocacy from veterans organizations, among others, the VA Maintaining Internal Systems and Strengthening Integrated Outside Networks Act of 2018 (VA MISSION Act; P.L. 115-182, as amended) was enacted. It required VA to expand eligibility for supports under the family caregivers program to caregivers of veterans of all eras. Expansion is being implemented in two phases, as required by the VA MISSION Act. Veterans who were seriously injured in the line of duty before May 7, 1975, are to become eligible first. Two years later, veterans who served and were injured in the line of duty between May 7, 1975, and September 11, 2001, are to become eligible for the program.
This expansion, which has yet to go into effect, is expected to generate a large increase in enrollment and may lead to changes to the underlying structure of the family caregivers program due to a large increase in the number of eligible individuals. Unlike the population currently eligible for the program, this newly eligible population is older and may have different disabling conditions that require personal care assistance, characteristics that may present a challenge to determining eligibility based on an injury in the line of duty. (See the text box "Proposed Rule Published on March 6, 2020" for information on a proposed rule to implement requirements under the VA MISSION Act.)
|
Proposed Rule Published on March 6, 2020 VA published a proposed rule to implement the changes required under the VA MISSION Act on March 6, 2020. The public comment period for the proposed rule ends on May 5, 2020.9 This report describes the family caregiver program under current law. In addition to amending current regulations to implement the eligibility expansion required under the VA MISSION Act, the proposed rule would amend a number of definitions under the Caregiver Support Program, alter the formula for stipend payment calculations, and define new benefits. A detailed description of the proposed rule is beyond the scope of this report. |
The Caregiver Support Program
Title I of the Caregivers and Veterans Omnibus Health Services Act of 2010 (P.L. 111-163) includes programs and services to provide support to caregivers of veterans. Specifically, the act amends Title 38, Chapter 17, Subchapter II of the United States Code (U.S.C.) by establishing two programs to assist family caregivers.10 The first is a Program of Comprehensive Assistance for Family Caregivers, for caregivers of eligible veterans who incurred a serious injury in the line of duty while actively serving in the military on or after September 11, 2001 (referred to as the as the family caregivers program in this report). The second is a Program of General Caregiver Support Services, for caregivers of covered veterans of all eras enrolled in the VA health care system (referred to as the general caregivers program in this report). VA refers to the two programs together as the Caregiver Support Program. The Appendix provides a legislative history of the Caregiver Support Program.
Title I of the act also amends Title 38 of the U.S.C. to provide the following services: (1) medical care to certain primary family caregivers; (2) counseling and mental health services to certain family caregivers and other caregivers; and (3) lodging and subsistence for attendants who travel with veterans for medical treatment, regardless of whether they require an attendant for such travel.11
The VA MISSION Act required VA to add additional services to the family caregivers program, to implement a new information technology (IT) system to support the family caregivers program, and to expand eligibility for the program to caregivers of veterans of all eras.
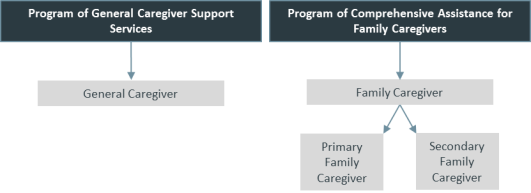
Caregiver Designations and Eligibility for Support
Title I of the Caregivers and Veterans Omnibus Health Services Act of 2010 (P.L. 111-163) creates two caregiver designations: general caregiver and family caregiver. Within the family caregiver designation, the act established a primary designation.12 VA refers to individuals not designated primary as secondary family caregivers.13 Multiple individuals can be designated as a family caregiver for one veteran, hence the primary and secondary designations. Both primary and secondary family caregivers are provided supports through the family caregivers program. General caregivers are provided supports through the general caregivers program. Caregiver designation is conferred based on both the veteran's and the caregiver's eligibility for either of the two programs. Figure 1 shows these caregiver designations under the appropriate VA program.
|
Figure 1. Caregiver Designations VA Caregiver Support Program |
 |
|
Source: Prepared by CRS based on 38 U.S.C. §1720G and 38 C.F.R. §71.15. |
Eligibility for the General Caregivers Program
The general caregivers program does not have a formal application process. Likewise, VA does not require a clinical evaluation to obtain benefits through the general caregivers program.14 A general caregiver may not be a primary or secondary family caregiver, as designated under the family caregivers program, and must provide personal care services to a veteran who is enrolled in the VA health care system and is either
- unable to perform an activity of daily living (ADL), or
- in need of supervision or protection based on symptoms or residuals of neurological or other impairment or injury (supervision or protection).15
The veteran's general caregiver is not required to reside with the veteran.16
To receive services under the general caregivers program, the veteran or the caregiver must contact a local VA medical center. The caregiver is identified in the veteran's medical record for the purpose of care coordination. VA health care providers are required to recognize the caregiver as a collaborative partner in the care of the veteran.17
Eligibility for the Family Caregivers Program
The family caregivers program requires veterans and their caregivers to undergo an eligibility determination process before conferring caregiver designation under the program. Individuals who wish to be designated by VA as primary or secondary family caregivers must complete and sign a joint application with the veteran.18 Figure 2 describes the eligibility requirements that veterans and caregivers must meet before submitting an application, and the process used to determine eligibility after the application is submitted.
Veteran Eligibility Criteria
To qualify for the family caregivers program, an individual must first either (1) meet the statutory definition of a veteran, meaning an individual who served in the active military, naval, or air service and who was discharged or released under conditions other than dishonorable, or (2) be a servicemember who has been issued a date of medical discharge from the military.19
Since the inception of the family caregivers program, the basis of veteran eligibility has been a serious injury incurred in the line of duty on or after September 11, 2001.20 As such, veterans eligible for this program are referred to as post-9/11 veterans. (See the "Issues for Congress" section for information on eligibility for pre-9/11 veterans.) In addition to this post-9/11 requirement, the veteran must have been in need of personal care services21 for a minimum of six continuous months due to either of the following clinical criteria:
- an inability to perform one or more activities of daily living (ADL), or
- a need for supervision or protection based on symptoms or residuals of neurological or other impairment or injury (supervision or protection).22
In addition to those criteria, the veteran's primary care team must determine clinically that it is in the best interest of the veteran to participate in the program. The veteran cannot receive personal care services simultaneously and regularly by another individual or entity who is not the family caregiver. The veteran must agree to receive care at home from the family caregiver and to receive ongoing care from a primary care team after VA designates a family caregiver.
The following section describes the ADLs recognized by VA for the purpose of establishing eligibility for the family caregivers program. The section below that one describes the VA-recognized reasons why a veteran may need supervision or protection; these reasons are based on symptoms or residuals of neurological or other impairment or injury.
Eligibility Based on ADLs
VA considers the following seven ADLs when determining a veteran's eligibility for the family caregiver program:
- 1. Eating. The ability to feed oneself. Specifically, the process of eating, chewing, and swallowing. This does not include preparing food.
- 2. Grooming. The ability to safely tend to personal hygiene needs.
- 3. Bathing. The ability to wash the entire body safely.
- 4. Dressing and undressing. The ability to dress and/or undress the upper and lower body with or without dressing aids.
- 5. Toileting. The ability to maintain perineal hygiene and adjust clothing before and/or after using the toilet or bedpan; the ability to manage an ostomy, including cleaning the area around stoma but not managing equipment;23 or ability to manage urinary catheter or urinal.
- 6. Prosthetic adjustment. The ability to adjust special prosthetic or orthopedic appliances without assistance. The adjustment of appliances that any person (with or without a disability) would need assistance with should not be scored (e.g., supports, belts, lacing at back).
- 7. Mobility. The ability to transfer safely from bed to chair and/or chair to toilet, the ability to turn and position self in bed, the ability to walk safely on a variety of surfaces, and the ability to go upstairs.24
The inability to perform any one of these ADLs for a minimum of six continuous months is a qualifying factor for enrollment in the program.
The VA also tracks a veteran's ability to perform instrumental activities of daily living (IADLs).25 However, IADLs are not considered in the eligibility determination process.
Eligibility Based on Supervision or Protection
VA recognizes seven reasons that a veteran may need supervision or protection under this clinical criterion:
- 1. Seizures. The veteran is unable to manage seizures independently.
- 2. Planning and organizing. The veteran has difficulty planning and organizing daily tasks, appointments, and medication regiments.
- 3. Safety. The veteran is unable to maintain safety with self and others. This may include a risk of falling or wandering.
- 4. Sleep. The veteran has difficulty regulating sleep without intervention.
- 5. Delusions/hallucinations. The veteran is unable to maintain safe behavior in response to delusions (irrational beliefs) or hallucinations (serious disturbances in perception).
- 6. Impairment of recent memory. The veteran has difficulty remembering recent events and learning new information.
- 7. Affective/behavioral dysregulation (self-regulation). The veteran is unable to regulate behavior without exhibiting any of the following behaviors: aggressive or combative with self or others, verbally disruptive including yelling, threatening and excessive profanity, impaired decision making, inability to appropriately stop activities, and disruptive, infantile or socially inappropriate behavior.26
The need for supervision or protection based on any one of these reasons for a minimum of six continuous months is a qualifying factor for enrollment in the program.
Family Caregiver Eligibility Criteria
Under the family caregivers program, a caregiver must be at least 18 years of age, and be either a family member or a person who is living with the veteran or will live with the veteran upon approval.27 An individual is considered a family member if he or she is the eligible veteran's spouse, son, daughter, parent, step-family member, or extended family member.28
Although the family caregiver status includes the term family, the individual is not required to have any familial relationship with the veteran. Furthermore, to apply for the family caregivers program, an individual is not required to currently live with the veteran. The individual simply has to certify that he or she will live with the veteran upon approval as a family caregiver.
Applying for the Family Caregivers Program
If a veteran meets the eligibility criteria for the family caregivers program, he or she is encouraged to apply using VA form 10-10CG.29 The application can either be mailed to the VA Health Eligibility Center or submitted to the caregiver support coordinator at the veteran's local VA medical center.30 The application asks the veteran to identify up to three family caregivers—one primary family caregiver and two secondary family caregivers.
The qualification requirements are the same for the primary or secondary family caregivers. However, primary family caregivers are provided additional benefits, which are listed in Table 1.
After receiving the application, VA evaluates eligibility by identifying the veteran's potential qualifying injury and assessing whether it may render the veteran in need of personal care services. Before the approval and designation of family caregiver(s), the applicant undergoes an initial assessment, education, training, and an initial home care assessment.
The entire VA approval process should be completed within 45 calendar days from the date of submission of an application. The 45-day deadline can be extended if a veteran is hospitalized during the application process or if the caregiver has not completed the required education and training.31
Initial Assessment
A VA primary care team initially assesses each caregiver applicant to confirm that he or she is able to complete caregiver education and training. This initial assessment is completed at a VA medical center. The primary goals of this initial assessment are to assess whether the caregiver applicant can (1) communicate and understand details of the specific care needs related to the veteran and (2) follow a specific treatment plan for the veteran.32
During this initial assessment, the VA primary care team determines whether the veteran is eligible for the program. The team examines administrative eligibility (i.e., whether the veteran is enrolled in the VA health care system and has a documented serious injury that was incurred or aggravated in the line of duty on or after September 11, 2001) and clinical eligibility (i.e., the veterans need for personal care services). The veteran is assigned to a tier level during the clinical evaluation based on the number of hours of personal care services needed.33 (See the text box "Centralized Eligibility and Appeals Teams" for information on how VA is implementing centralized teams to change the eligibility determination process.)
|
Centralized Eligibility and Appeals Teams VA is currently implementing centralized eligibility and appeals teams to conduct the clinical eligibility determination. These teams will replace the veteran's primary care team for eligibility determination. The teams will be located at each Veterans Integrated Service Network (VISN).34 Each team will be led by a physician and staffed by individuals at both the VISN and medical center level. The stated purpose of centralized teams is to standardize the eligibility determination process, tier level adjustments, program revocations, and management of appeals.35 |
During the initial assessment, prospective caregivers are eligible for the Veterans Transportation Service (VTS) program.36 The VTS provides free transportation services to and from a VA medical center.37
Education and Training
Following the initial assessment, VA administers a training program that consists of topics generally applicable to caregivers, as well as topics targeted to the needs of the specific veteran. The training program must cover 10 specific core competencies: medication management, vital signs and pain control, infection control, nutrition, functional activities, activities of daily living, communication and cognition skills, behavior management skills, skin care, and caregiver self-care.38
During this education and training process, prospective caregivers are eligible for either VTS or the VA beneficiary travel program, which reimburses travel expenses related to the veteran's medical appointments. The prospective caregiver can be reimbursed for expenses such as the cost of transport, lodging, and meals.39 In addition, during this period VA provides respite care for the veteran, if necessary.40 (For information on respite care, see the "Services and Benefits for General Caregivers" section.)
Initial Home Care Assessment
The final step before approval and designation is an initial home care assessment. In this step, a VA clinician or clinical team visits the veteran's home to assess whether the caregiver is competent to provide personal care services and to measure the veteran's well-being.41
The clinician or clinical team assesses the veteran's ability to complete ADLs and IADLs, identifies special care needs (e.g., use of a feeding tube), monitors vital signs, looks for signs of abuse or neglect, notes other potential health or safety risks, and screens both the veteran and the caregiver for depression. The clinician or clinical team is not responsible for developing a care plan or for management of the veteran's conditions. However, the clinician or clinical team is responsible for reporting any findings to the veteran's primary care team. The clinician or clinical team can also recommend referrals for follow-up care.42
VA requires that this assessment be completed within 10 days of certification that the caregiver completed the requisite education and training curriculum. If the veteran is hospitalized before the assessment is conducted, VA must conduct the assessment within 10 days from the date the veteran returns home.
Approval and Designation
If the veteran and his or her caregiver(s) are deemed eligible following the initial home care assessment, VA will approve the application and designate the primary and/or secondary family caregivers. Approval of one caregiver is not contingent on the approval of other caregivers listed on the application. For instance, if a veteran designates two caregivers, but only one of the two completed the required training, VA may still approve the individual who completed the training.
VA informs veterans and caregivers deemed ineligible of their ability to appeal the decision. Appeals may be filed at either the local VA facility or at the VISN level.43
Ongoing Monitoring and Revocation of Caregiver Status
Veterans and family caregivers are subject to ongoing monitoring while enrolled in the family caregivers program. VA requires ongoing assessments every 90 days. Assessments can be completed in-person, through video telehealth, or by phone, as well as with an annual in-home visit. The annual visit must be completed in the veteran's home. The purpose of ongoing monitoring is to monitor the veteran's overall health and well-being and adequacy of the personal care services provided by the family caregiver.44
Caregiver status can be revoked immediately if VA determines that the caregiver or the veteran no longer meet eligibility criteria, or if VA makes a clinical determination that having the family caregiver is no longer in the best interest of the veteran. If the family caregiver designation is revoked because the veteran's condition improves—or as the result of the veteran's death or institutionalization—the caregiver will continue to receive benefits for 90 days following the loss of the caregiver designation.45
The family caregiver or the veteran can request that the caregiver designation be revoked. If requested by the caregiver, benefits will terminate immediately upon the date that the caregiver requests revocation.46 If requested by the veteran, the caregiver will continue to receive benefits for 30 days. If the caregiver whose status is being revoked was a primary family caregiver and another primary family caregiver is designated within 30 days, the revoked caregiver's benefits will terminate the day before the new family caregiver is designated as such.47
Services and Benefits Available to Caregivers
Table 1 lists the services and benefits available under the two caregiver support programs (i.e., the Program of General Caregiver Support Services and the Program of Comprehensive Assistance for Family Caregivers). The table also details which of the three categories of caregiver status (i.e., general caregiver, secondary family caregiver, or primary family caregiver) are eligible for the specific service or benefit. The general caregiver category, which confers the least services and benefits, is presented first; followed by the primary family caregiver category, which confers the most services and benefits. In developing Table 1, CRS consulted Title 38 of the Code of Federal Regulations (38 C.F.R. §§71.40 and 71.50), as well as publicly available VHA Directive 1152(1). A detailed description of each service and benefit appears below the table.
|
Benefit |
Explanation of Service or Benefit |
General Caregiver |
Secondary Family Caregiver |
Primary Family Caregiver |
|
Program of General Caregiver Support Services (general caregivers program) |
||||
|
Caregiver Support Line |
Licensed professionals staff the support line to connect caregivers with VA services. The support line also offers monthly telephone education groups. |
X |
X |
X |
|
Peer Support Mentoring |
Caregivers can participate in peer support as both mentors and mentees. This is usually a six-month program, but one-time support is also available. |
X |
X |
X |
|
Education, Training and Technical Support |
VA provides online and in-person education and training offerings to caregivers. VA will also make referrals to non-VA community services. |
X |
X |
X |
|
Telehealtha |
Telehealth allows a veteran's physician or nurse to monitor the veteran's medical condition remotely using home monitoring equipment. This is an indirect benefit to caregivers. |
X |
X |
X |
|
Counseling |
Counseling services are provided to a caregiver if the VA medical professional caring for the veteran determines that the services would further the objectives of the veteran's medical treatment. |
X |
X |
X |
|
Respite Care |
Allows a home health aide to go to a veteran's home to provide personal care services or take a veteran to a program while the caregiver takes a break. The respite care must be medically and age appropriate. It is generally limited to 30 days per calendar year. |
X |
X |
X |
|
Program of Comprehensive Assistance for Family Caregivers (family caregivers program) |
||||
|
Primary Care Team Support and Monitoring |
Ongoing monitoring of a veteran's overall health and well-being and adequacy of care and supervision being provided. |
NE |
X |
X |
|
Mental Health Services |
These services include individual and group therapy, individual counseling, and peer support groups. These services are limited to outpatient care only. |
NE |
X |
X |
|
Beneficiary Travel |
Travel reimbursement during the period when the veteran is traveling to and from medical examination, treatment or care, and for the duration of such examination. |
NE |
X |
X |
|
Stipend |
A monthly stipend payment paid directly to the primary family caregiver. |
NE |
NE |
X |
|
Civilian Health and Medical Program (CHAMPVA)b |
Health insurance program where primary family caregivers obtain medical care from private health care providers. |
NE |
NE |
X |
Source: Prepared by CRS based on Title 38 C.F.R. §§71.40 and 71.50, as well as VHA Directive 1152(1).
Notes: NE = Not Eligible. VA = Department of Veterans Affairs. The statutory authority for all services and benefits is 38 U.S.C. §1720G.
a. For more information, see CRS Report R45834, Department of Veterans Affairs (VA): A Primer on Telehealth.
b. For more information, see CRS Report RS22483, Health Care for Dependents and Survivors of Veterans.
Services and Benefits for General Caregivers
As shown in Table 1, the general caregivers are eligible for various services and benefits: limited to access to the VA caregiver support line; peer mentoring; education, training, and technical support; telehealth; counseling; and respite care. These services and benefits are detailed below.
The caregiver support line is available to general and family caregivers, as well as to any individual who calls to learn more about offered services and eligibility.48 The support line serves as a resource referral center for individuals seeking caregiver information, provides referrals to local VA medical center caregiver support coordinators and other VA or community resources, and provides emotional support to callers.
The caregiver support line also hosts monthly education calls for caregivers. An individual must be a caregiver of a veteran enrolled in VA health care, and participants must register for the call in advance.49 This optional benefit includes courses on managing difficult behavior, self-care, and other topics.
The peer support mentoring program facilitates a mentor/mentee relationship between caregivers. Caregivers can join the program as both mentors and mentees. Mentors receive training and are considered volunteers by VA. This program generally asks mentees to commit to a minimum of six months of mentoring. However, VA also offers one-time connections for caregivers who cannot commit to long-term mentoring but who may need brief support.
VA offers a variety of education, training, and technical support, which includes specific programs such as the Building Better Caregivers program and REACH VA, as well as online tools to assist in caregiving duties.50 This is separate and distinct from the required training that family caregivers must participate in to qualify under the family caregivers program.
Building Better Caregivers is an online workshop that offers weekly lessons, guidance, group support, and access to an alumni community for graduates of the program. The workshops are anonymous to facilitate open communication among caregivers.
REACH VA is an individual coaching program for caregivers designed to help them build skills to take care of themselves and the veterans for whom they are providing personal care services. This program, unlike others available to general caregivers, is available only to caregivers of veterans diagnosed with amyotrophic lateral sclerosis (ALS), dementia, multiple sclerosis (MS), PTSD, or spinal cord injury/disorder. Coaches generally provide four individual hour-long coaching sessions over a period of two to three months. Additional sessions can be provided if the caregiver and coach believe that they will be beneficial.
Telehealth services are provided directly to the veteran. However, they are an indirect benefit to the caregiver, because they allow the veteran to receive medical services without needing a caregiver's assistance in transporting the veteran to medical appointments. Caregivers are able to access VA mobile applications, such as MyHealtheVet, which allows them to view electronic health records, reorder medication, and contact health care providers via secure messaging, among other things.51
The counseling services provided to general caregivers include consultation, professional counseling, marriage and family counseling, training, and mental health services. However, these services are available only if a veteran's medical team determines that the service is "in connection with the treatment" of a veteran's disability.52 In other words, the counseling services may be authorized only if they further the objectives of a veteran's treatment plan. For instance, marriage and family counseling may be provided only if it is intended to address the veteran's mental health. VA clinicians are authorized to refer caregivers to the community for counseling when it is not related to the veteran's treatment.53
Veterans are eligible for 30 days of respite care per calendar year, in general. Respite care is short-term relief for the caregiver, in which another individual acts as the primary caregiver. This care can be provided in an institutional setting or as 24-hour per day in-home care. The respite care must be medically and age-appropriate.54 Respite care can be provided at the home, in a VA community Living Center, through a contracted community skilled nursing home, or through a VA adult day care program.
Services and Benefits for Secondary Family Caregivers
Secondary family caregivers are eligible for the same suite of benefits as general caregivers.55 In addition, veterans under the family caregivers program receive primary care team support and monitoring. Secondary family caregivers receive more comprehensive mental health services and travel reimbursement (described below).
Unlike the counseling services provided to general caregivers, secondary family caregivers can receive mental health services regardless of the medical benefit to the veteran. These services can be provided with the health of the caregiver in mind rather than treatment of the veteran. Services include individual and group therapy, individual counseling, and peer support groups. Mental health services are limited to outpatient care and do not include medication or medication management.56
Secondary family caregivers are eligible for travel reimbursement through the VA Beneficiary Travel program when travel is related to the veteran's medical treatment. Reimbursement is not provided when travel is related solely to the treatment of the caregiver (e.g., travel to a VA medical center for mental health services). To receive travel reimbursement, the veteran must be eligible for the program.57 If eligible, reimbursement includes expenses for lodging and meals, as well as for travel to and from medical appointments.
Services and Benefits for Primary Family Caregivers
Primary family caregivers are eligible for all of the benefits available to both general caregivers and secondary family caregivers.58 In addition to those benefits, primary family caregivers are eligible to receive health care through the Civilian Health and Medical Program of the Department of Veterans Affairs (CHAMPVA) and to receive a monthly stipend based on the number of hours of personal care services that a veteran requires.
Enrollment in the family caregivers program does not confer eligibility for health care services to all primary family caregivers. Individuals must meet additional criteria to be eligible for enrollment in CHAMPVA. Specifically, caregivers must be unable to access any other form of health plan contract, such as health insurance or a state health plan.59 Distinct from VA health care provided to enrolled veterans, CHAMPVA is primarily a health insurance program where individuals receive care from private sector health care providers.60
Caregiver Stipend
In the clinical determination process during the initial assessment, VA assigns veterans to one of three tier levels based on the amount of hours of personal care service required:
- Tier 1. A maximum of 10 hours of caregiver assistance per week.
- Tier 2. A maximum of 25 hours of caregiver assistance per week.
- Tier 3. A maximum of 40 hours of caregiver assistance per week.61
The tier level is used to calculate monthly stipend levels for primary family caregivers. VA determines the monthly value of the stipend by multiplying the hours corresponding to the assigned tier level by the hourly wage for a home health aide, then multiplying the result by 4.35 weeks (the average number of weeks in a month, according to VA). VA uses the 75th percentile hourly wage index for a home health aide for the geographic region in which the veteran and caregiver reside, as determined by the Bureau of Labor Services62 (see the text box "Caregiver Stipend Formula" for the stipend formula).
|
Caregiver Stipend Formula
|
Source: Prepared by CRS based on information from the VA Office of Community Care.
Notes: The hourly wage for a home health aide is the 75th percentile wage for the geographic region in which the veteran and caregiver reside.
The monthly stipend varies based on the assigned tier level and the geographic region in which the veteran and caregiver reside. The 75th percentile hourly wage for home health aides ranges from $8.91 in Ponce, PR, to $36.48 in Santa Rosa, CA, with a median nationwide of $13.00.63 Table 2 provides the average monthly stipend amounts nationwide by tier level.
|
Tier Level |
Monthly Stipend |
|
Tier 1 |
$600 |
|
Tier 2 |
$1,500 |
|
Tier 3 |
$2,500 |
|
All Tiers |
$1,400 |
Source: Prepared by CRS based on VA Assistance and Support Services for Caregivers Annual Report, FY2018.
Despite receiving a stipend, primary family caregivers are not considered VA employees and the stipend is not considered taxable income.64
Caregiver Support Program Administration and Funding
This section details the administrative structure of the Caregiver Support Program and provides historical funding for the program. The narrative explaining the administrative structure of the program is largely adapted from the publicly available VHA Directive 1152(1). The funding history is compiled from VA congressional budget submissions.
Caregiver Support Program Administration
The Caregiver Support Program is administered by a central office within VHA. The Caregiver Support Program Office develops national policy and procedures and provides guidance, oversight, and support to regional and local VA staff regarding caregiver support.65
Two other VA national offices, the Health Eligibility Center (HEC) and the Office of Community Care, perform significant roles in administration of the Caregiver Support Program. The HEC is responsible for processing applications for the family caregiver program. The Office of Community Care calculates and processes stipend payments for family caregivers and administers enrollment and claims processing for family caregivers in CHAMPVA.66
Regionally, each VISN ensures that every medical center within the VISN employs at least one full-time equivalent Caregiver Support Coordinator and that the program is operated consistently across the VISN.67 The VISN also maintains a process for appeals related to clinical disputes, which includes independent external review. The VISN employs a clinical staff member as a VISN lead for the Caregiver Support Program.68
The VISN lead acts as an intermediary between the central office and the Caregiver Support Coordinators at the local level. The VISN lead provides guidance and support to the Caregiver Support Coordinators within the VISN.
The caregiver support coordinator administers the program locally at each VA medical center. The coordinator is responsible for managing the family caregiver program at the operational level by coordinating the application process, the initial home care assessment, and ongoing monitoring. The individual also acts as an advocate for caregivers and veterans internally by ensuring that services and benefits are available, as well as by creating educational tools and developing programs.69 VA has mandated that each medical center have at least one full-time equivalent caregiver support coordinator.
Caregiver Support Program Funding
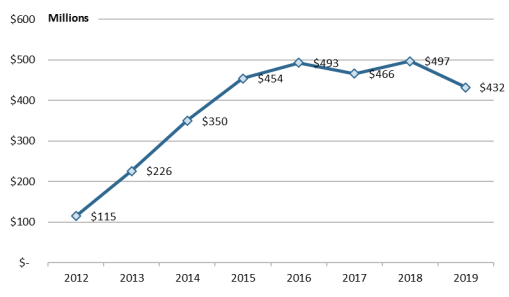
VA began reporting actual operating expenditures for the Caregiver Support Program in its annual budget submissions in FY2012. Figure 3 shows actual expenditures for FY2012 through FY2019. Between FY2012 and FY2015—the first years of implementation of the Caregiver Support Program—expenditures grew by 41.0% annually. Since FY2015, expenditures for the program have stabilized substantially. Between FY2015 and FY2018, expenditures grew by 2.3% annually. In FY2019, expenditures were lower than anticipated, decreasing by 13% from expenditures in FY2018. VA has indicated that decreasing enrollment in recent years may be due to decreasing application approval rates and increases in revocations for veterans and caregivers who do not meet eligibility requirements.70
The monthly stipend for primary family caregivers in the family caregivers program comprises the largest portion of spending under the Caregiver Support Program. In FY2019, for instance, stipend payments totaled approximately $347 million, or 79% of total program expenditures.71
Expansion of the family caregiver program to pre-9/11 veterans is expected to significantly increase demand for the program. VA has factored this expected increase into future budget estimates. VA estimates that the program will cost $710 million in FY2020 and nearly $1.2 billion in FY2021.72
Issues for Congress
Title 1 of the VA MISSION Act expands eligibility for the family caregiver program to pre-9/11 veterans in two phases. This expanded eligibility depends on certification of a new information technology (IT) system to administer the program:
- Phase 1. Veterans who have a serious injury incurred or aggravated in the line of duty in the active military, naval, or air service on or before May 7, 1975.
- Phase 2. Two years after certification, the program is to expand to cover veterans of all eras.73
Expanding eligibility for the Caregiver Support program raises two potential issues: (1) delays in implementation of an IT system to fully support the system and (2) increased costs associated with eligibility expansion under the act. As program eligibility expands, these issues may be of interest to policymakers.
In addition to these two issues, the program may change in other significant ways when VA modifies the regulations necessary to implement the eligibility expansion. VA published a proposed rule to implement the changes required under the VA MISSION Act on March 6, 2020. The public comment period for the proposed rule ends on May 5, 2020.74 Furthermore, rulemaking to add the expansion populations must be finalized, at the very least, prior to expansion becoming effective.
IT System Implementation Required for Expansion Is Delayed
The act required VA to implement a new IT system to fully support the family caregiver program by October 1, 2018—nearly four months after the legislation was enacted. The IT system must be able to (1) retrieve the data needed to assess and monitor program and workload trends, (2) manage data for program participation that exceeds VA estimates, and (3) integrate the system with other VHA IT systems.75
The act required VA to certify that the system had been implemented no later than October 1, 2019. The first phase of eligibility expansion is to become effective when the IT system is certified. However, VA has not yet certified an IT system.
Prior to enactment of the VA MISSION Act, the IT system used to support the family caregivers program, the Caregiver Application Tracker (CAT), was deemed inadequate. Specifically, limitations with CAT did not grant the Caregiver Support Program office ready access to the workload data needed to monitor the effects of the program on VA medical center resources.76 VA attempted to add functionality to CAT in a project called CAT Rescue. However, CAT Rescue was terminated in April 2018 after VA reported defects during system testing.
When the VA MISSION Act was enacted, VA was in the midst of replacing CAT with a new IT system, called the Caregivers Tool (CareT). This project began in September 2015. However, VA identified deficiencies in CareT during acceptance testing and terminated the project in February 2019.77
In March 2019, VA began a third effort to acquire a replacement system, which is based on an existing commercial product. The new system is referred to as the Caregiver Record Management Application (CARMA).
VA is deploying CARMA in three phases. The first phase replaced CAT with CARMA and was completed in October 2019. The second phase automated stipend processing within CARMA and was completed in January 2020. The third phase is expected to be completed in summer 2020. In this third phase, VA is updating other legacy systems, enabling online application submission, and enhancing reporting functionality (e.g., business analytics tools). VA has indicated that it expects to certify the system at the completion of phase 3 and the first eligibility expansion will occur at that time.78 Figure 4 illustrates a timeline of VA initiatives designed to replace the current IT system that supports the program and requirements of the VA MISSION Act.
|
Figure 4. IT Replacement Timeline and VA MISSION Act Requirements Program of Comprehensive Assistance for Family Caregivers |
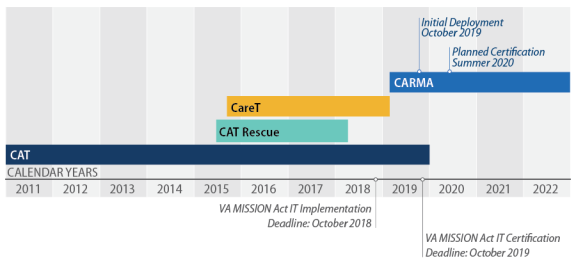 |
|
Source: Figure prepared by CRS based on a figure titled "Timeline of the Veterans Affairs' Family Caregiver Program's IT System Update and Replacement Projects" in U.S. Government Accountability Office, VA Health IT: Use of Acquisition Best Practices Can Improve Efforts to Implement a System to Support the Family Caregiver Program, GAO-190-581T, May 2019. Additional information is based on P.L. 115-182 and VA communications indicating a certification date for CARMA. Notes: IT = Information Technology; VA MISSION Act = The VA Maintaining Internal Systems and Strengthening Integrated Outside Networks Act of 2018 (VA MISSION Act; P.L. 115-182, as amended); CAT = Caregiver Application Tracker; CareT = Caregivers Tool; CARMA = Caregiver Record Management Application. |
Expansion Is Expected to Increase Costs
The family caregivers program currently serves approximately 20,000 post-9/11 veterans and their caregivers. When the first phase of expansion begins, to pre-9/11 veterans injured in the line of duty before May 7, 1975, VA projects that approximately 83,000 additional veterans and their caregivers will become eligible for the program.79 The number of eligible veterans and caregivers would potentially continue to grow when eligibility expands to all pre-9/11 veterans.
The largest cost driver in the family caregivers program is the monthly stipend to family caregivers. In FY2019, stipend payments totaled approximately $347 million, or 79% of total program expenditures. With expansion of the magnitude projected by VA, the number of caregivers receiving monthly stipends will increase. VA estimates that expenditures for the stipend will total $870 million in FY2021 and nearly $1.2 billion in FY2022.80
As the program expands, other program components may require additional resources to meet the demand resulting from the increased numbers of eligible veterans and caregivers. For instance, as it is currently structured, the program requires ongoing monitoring in a veteran and caregiver's home. In general, a VA clinical team that includes at least two individuals must visit each home on at least an annual basis. To continue to meet this requirement, VA will likely need to increase staffing levels to conduct similar program monitoring and oversight.81
VA requested nearly $1.2 billion in FY2021 (the first full year implementation of phase 1 of the eligibility expansion), a 276% increase from FY2019 (the last full year in which eligibility was available only to post-9/11 veterans). The FY2022 advance appropriation request is $1.5 billion, which represents only a partial year of implementation of phase 2 of the eligibility expansion.
Appendix. Program Evolution and Legislative History
Program Evolution
As military operations in Afghanistan and Iraq progressed, the provision of services and supports to family caregivers of veterans seriously injured in these conflicts moved to the forefront. Family caregiver issues became a focus of the President's Commission on Care for America's Returning Wounded Warriors, established by President G.W. Bush on March 8, 2007.82 Tasked with providing a comprehensive review of the care provided to injured servicemembers returning from the recent conflicts in Afghanistan and Iraq, the commission issued several recommendations to the President, Congress, DOD, and VA in a final report. Among these recommendations were several DOD and VA recommendations to strengthen family support programs, including providing "families of servicemembers who require long-term personal care with appropriate training and counseling to support them in their new caregiving roles."83
VA Advisory Committee on OEF/OIF Veterans and Families
In April 2007, VA established an independent advisory committee to assess the situation of OEF/OIF veterans and families.84 The committee was tasked with examining existing VA benefits and services and the need for new benefits and services tailored to OEF/OIF veterans. Committee membership included representation from veterans, family members, and caregivers, as well as veteran service organizations and other advocates and specialists. In 2008, the committee issued an interim report with preliminary observations and recommendations that centered around several themes, including family and caregivers.85 The Advisory Committee's recommendations, among others, were to increase support to families and caregivers. Specifically, the committee's recommendations and findings consisted of three priorities for caregivers: (1) mental health counseling services for those caregiving for severely injured veterans, particularly over a prolonged time period; (2) financial counseling and fiscal support while caring for severely disabled veterans, as well as training programs; and (3) enhanced efforts regarding information and education about available VA benefits and services.
In June 2008, VA established an interdisciplinary Caregiver Advisory Board to develop a caregiver assistance program. The board's chartered activities include identifying core caregiver needs, developing initial recommendations for VA caregiver support services, and overseeing eight caregiver assistance pilot programs.86 The pilot programs were conceptualized in December 2007 to examine ways to improve education and to provide training and resources for caregivers assisting veterans.87 Most of the programs focus on supporting caregivers of veterans with specific conditions, such as dementia and traumatic brain injury. These pilot programs were conducted through the end of FY2009.
Caregivers and Veterans Omnibus Health Services Act of 2010
Leading up to enactment of the Caregivers and Veterans Omnibus Health Services Act of 2010 (P.L. 111-163), the 111th Congress engaged in considerable debate and deliberation about various legislative proposals to assist family caregivers of veterans. The following provides a legislative history of significant proposals to address assistance to family caregivers of veterans and, more specifically, veterans injured in the conflicts in Afghanistan and Iraq.88 This history begins with legislation first enacted in the 109th Congress to address greater services and support to family caregivers and ends with passage of the Caregivers and Veterans Omnibus Health Services Act of 2010 in the 111th Congress.
The initial congressional response to providing assistance to family caregivers of veterans from recent conflicts in Iraq and Afghanistan dates back to the 109th Congress. On May 4, 2006, S. 2753 was introduced by Senator Daniel Akaka. The bill would have required a VA program to improve the provision of caregiver assistance services for veterans. Although the bill did not necessarily focus on caregiving assistance to veterans serving in recent conflicts, but rather all veterans, in his introductory speech Senator Akaka stated:
With more veterans returning from combat with severely debilitating injuries, young spouses and parents have been forced to take on an unexpected role as caregivers. Many have interrupted their own careers to dedicate time and attention to the care and rehabilitation of loved ones. These caregivers do not plan for this to happen and are not prepared mentally or financially for their new role. Therefore, we must protect, educate, and lend a helping hand to the caregivers who take on the responsibility and costly burden of caring for veterans, both young and old. This legislation serves to provide comprehensive assistance to these caregivers.89
Provisions from S. 2753 were included as Section 214 of the Veterans Benefits, Healthcare, and Information Technology Act of 2006 (P.L. 109-461) and enacted on December 22, 2006. P.L. 109-461 authorized VA to conduct a two-year pilot program to improve assistance provided to caregivers, particularly in home-based settings, and authorized $5 million to be appropriated for each of FY2007 and FY2008. The 110th Congress extended authorization of the caregiver assistance pilot programs through the end of FY2009 under Section 809 of the Veterans' Mental Health and Other Care Improvements Act of 2008 (P.L. 110-387).
Assistance to family caregivers received further legislative attention in the 111th Congress, with legislative proposals introduced to specifically target caregivers of veterans injured while serving in OEF/OIF. In the Senate, Senator Akaka introduced the Family Caregiver Program Act of 2009 (S. 801) on April 2, 2009.90 In his introductory remarks, Senator Akaka stated:
Some veterans returning from the recent wars in Iraq and Afghanistan, as well as previous conflicts, suffer from disabilities that prevent them from being fully independent. This is a sad fact of war. The legislation I am introducing today is designed to provide for several improvements in health care for veterans by supporting the family members who care for them. The challenges faced by family caregivers are well known to us. We have been working on this issue for nearly two years … I think we are now beyond the scope of that original pilot program and I believe that a full-fledged permanent program is needed in VA that would have a national program for the caregivers of seriously injured veterans to provide them with education, grants, counseling, and other support services. 91
An amended version of S. 801 was reported by Senator Akaka on September 29, 2009 (S.Rept. 111-80). The amended version would have, among other things, authorized VA to waive the cost of emergency care for caregivers of veterans; created a comprehensive program to provide assistance to the caregivers of severely injured veterans; authorized VA to pay for the caregivers' lodging and subsistence, as well as the expenses of travel for the period consisting of travel to and from a treatment facility and the duration of a treatment episode at that facility; and required VA to collaborate with DOD to conduct a national survey of family caregivers.
The House also introduced legislation that would specifically provide assistance to caregivers of OEF/OIF veterans. On July 9, 2009, Representative Michael H. Michaud introduced the Caregiver Assistance and Resource Enhancement Act (H.R. 3155). On July 15, 2009, H.R. 3155 as amended, was ordered reported out of the House Veterans' Affairs Committee (H.Rept. 111-224). The bill was then passed by the House on July 27, 2009. As passed by the House, H.R. 3155 would have required VA to provide support services (including CHAMPVA medical care and stipends) to the eligible caregivers of OEF and OIF veterans. To be eligible, veterans would need to meet three conditions: (1) have a severe service-connected disability or illness; (2) be in need of caregiver services, such that without such services, the veteran would require hospitalization, nursing home care, or other residential institutional care; and (3) be unable to carry out the activities of daily living (including instrumental activities of daily living).92
A "hold" was placed on S. 801 that prevented the Senate from considering this measure. Subsequently, on October 28, 2009, Senator Akaka introduced a separate bill, the Caregivers and Veterans Omnibus Health Services Act of 2010 (S. 1963), which included provisions from S. 801, among other provisions. S. 1963 was passed by the Senate on November 11, 2009. The family caregiver provisions in the Senate-passed bill would have waived charges for humanitarian care to attendants of covered veterans under certain circumstances; provided family caregiver assistance including training, respite care, mental health services, and stipends; and provided lodging and subsistence for family caregivers. It would have also required VA, in coordination with DOD, to design and conduct a survey on caregivers and family caregivers.
On April 22, 2010, an amended version of S. 1963 was passed by Congress. The final version reflected a compromise agreement between the House and the Senate and included provisions derived from a number of bills, including the earlier Senate-passed S. 1963 and House-passed H.R. 3155. On May 5, 2010, President Obama signed into law P.L. 111-163, the Caregivers and Veterans Omnibus Health Services Act of 2010. Title I of the act provides programs and services to provide support to caregivers of veterans.
Following enactment of the 2010 legislation that established the Caregiver Support Program, there were a number of legislative attempts to expand eligibility for the Program of Comprehensive Assistance for Family Caregivers to veterans of all eras. This effort ultimately culminated with the enactment of the VA Maintaining Internal Systems and Strengthening Integrated Outside Networks Act of 2018 (VA MISSION Act; P.L. 115-182, as amended).93
Author Contact Information
Acknowledgments
Jamie Hutchinson, CRS Visual Information Specialist, provided invaluable assistance with the graphics in this report.
Footnotes
| 1. |
Since the September 11, 2001, terrorist attacks, the Department of Defense (DOD) has been engaged in domestic and overseas military operations. For more information on the specific conflicts that followed, see CRS Report RS21405, U.S. Periods of War and Dates of Recent Conflicts. |
| 2. |
President's Commission on Care for America's Returning Wounded Warriors, Serve, Support, Simplify: Report of the President's Commission on Care for America's Returning Wounded Warriors, June 2007, p. 2. |
| 3. |
VA defines polytrauma "as two or more injuries sustained in the same incident, one of which may be life threatening, which affect multiple body parts and organ systems and result in physical, cognitive, emotional, and behavioral impairments and functional disabilities." Department of Veterans Affairs, Veterans Health Administration, Caregiver Support Program, VHA Handbook 1172.01, Washington, DC, January 24, 2019, p. 1. |
| 4. |
Commission on Care for America's Returning Wounded Warriors, Serve, Support, Simplify: Report of the President's Commission on Care for America's Returning Wounded Warriors, June 2007, p. 9. |
| 5. |
Ibid. |
| 6. |
Department of Veterans Affairs, Veterans Health Administration, Caregiver Support Program, VHA Directive 1152(1), Washington, DC, October 4, 2018, p. 1. |
| 7. |
The Civilian Health and Medical Program (CHAMPVA), readjustment counseling and related mental health services, and certain education benefits are available to family members of living veterans. |
| 8. |
If the veteran receiving care dies, the caregiver continues to receive benefits for 90 days after the veteran's death. For more information, see 38 C.F.R. §71.45(c). |
| 9. |
The proposed rule is available at https://www.regulations.gov/docket?D=VA-2020-VHA-0010. The VA press release announcing the proposed rule is available at https://www.va.gov/opa/pressrel/pressrelease.cfm?id=5398. |
| 10. |
38 U.S.C. §1720G. |
| 11. |
38 U.S.C. §§1720G(a)(3)(A)(ii)(IV); 1720G(a)(3)(A)(i)(III); and 1720G(a)(3)(A)(i)(IV). |
| 12. |
38 U.S.C. §1720G(a)(7)(A), 38 U.S.C. §1720G(b)(1), and 38 C.F.R. §71.30. |
| 13. |
38 C.F.R. §71.15. |
| 14. |
38 C.F.R. §71.30(c). |
| 15. |
For more information on ADLs, see the "Eligibility Based on ADLs" section. For more information on supervision or protection, see the "Eligibility Based on Supervision or Protection" section. |
| 16. |
38 C.F.R. §71.30. |
| 17. |
Department of Veterans Affairs, Veterans Health Administration, Caregiver Support Program, VHA Directive 1152(1), Washington, DC, October 4, 2018, pp. 20-21. |
| 18. |
VA Form 10-10CG. Application for Comprehensive Assistance for Family Caregivers Program. For more information, see https://www.va.gov/health-care/forms/vha-10-10CG.pdf. |
| 19. |
38 U.S.C. §1720G(a)(2)(A). The term serious injury includes traumatic brain injury, psychological trauma, or other mental disorder. |
| 20. |
38 U.S.C. §1720G(a)(2)(B). |
| 21. |
As defined in 38 U.S.C. §1720G(d)(4), personal care services mean assistance with one or more activities of daily living, supervision or protection based on symptoms or residuals of neurological or other impairment or injury, regular or extensive instruction or supervision without which the ability of the veteran to function in daily life would be seriously impaired, or any other noninstitutional extended care. |
| 22. |
The regulatory framework for the family caregivers program lists two more qualifying clinical criteria for the need for personal care services. The first additional criterion is the existence of a psychological trauma or a mental disorder that has been scored by a licensed mental health professional, with a Global Assessment of Functioning (GAF) score of 30 or less. The Global Assessment of Functioning is a well-established mental health examination that uses a score of zero to 100 to determine an individual's ability to function psychologically and socially. An individual who has been assessed as having a psychological trauma or mental disorder and has been scored at 30 or less generally requires a higher level of care that would include constant supervision. VA stopped using the GAF to determine eligibility when it was not included in the most recent iteration of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5). The second additional clinical criterion is that the veteran has been rated 100% service-connected disabled for a qualifying serious injury and has been awarded special monthly compensation that includes an aid and attendance allowance. In practice, this criterion is not considered independently from the two detailed in this section. For more information, see 38 C.F.R. §71.20(c). |
| 23. |
An ostomy is an opening from an area inside the body to the outside. A stoma is the opening created during the ostomy. For more information, see https://medlineplus.gov/ostomy.html. |
| 24. |
Department of Veterans Affairs, Veterans Health Administration, Caregiver Support Program, VHA Directive 1152(1), Washington, DC, October 4, 2018, p. 2. |
| 25. |
Examples of IADLs include the ability to prepare meals, conduct housework, shop, use transportation, use the telephone, manage medications, and manage finances. |
| 26. |
Ibid., pp. 3-4. |
| 27. |
38 C.F.R. §71.25(b). |
| 28. |
38 C.F.R. §71.25(b)(i). |
| 29. |
For more information, see https://www.va.gov/health-care/forms/vha-10-10CG.pdf. |
| 30. |
Applications are mailed to Health Eligibility Center, 2957 Clairmont Road, Suite 200, Atlanta, GA 30329. |
| 31. |
38 C.F.R. §71.40(d). |
| 32. |
38 C.F.R. §71.40(c) and Department of Veterans Affairs, Veterans Health Administration, Caregiver Support Program, VHA Directive 1152(1), Washington, DC, October 4, 2018, p. 13. |
| 33. |
U.S. Government Accountability Office, VA Health Care: Actions Needed to Improve Family Caregiver Program, GAO-19-618, September 2019, p. 11, https://www.gao.gov/assets/710/701396.pdf. |
| 34. |
The VA health care system is divided into administrative regions, called Veterans Integrated Service Networks (VISN), based on geography. There are currently 18 VISNs, which vary regarding the number of sites of care, the types and number of facilities, and the geographic size of the network's region. For more information, see CRS In Focus IF10555, Introduction to Veterans Health Care. |
| 35. |
Department of Veterans Affairs, FY2021 Congressional Submission, Medical Programs and Information Technology Programs, vol. 2 of 4, February 2020, p. VHA-101. |
| 36. |
38 C.F.R. §70.71(e)(1). |
| 37. |
For more information on the VTS, see https://www.va.gov/HEALTHBENEFITS/vtp/veterans_transportation_service.asp. |
| 38. |
38 C.F.R. §71.25(d). |
| 39. |
For more information on the VA Beneficiary Travel Program, see https://www.va.gov/health-care/get-reimbursed-for-travel-pay/. |
| 40. |
Department of Veterans Affairs, Veterans Health Administration, Caregiver Support Program, VHA Directive 1152(1), Washington, DC, October 4, 2018, p. 14. |
| 41. |
Ibid., p. 14. |
| 42. |
This information is based on the Department of Veterans Affairs, Caregiver Support Program Initial In-Home Assessment Worksheet. |
| 43. |
Each VA medical center and each VISN establishes procedures for appeals of clinical decisions based on guidance in VHA Directive 1041, Appeal of VHA Clinical Decisions. |
| 44. |
Department of Veterans Affairs, Veterans Health Administration, Caregiver Support Program, VHA Directive 1152(1), Washington, DC, October 4, 2018, p. 16. |
| 45. |
38 C.F.R. §71.45(c). |
| 46. |
38 C.F.R. §71.45(a). |
| 47. |
38 C.F.R. §71.45(b). |
| 48. |
The caregiver support line can be reached by calling 855-260-3274. The line is open daily from 8:00 a.m. to 8:00 p.m. (EST). |
| 49. |
For more information, see https://www.caregiver.va.gov/help_landing.asp. |
| 50. |
The Caregiver Support Program offers a number of online tools, such as medication logs, tips on talking to providers, and self-care guides. For more information, see https://www.caregiver.va.gov/tips_tools.asp. |
| 51. |
VA telehealth encompasses multiple components in addition to access to mobile applications. For more information, see CRS Report R45834, Department of Veterans Affairs (VA): A Primer on Telehealth. |
| 52. |
38 C.F.R. §71.50(a). |
| 53. |
38 C.F.R. §71.50(c). |
| 54. |
For more information on respite care and other long-term care services provided through VA, see CRS Report R44697, Long-Term Care Services for Veterans (archived). |
| 55. |
38 C.F.R. §71.40(b)(1). |
| 56. |
Department of Veterans Affairs, Veterans Health Administration, Caregiver Support Program, VHA Directive 1152(1), Washington, DC, October 4, 2018, p. 15. |
| 57. |
For information on eligibility for VA Beneficiary Travel, see 38 C.F.R. §70.10. |
| 58. |
38 C.F.R. §71.40(c)(1). |
| 59. |
For more information on health-plan contracts, see 38 U.S.C. §1725(f). |
| 60. |
For more information on CHAMPVA, see CRS Report RS22483, Health Care for Dependents and Survivors of Veterans. For more information on the VA health system and health care for veterans, see CRS Report R42747, Health Care for Veterans: Answers to Frequently Asked Questions. |
| 61. |
38 C.F.R. §71.40(c)(iv). For more information, see VA Fact Sheet 11-02: Caregiver Support Program – Stipend Benefit for the Primary Family Caregiver, https://www.va.gov/COMMUNITYCARE/docs/pubfiles/factsheets/FactSheet_11-02.pdf. |
| 62. |
The Bureau of Labor Services Standard Occupational Code for home health aide is 311011. |
| 63. |
These figures are based on wage data provided by the Bureau of Labor Services for May 2018. |
| 64. |
38 C.F.R. §71.40(c)(4)(vii). |
| 65. |
Department of Veterans Affairs, Veterans Health Administration, Caregiver Support Program, VHA Directive 1152(1), Washington, DC, October 4, 2018, p. 4. |
| 66. |
Ibid., p. 5. |
| 67. |
The VA health care system is divided into administrative regions, called Veterans Integrated Service Networks (VISN), based on geography. There are currently 18 VISNs, which vary regarding the number of sites of care, the types and number of facilities, and the geographic size of the network's region. For more information, see CRS In Focus IF10555, Introduction to Veterans Health Care. |
| 68. |
Department of Veterans Affairs, Veterans Health Administration, Caregiver Support Program, VHA Directive 1152(1), Washington, DC, October 4, 2018, pp. 6-7. |
| 69. |
Ibid., pp. 9-10. |
| 70. |
Department of Veterans Affairs, Economic Regulatory Impact Analysis for RIN 2900-AQ48(P), Program of Comprehensive Assistance for Family Caregivers Improvements and Amendments under the VA Mission Act of 2018, March 4, 2020, p. 29. |
| 71. |
Department of Veterans Affairs, FY2021 Congressional Submission, Medical Programs and Information Technology Programs, vol. 2 of 4, February 2020, p. VHA-43. |
| 72. |
Ibid., p. VHA-99. |
| 73. |
38 U.S.C. §1720G(a)(2). |
| 74. |
The proposed rule is available at https://www.regulations.gov/docket?D=VA-2020-VHA-0010. |
| 75. |
38 U.S.C. §1720G note. |
| 76. |
U.S. Government Accountability Office, VA Health Care: Actions Needed to Address Higher-Than-Expected Demand for the Family Caregiver Program, GAO-14-675, September 2014, p. 21, https://www.gao.gov/assets/670/665928.pdf. |
| 77. |
U.S. Government Accountability Office, VA Health IT: Use of Acquisition Best Practices Can Improve Efforts to Implement a System to Support the Family Caregiver Program, GAO-190-581T, May 2019, p. 7, https://www.gao.gov/assets/700/699259.pdf. |
| 78. |
Department of Veterans Affairs, "VA strengthens Caregiver Support Program and expands timeline of the Program of Comprehensive Assistance for Family Caregivers," press release, September 25, 2019, https://www.va.gov/opa/pressrel/pressrelease.cfm?id=5319. |
| 79. |
This projection was provided in VA briefing materials. |
| 80. |
Department of Veterans Affairs, FY2021 Congressional Submission, Medical Programs and Information Technology Programs, vol. 2 of 4, February 2020, p. VHA-43. |
| 81. |
Ibid., p. VHA-99. |
| 82. |
Executive Order 13426, "Establishing a Commission on Care for America's Returning Wounded Warriors and a Task Force on Returning Global War on Terror Heroes," 72 Federal Register 10589, March 8, 2007. |
| 83. |
Commission on Care for America's Returning Wounded Warriors, Serve, Support, Simplify: Report of the President's Commission on Care for America's Returning Wounded Warriors, June 2007, p. 10. |
| 84. |
Post-9/11 veterans are also referred to as OEF/OIF veterans. |
| 85. |
Department of Veterans Affairs, Interim Report of Department of Veterans Affairs Advisory Committee on Operations Iraqi Freedom and Operations Enduring Freedom Veterans and Families, June 2008. |
| 86. |
U.S. Government Accountability Office, VA Family and Education Support, GAO-09-22R, October 22, 2008. |
| 87. |
The Veterans Benefits, Health Care, and Information Technology Act of 2006 (P.L. 109-461) required VA to establish a pilot program to assess various ways to expand and improve caregiver assistance. |
| 88. |
Legislation included in this section was either introduced by the Chairman of the respective committee or subcommittee or was reported out of full committee. |
| 89. |
"Statements on Introduced Bills and Joint Resolutions," Remarks in the Senate, Congressional Record, daily edition, vol. 152 (May 4, 2006), p. S4075. |
| 90. |
On May 11, 2009, a comparable measure to S. 801 was introduced in the House by Representative Michael Michaud, titled the Warrior Project Family Caregiver Act of 2009 (H.R. 2342). Several other measures were also introduced in the 111th Congress to provide assistance to family caregivers. These include, among others, the Health Care for Family Caregivers Act of 2009 (H.R. 2734), the Wounded Warrior Caregiver Assistance Act (H.R. 2898), and the Veteran and Servicemember Caregiver Support Act of 2009 (S. 543). |
| 91. |
"Statements on Introduced Bills and Joint Resolutions," Remarks in the Senate, Congressional Record, daily edition, vol.155 (April 2, 2009), p. S4350. |
| 92. |
Several other measures were also introduced in the 111th Congress to provide assistance to family caregivers of veterans. These include, among others, the Health Care for Family Caregivers Act of 2009 (H.R. 2734), the Wounded Warrior Caregiver Assistance Act (H.R. 2898), and the Veteran and Servicemember Caregiver Support Act of 2009 (S. 543). |
| 93. |
For additional information on the VA MISSION Act, see CRS Report R45390, VA Maintaining Internal Systems and Strengthening Integrated Outside Networks Act of 2018 (VA MISSION Act; P.L.115-182). |