Department of Veterans Affairs (VA): A Primer on Telehealth
The Veterans Health Administration (VHA), of the Department of Veterans Affairs (VA), is leveraging the use of telehealth with the goal of expanding veterans’ access to VA care. Telehealth generally refers to the use of information and communication technology to deliver a health care service. It is a mode of health care delivery that extends beyond the “brick-and-mortar” health care facilities of the VHA. VA telehealth services are generally provided on an outpatient basis and supplement in-person care. Such services do not replace VA in-person care. The VA copay requirements for telehealth are the same as for VA in-person care, but in some cases may be lower than the copays for VA in-person outpatient health care services delivered through the VHA. President Trump and Congress have recently enacted measures such as the VA Maintaining Internal Systems and Strengthening Integrated Outside Networks of 2018 (VA MISSION Act; P.L. 115-182) that aim to address the access barriers that veterans may experience when accessing VA telehealth services across states lines. The VA MISSION Act, among other things, removes all geographic and licensing barriers to VA telehealth, thereby allowing veterans to access VA telehealth services in their communities from any location in the United States, U.S. territories, District of Columbia, and Commonwealth of Puerto Rico.
VA Telehealth Modalities
In FY2018, more than 9.3 million veterans were enrolled in VA care. In that same fiscal year, the VA provided 2.29 million telehealth episodes of care to 782,000 veteran patients collectively using the following three VA telehealth modalities: (1) home telehealth, (2) store-and-forward telehealth, and (3) clinical video telehealth. The VA has developed VA mobile applications (apps), which refer to software programs that run on certain operating systems of mobile devices (e.g., smartphones and tablets) and computers that transmit data over the internet that veterans can access as telehealth applications. Veterans can access VA mobile apps on cellular and mobile devices that operate using either a web-based platform, an iOS platform, or an Android operating platform.
VA Telehealth Partnerships and Access
According to the VA, it cannot meet the health care demands of veteran patients in-house and therefore, it has established partnerships with private sector vendors to help address veterans’ demand for VA care. For example, the VA’s partnership with the wireless service provider T-Mobile would allow a veteran who has T-Mobile as a cellular wireless service provider to access the VA Video Connect app without incurring additional charges or reducing plan data allotments.
VA Teleconsultations
VA providers can use telehealth platforms and applications to consult with one another, which is referred to as a teleconsultation by section 1709A(b) of title 38 of the U.S. Code. The VA has adopted and modified the Project Extension for Community Healthcare Outcomes (Project ECHO) learning model, which the Expanding Capacity for Health Outcomes Act (P.L. 114-270) required the Secretary of the Department of Health and Human Services to examine and report on, to create a Specialty Care Access Network-Extension for Community Healthcare Outcomes (SCAN-ECHO) learning model. The VA’s SCAN-ECHO is a similar approach that aims to connect underproductive providers to assist access-challenged providers, using the hub-and-spoke model, which refers to a structure whereby a central point (referred to as the “hub”) disseminates information to different connecting points (referred to as the “spokes”).
Topics Covered in This Report
This report provides background information on VA telehealth, including veteran eligibility and enrollment criteria, VA telehealth copayment requirements, and VA providers’ authority to provide telehealth services anywhere. The report also discusses the components of VA telehealth. It also discusses three issues that Congress could choose to consider: (1) access barriers to in-person VA care, (2) lack of access to the internet, and (3) conflicting guidelines for prescribing controlled substances via telehealth across state lines.
Department of Veterans Affairs (VA): A Primer on Telehealth
Jump to Main Text of Report
Contents
- Introduction
- VA Telehealth Overview
- Rural Veterans
- Integration with the Private Sector
- Report Roadmap
- VA Telehealth Programs and Requirements
- Veteran Eligibility, Enrollment, and Access
- Telehealth Copayment Requirements
- VA Provider Eligibility and Training on Telehealth
- VA Telehealth Components
- The Internet and Wireless Data
- Potential Cybersecurity and Privacy Risks
- Telehealth Modalities
- Home Telehealth (HT)
- Store-and-Forward Telehealth (SFT)
- Clinical Video Telehealth (CVT)
- VA Mobile Health (VA Mobile)
- VA App Store
- Required Login Credentials
- Required Operating Platforms
- VA Video Connect (VVC)
- The VA's Partnerships with Philips Healthcare and T-Mobile
- VA Telehealth Services
- The VA's Partnership with Walmart
- VA Teleconsultations
- Issues for Congress
- Access Barriers to In-Person VA Care Continue to Exist
- Some Veterans Lack Access to the Internet
- Conflicting Guidelines for Prescribing Controlled Substances via Telehealth across State Lines
Figures
- Figure 1. Distribution of Services That Transpired via the Home Telehealth (HT) Modality for those Veterans who Received Telehealth Services, FY2009-FY2018
- Figure 2. Distribution of Services That Transpired via the Store-and-Forward Telehealth (SFT) Modality for Those Veterans who Received Telehealth Services, FY2009-FY2018
- Figure 3. Distribution of Services That Transpired via the Clinical Video Telehealth (CVT) Modality for those Veterans who Received Telehealth Services, FY2009-FY2018
- Figure 4. Selected VA Mobile Apps from the VA App Store
Tables
Appendixes
- Appendix A. Abbreviations Used in This Report
- Appendix B. History of VA Telehealth
- Appendix C. VA Provider Authority to Provide Telehealth Services Anywhere
- Appendix D. Total Number of Veteran Patients who Had Received VA Telehealth Services and Total Number of Telehealth Encounters that Transpired, FY2009-FY2018
Summary
The Veterans Health Administration (VHA), of the Department of Veterans Affairs (VA), is leveraging the use of telehealth with the goal of expanding veterans' access to VA care. Telehealth generally refers to the use of information and communication technology to deliver a health care service. It is a mode of health care delivery that extends beyond the "brick-and-mortar" health care facilities of the VHA. VA telehealth services are generally provided on an outpatient basis and supplement in-person care. Such services do not replace VA in-person care. The VA copay requirements for telehealth are the same as for VA in-person care, but in some cases may be lower than the copays for VA in-person outpatient health care services delivered through the VHA. President Trump and Congress have recently enacted measures such as the VA Maintaining Internal Systems and Strengthening Integrated Outside Networks of 2018 (VA MISSION Act; P.L. 115-182) that aim to address the access barriers that veterans may experience when accessing VA telehealth services across states lines. The VA MISSION Act, among other things, removes all geographic and licensing barriers to VA telehealth, thereby allowing veterans to access VA telehealth services in their communities from any location in the United States, U.S. territories, District of Columbia, and Commonwealth of Puerto Rico.
VA Telehealth Modalities
In FY2018, more than 9.3 million veterans were enrolled in VA care. In that same fiscal year, the VA provided 2.29 million telehealth episodes of care to 782,000 veteran patients collectively using the following three VA telehealth modalities: (1) home telehealth, (2) store-and-forward telehealth, and (3) clinical video telehealth. The VA has developed VA mobile applications (apps), which refer to software programs that run on certain operating systems of mobile devices (e.g., smartphones and tablets) and computers that transmit data over the internet that veterans can access as telehealth applications. Veterans can access VA mobile apps on cellular and mobile devices that operate using either a web-based platform, an iOS platform, or an Android operating platform.
VA Telehealth Partnerships and Access
According to the VA, it cannot meet the health care demands of veteran patients in-house and therefore, it has established partnerships with private sector vendors to help address veterans' demand for VA care. For example, the VA's partnership with the wireless service provider T-Mobile would allow a veteran who has T-Mobile as a cellular wireless service provider to access the VA Video Connect app without incurring additional charges or reducing plan data allotments.
VA Teleconsultations
VA providers can use telehealth platforms and applications to consult with one another, which is referred to as a teleconsultation by section 1709A(b) of title 38 of the U.S. Code. The VA has adopted and modified the Project Extension for Community Healthcare Outcomes (Project ECHO) learning model, which the Expanding Capacity for Health Outcomes Act (P.L. 114-270) required the Secretary of the Department of Health and Human Services to examine and report on, to create a Specialty Care Access Network-Extension for Community Healthcare Outcomes (SCAN-ECHO) learning model. The VA's SCAN-ECHO is a similar approach that aims to connect underproductive providers to assist access-challenged providers, using the hub-and-spoke model, which refers to a structure whereby a central point (referred to as the "hub") disseminates information to different connecting points (referred to as the "spokes").
Topics Covered in This Report
This report provides background information on VA telehealth, including veteran eligibility and enrollment criteria, VA telehealth copayment requirements, and VA providers' authority to provide telehealth services anywhere. The report also discusses the components of VA telehealth. It also discusses three issues that Congress could choose to consider: (1) access barriers to in-person VA care, (2) lack of access to the internet, and (3) conflicting guidelines for prescribing controlled substances via telehealth across state lines.
Introduction
In FY2019, an estimated 20 million veterans were living in the United States, of which 9.3 million were enrolled in care through the Department of Veterans Affairs (VA).1 Chapter 17 of Title 38, U.S.C., requires the VA to provide health care services to eligible veterans through the Veterans Health Administration (VHA) of the VA, which is one of the largest integrated health care systems in the United States. The VHA is composed of nearly 1,700 VA medical facilities.2 VA care is not a health insurance program; it is primarily a direct provider of care.
Meeting veterans' demand for care has been challenging for the VA. Some veteran patients who seek health care services from the VHA experience barriers to receiving in-person care; for example, by being unable to schedule VA medical appointments in a timely manner or having to travel long distances to reach health care facilities.3 In conjunction with the Veterans Choice Program (VCP), the recently enacted VA Maintaining Internal Systems and Strengthening Integrated Outside Networks Act of 2018 (VA MISSION Act; P.L. 115-182), and other measures that aim to expand veterans' access to care, the VA has attempted to address barriers to in-person care using telehealth in VA health care facilities.4 According to the VHA, telehealth refers to the
use of health informatics, disease management and [t]elehealth technologies to enhance and extend care and case management to facilitate access to care and improve the health of designated individuals and populations with the specific intent of providing the right care in the right place at the right time.5
VA Telehealth Overview
VA telehealth is a mode of health care delivery that extends outside of the "brick-and-mortar" health care facilities of the VHA. Telehealth, in contrast to in-person care, functions using information and communication technology (ICT) to transpire an episode of care to a veteran patient, without requiring the patient to visit a service provider in person. Although telehealth generally supplements in-person care, it does not replace VA in-person care.
In this context, the use of ICT to deliver telehealth services does not disrupt a veteran patient's daily life activities, such as working and going to school. Veterans do not need to meet their VA provider in-person to receive VA health care services. This type of nondisruptive access to health care services is likely more convenient than the traditional in-person care services used by veteran patients and their civilian counterparts.6
Telehealth encourages veteran patients to be actively involved in their health care decisions, because it requires veterans to perform telehealth-related tasks such as downloading mobile applications (apps) to connect with VA providers and staff. A mobile app refers to a software program that runs on certain operating systems of mobile devices (e.g., smartphones and tablets) and computers that transmit data over the internet.7 (See the "VA Mobile Health (VA Mobile)" section in this report).
Rural Veterans
Legislation and regulations that aim to expand veterans' access to VA telehealth services generally focus on the U.S. population of rural veterans. Many of these veterans experience geographic barriers to accessing in-person VA care, such as having to travel long distances to reach their nearest health care facilities.8 Of the estimated 9.2 million veterans who were enrolled in the VA health care system in FY2019, approximately 33% of them were rural veterans.9 According to the VA, "[the U.S. population of rural veterans] is older (56% are over 65), poorer (52% earn less than $35,000 per year), and sicker (a greater number of co-morbidities) than their urban counterparts."10 In addition to having to travel long distances to reach their nearest health care facilities, rural veterans may experience access barriers to VA telehealth services because they lack access to broadband internet in their communities.11 Similarly, veterans who live in urban areas also experience access barriers to VA care such as having to wait more than 30 days to receive care through the VA.12
Integration with the Private Sector
According to former Under Secretary of the VHA, David J. Shulkin, MD, who later became the VA Secretary, "[t]he fact is that demand for [v]eterans' health care is outpacing VA's ability to supply [the health care services] in-house."13 President Trump and the Congress have acknowledged the challenges the VA has faced in supplying VA care in-house by enacting measures such as the VA MISSION Act.14 The VA has since established new partnerships with private sector vendors, such as Philips Healthcare, T-Mobile USA, Inc. (T-Mobile), and Walmart Inc. (Walmart), under the VA's Advancing Telehealth through Local Access Stations program. The VA established these partnerships with the goal of reducing veterans' access barriers to VA in-person care by expanding their access to VA telehealth services.15
Report Roadmap
To assist Congress as it considers measures on VA telehealth, this report
- provides an overview of VA telehealth programs and requirements including veteran eligibility and enrollment criteria and VA telehealth copayment requirements;
- discusses VA providers' authority to provide telehealth services anywhere;
- discusses the components of VA telehealth;
- provides an overview of VA teleconsultations;
- discusses three issues that Congress could choose to consider: (1) access barriers to in-person VA care, (2) lack of access to the internet, and (3) conflicting guidelines for prescribing controlled substances via telehealth across state lines;
- provides, in Appendix A, a summary table with all abbreviations used in the report;
- provides, in Appendix B, the history of VA telehealth and a high-level overview of at least one legislative provision that was enacted into law and aims to address VA telehealth, beginning with the 109th Congress;
- provides, in Appendix C, a discussion on the VA providers' authority to provide telehealth services anywhere; and
- provides, in Appendix D, the total number of veterans who received VA telehealth services and the total number of telehealth encounters that transpired during each of the fiscal years FY2009-FY2018.
VA Telehealth Programs and Requirements
On July 12, 2016, the VA established the Office of Connected Care (OCC) within the VHA. The goal of OCC is to "deliver [information technology (IT)] health solutions that increase a [v]eteran's access to care and supports a [v]eteran's participation in their health care."16 OCC administers the following four VA telehealth programs:17
- 1. According to the VA, VA Telehealth Services "[improve] convenience to [v]eterans by providing access to care from their homes or local communities when they need it."
- 2. My HealtheVet is the web-based electronic health record (EHR) for veteran patients through which veterans can view, and download electronic protected health information (ePHI);
- 3. VHA Innovation Program is an annual competitive program that allows VA staff and key stakeholders in the private sector to submit innovative ideas on enhancing VA care; and
- 4. VA Mobile Health (VA Mobile) develops mobile apps.18
For its telehealth programs, the VA has requested an appropriation of $1.1 billion for FY2020 and an advanced appropriation of $1.7 billion for FY2021.19
Veteran Eligibility, Enrollment, and Access
Not all veterans are eligible to receive VA care, and not every veteran is automatically entitled to medical care from the VHA.20 Veterans' eligibility for enrollment in the VHA is based on veteran status (i.e., previous military service), service-connected disability, and income.21 Veterans enrolled in the VA health care system can receive a range of health care services, including primary care and specialty care via telehealth, as authorized under the VA's medical benefits package. The VA medical benefits package refers to a suite of health care services that are covered for eligible veterans, generally at no cost under certain circumstances.22 In a given year, however, not all enrolled veterans receive their care from the VA—either because they do not need services or because they have other forms of health coverage, such as Medicare, Medicaid, or private health insurance.23 In FY2018, more than 9.3 million veterans were enrolled in VA care.24
A veteran generally must be enrolled in the VA health care system to access VA telehealth services, which are typically provided on an outpatient basis. A veteran who is not enrolled in VA care can access VA telehealth services under certain circumstances. For example, a veteran who is not enrolled in VA care but who is "tentatively" eligible for VA care could access VA telehealth services on an outpatient basis.25 Of the 9.3 million veterans who were enrolled in VA care in FY2018, the VA provided 2.29 million telehealth episodes of care to 782,000 veteran patients.26 An episode of care generally refers to all of the health care services that a VA provider provides to a veteran patient, to treat the veteran's health condition/disability.27
The Faster Care for Veterans Act of 2016 (P.L. 114-286) required the VA, among other things, to ensure that veterans could schedule their own telehealth appointments.28 A recent U.S. Government Accountability Office (GAO) report found that neither the Veteran Appointment Request System nor the On-line Patient Self-Scheduling System (OPSS) had the capability to allow veterans to schedule their own telehealth appointments.29 According to the VHA, access to VA telehealth services is a joint decision between the veteran and his or her care team of VA providers and clinical staff.30 The care team tells the veteran which clinically appropriate VA care services he or she can access through the VHA. There may be instances when it is clinically appropriate for a veteran to receive in-person care rather than a telehealth service. When the care team decides that it is clinically appropriate for a veteran to receive telehealth services, the veteran would need to opt into accessing VA telehealth services. The veteran patient would then be able to schedule his or her telehealth appointment.
Telehealth Copayment Requirements
A telehealth copayment refers to the out-of-pocket costs that a veteran patient pays for a telehealth encounter.31 A veteran patient generally pays $15 per primary care outpatient visit and $50 per specialty care visit at VA medical facilities.32 According to the VA, copay amounts for telehealth are usually less than for VA in-person care.33
The VHA does not require veterans to pay a copay for health care services to treat a service-connected disability/condition, nor is a copay required if a veteran meets at least one of the following four main criteria:34
- 1. The veteran patient has a service-connected disability/condition that is rated at 50% percent or more.
- 2. The veteran patient is a former prisoner of war.
- 3. The veteran has an annual income that is below the income limit.
- 4. The veteran is a recipient of the Medal of Honor.
Other veteran patients can receive free VA care when they receive care under certain circumstances, such as care for military sexual trauma, care that is part of a VA research project, and care that is provided for compensation and pension examinations.35
Veteran patients who are not exempt from paying VA copays incur the costs of their VA care. The VA determines a veteran patient's copay by evaluating the rendered telehealth encounter against two factors: (1) the location of the veteran patient when the telehealth encounter transpired and (2) the VA's internal business office protocols on copay amounts for VA care.36
The Honoring America's Veterans and Caring for Camp Lejeune Families Act of 2012 (P.L. 112-154), among other things, allows the VA Secretary to waive veteran patients' copay requirements for telehealth.37 In March 2012, the VA Secretary began waiving copays for telehealth services provided to veteran patients in their homes.
VA Provider Eligibility and Training on Telehealth
The Department of Veterans Affairs Codification Act (P.L. 102-83) requires the VA Secretary, among other things, to establish interrelationships and coordinate the delivery of VA health care services with the public and private sectors.38 Therefore, a health care provider who is either seeking a government position within the VA (referred to as a VA-employed provider) or seeking to remain as a private sector provider while working with the VA under a contract (referred to as a VA-contracted provider) is eligible to provide VA care to veterans. A VA provider, either VA-employed or VA-contracted, must hold at least one full, active, current, and unrestricted state39 license to be eligible to work for or with the VA.40 The provider can use his or her license to deliver in-person care and telehealth services through the VHA. Each VA provider can decide whether he or she wants to provide VA telehealth services to veteran patients across state lines.
The VA MISSION Act, among other things, allows a VA-employed health care provider to provide telehealth services to veteran patients across state lines using only one state license, even in states where the provider is not licensed to practice.41 (Appendix C provides an overview of the VA-employed providers' authority to provide telehealth services across state lines using one state license.) A VA-employed provider who chooses to use a single license in this manner must meet the following four statutory requirements of a covered health care professional:42
- 1. the VA provider must be an employee of the VA;
- 2. the VA Secretary must have authorized the VA provider to provide telehealth services across state lines;
- 3. the VA provider must agree to adhere to all standards for quality relating to the provision of medicine that is consistent with VA policies; and
- 4. the VA provider must hold an active, current, full, and unrestricted license, registration, or certification in at least one state to practice in his or her field of medicine.
This authority does not extend to VA-contracted providers. Current law43 does not allow a VA-contracted provider to provide VA health care services, including telehealth, to veteran patients across states lines using a single license in states where the VA-contracted provider is not licensed to practice. A VA-contracted provider, in contrast to a VA-employed provider, must hold a license in each state where the provider chooses to practice. Neither type of provider is required to obtain a specialty license, registration, or certification to practice his or her field of medicine via telehealth through the VHA.
The VA encourages its providers to complete the Telehealth Master Preceptor Certification Program.44 This program offers an educational curriculum on the delivery of VA telehealth, including the VA telehealth modalities used to deliver telehealth services (see the "Telehealth Modalities" section below). The VHA Telehealth Services National Training Center, which is a nationally accredited training center, oversees the program and other telehealth trainings. In FY2018, according to the VA, more than 56,000 VA providers and staff completed at least one training session on telehealth.45 In that same fiscal year, the VA had provided more than 100,720 telehealth trainings.
VA Telehealth Components
VA telehealth encompasses four general components: (1) the internet and wireless data, (2) telehealth modalities, (3) VA Mobile Health, and (4) VA teleconsultations. Each of these components is discussed below. Health informatics and data visualizations are not discussed because they are beyond the scope of this report.
The Internet and Wireless Data
A veteran patient who chooses to access VA telehealth services must be willing to perform telehealth related tasks, such as accessing a health care service and obtaining his or her ePHI (electronic protected health information), using the internet—the vehicle for which a telehealth episode of care transpires. A veteran patient must have access to the internet to access VA telehealth services on mobile devices and computers. In 2017, according to a VA study of 43,600 veteran enrollees, 77% reported using the internet on an occasional or more frequent basis.46 Of those 77% of veteran enrollees who reported using the internet, the enrollees performed the following telehealth related tasks:47
- 33% scheduled medical appointments,
- 45% accessed their EHRs (electronic health records), and
- 77% searched for information on health.
The VA's findings reveal that veterans who are enrolled in the VA health care system are using the internet to perform telehealth-related tasks. However, veteran patients do not necessarily have to have their own internet service to perform telehealth related tasks and access VA telehealth services. For example, veteran patients can access the internet from a VA medical facility, a family member's home, or a local library (access to high-speed internet service typically yields the best internet performance).48 In addition, a veteran who chooses to access VA telehealth services via a mobile device (e.g., smartphones and tablets) must have adequate cellular data storage. The amount of wireless data storage on a mobile device determines whether the veteran will be able to download and use certain components of VA telehealth such as VA mobile apps.
Potential Cybersecurity and Privacy Risks
A veteran patient who chooses to perform telehealth-related tasks on a personal mobile device and computer must consider the potential cybersecurity and privacy risks associated with accessing VA telehealth services.49 During a telehealth encounter, for example, a veteran patient can view, download, and transmit their ePHI over the internet. According to the Federal Bureau of Investigation, mobile devices and internet connections can be compromised when accessed by an unauthorized party.50 The VHA cannot ensure that a veteran is accessing VA telehealth services on a trustworthy device via a trustworthy connection—that responsibility falls upon the user when the user is accessing the service on their personal device. According to the VA, it "will coordinate restoration activities" with internal and external key stakeholders when veteran patients experience cybersecurity and privacy threats.51
Certain veteran patients can access VA telehealth services on VA issued mobile devices. According to the Federal Communications Commission, the VA provided 6,000 tablets with 4G LTE connectivity to low-income and rural veterans with the goal of reducing the veterans' broadband infrastructure barriers to telehealth in their homes.52 These veterans are accessing telehealth services on trustworthy devices via trustworthy connections. The VA's Cybersecurity Program ensures that, among other things, ePHI and personally identifiable information that are transmitted via VA devices and systems are protected against cybersecurity and privacy threats.53 Of course, cybersecurity and privacy risks are not limited to the U.S. veteran patient population.54
Telehealth Modalities
A telehealth modality refers to the mode in which a telehealth episode of care transpires.55 VA providers offer telehealth services to veteran patients via one of the following three telehealth modalities: (1) home telehealth, (2) store-and-forward telehealth, and (3) clinical video telehealth.56 The three VA telehealth modalities are described in more detail below. Note that the VHA does not consider VA Mobile Health as a telehealth modality, even though veterans can use this technology to access telehealth services.57 The VA considers VA Mobile Health as an "essential element of health care" delivery rather than an ICT tool used to deliver telehealth services.58
In FY2019, the VA is to begin measuring the VHA's performance in addressing the health care needs of eligible veterans who receive telehealth services via these three VA telehealth modalities. For example, one new measurement would analyze the ratio of "the number of unique [v]eterans served through telehealth services (numerator) and the number of unique [v]eterans that receive care through [the] VHA (denominator)."59 Using this measurement, the VA anticipates that at least 15% of eligible veteran patients will access VA telehealth services in FY2019.
Home Telehealth (HT)
The home telehealth (HT) modality allows a VA provider who is not located in the same location as a veteran patient to provide the patient with daily case management services for his or her chronic medical conditions, such as chronic heart disease or diabetes.60 The HT modality allows the VA provider to view medical data and information from a medical device, such as a heart monitor that the veteran patient wears. Telehealth episodes of care via the HT modality generally have no location restrictions unless the veteran patient is on bed rest. From FY2012 to FY2018, the VA provided 6.7 million telehealth encounters via the HT modality to 1.0 million veteran patients.61
In FY2018, the VA provided 872,705 telehealth episodes of care to 136,741 veteran patients through the HT modality. According to the VA, the case management service that VA providers most often provide to veteran patients via the HT modality is the management of hypertension (commonly known as high blood pressure). Figure 1 illustrates the distribution of services that transpired via the HT modality, for those veterans who received telehealth services for each of the fiscal years FY2012-FY2018.
|
Figure 1. Distribution of Services That Transpired via the Home Telehealth (HT) Modality for those Veterans who Received Telehealth Services, FY2009-FY2018 |
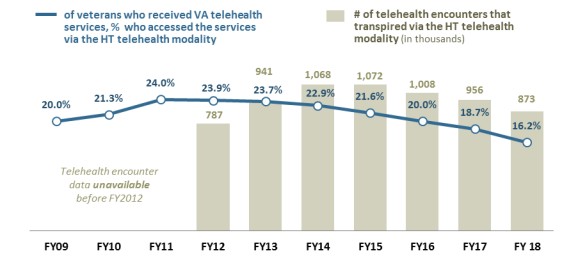 |
|
Source: Figure prepared by CRS based on data from an email that CRS received from the Veterans Health Administration (VHA) of the Department of Veterans Affairs (VA), January 14, 2019. Notes: A single veteran could have received more than one telehealth service via the HT modality. See Appendix D for the total number of veterans who received telehealth services and the total number of telehealth encounters that transpired during each of the fiscal years FY2009-FY2018. According to the VA, the telehealth encounter data on the HT telehealth modality is unavailable for FY2009-FY2011. |
The number of veteran patients who have accessed telehealth services via the HT modality has increased, even though Figure 1 shows a downward trend for the percentage of veteran patients who accessed VA telehealth services via the HT modality. The total population of veteran patients accessing VA telehealth services via the HT modality increased by 142.1%, from 56,484 veteran patients in FY2009 to 136,741 veteran patients in FY2018. However, the number of telehealth encounters that transpired via the HT modality has fluctuated (see Figure 1 and Table D-2).
The VA provided its financial obligations for the delivery of telehealth services via the HT modality in the agency's FY2020 funding and FY2021 advanced appropriations budget request to the Congress.62 In FY2019, the VA estimates that $270.6 million was obligated to the delivery of telehealth services via the HT modality.63 The VA has requested an appropriation of $279.8 million for FY2020 and an advance appropriation of $291 million for FY2021 to deliver telehealth services via the HT modality.
Store-and-Forward Telehealth (SFT)
The store-and-forward telehealth (SFT) modality facilitates the interpretation of patients' clinical information by allowing a VA provider who is not located in the same location as a veteran patient to assist another VA provider who is located in the same location and has provided in-person care to the veteran patient.64 Examples of the clinical information include data, images, sound, and video medical records from the veteran patient's radiology and dermatology examinations. The veteran patient does not have to be present during the electronic transfer of his or her clinical information. After receiving the clinical information, the VA provider interprets the clinical information for the other VA provider and provides follow-up care instructions for the veteran patient. From FY2009 to FY2018, the VA provided 2.7 million telehealth encounters via the SFT modality to 2.5 million veteran patients.65
In FY2018, the VA provided 344,853 telehealth episodes of care to 314,487 veteran patients through the SFT modality. According to the VA, it provides captures, stores, and forwards clinical information mostly for teleretinal imagining via the SFT modality to screen for diabetic eye disease in veteran patients. According to the VA, teleretinal imaging refers to a VA provider's use of a special camera to take a picture of a veteran patient's eye.66 The picture is electronically sent to an eye care specialist. After reviewing the picture, the specialist then reports his or her findings to the veteran patient's primary care provider. Figure 2 illustrates the distribution of services that transpired via the SFT modality, for those veterans who received telehealth services for each of the FY2009-FY2018.
|
Figure 2. Distribution of Services That Transpired via the Store-and-Forward Telehealth (SFT) Modality for Those Veterans who Received Telehealth Services, FY2009-FY2018 |
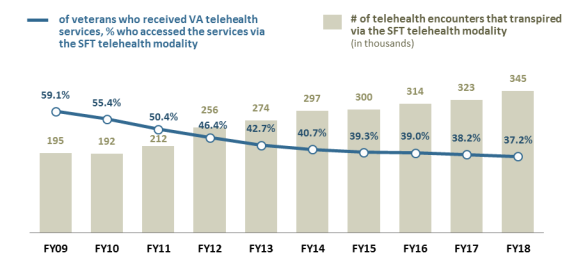 |
|
Source: Figure prepared by CRS based on data from an email that CRS received from the Veterans Health Administration of the Department of Veterans Affairs, January 14, 2019. Notes: A single veteran could have received more than one telehealth service via the SFT modality. See Appendix D for the total number of veterans who received telehealth services and the total number of telehealth encounters that transpired during each of the fiscal years FY2009-FY2018. |
The increase in the number of telehealth encounters that have transpired via the SFT modality seems to indicate that VA providers are increasingly seeking the expertise of their peers. VA providers are presumably seeking additional expertise due to the lack of a given expertise in their respective geographic area and the VA's overall shortage of health care providers.67
Clinical Video Telehealth (CVT)
The clinical video telehealth (CVT) modality allows a VA provider who is not located in the same location as a veteran patient to view, diagnose, monitor, and treat medical conditions of the veteran patient in real-time.68 The CVT modality functions by allowing the VA provider and the veteran patient to see each other via an interactive live video technology. Telehealth episodes of care via the CVT modality transpire between different VA sites of care, such as from a VA medical center (VAMC) to a veteran patient's home or from a veteran patient's home to a VA provider's home office. From FY2009 to FY2018, the VA has provided 5.7 million telehealth encounters via the CVT modality to 2.1 million veteran patients.69
In FY2018, the VA provided 1,074,422 telehealth episodes of care to 393,370 veteran patients through the CVT modality. According to the VA, the telehealth service that veteran patients accessed the most via the CVT modality is telemental health, which refers to the delivery of a mental health service via telehealth.70 Figure 3 illustrates the percentage of veterans who received telehealth services and the number of telehealth encounters that transpired via the CVT modality, for each of the fiscal years FY2009-FY2018.
|
Figure 3. Distribution of Services That Transpired via the Clinical Video Telehealth (CVT) Modality for those Veterans who Received Telehealth Services, FY2009-FY2018 |
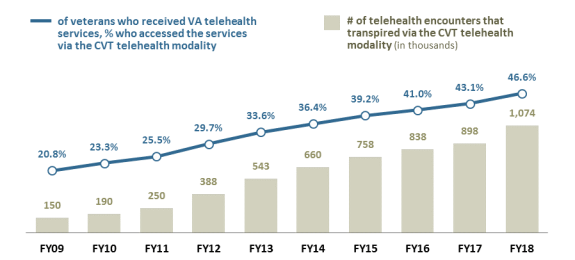 |
|
Source: Figure prepared by CRS based on data from an email that CRS received from the Veterans Health Administration of the Department of Veterans Affairs, January 14, 2019. Notes: A single veteran could have received more than one telehealth service via the CVT modality. See Appendix D for the total number of veterans who received telehealth services and the total number of telehealth encounters that transpired during each of the fiscal years FY2009-FY2018. |
The upward trends in both the percentage of veterans who received telehealth services and the number of telehealth encounters that transpired via the CVT program seem to illustrate that veteran patients are increasingly interested in receiving VA telehealth services via this modality. Veteran patients' interest in the CVT program might stem from it being well established and publicized. The program is the VA's oldest method of telehealth delivery. Additionally, veterans have been able to access telemental health care services via the CVT modality since the VA started providing telehealth services. This report discusses the history of VA telehealth in Appendix B.
VA Mobile Health (VA Mobile)
VA Mobile allows veterans to access certain health services and ePHI via VA mobile apps on mobile devices (e.g. smartphones) and computers.71 According to the National Center for Veterans Analysis and Statistics (NCVAS), 97.9% of veterans who were enrolled in the VHA in 2016 owned a smartphone and 78.3% owned a computer (i.e., a laptop, desktop, or notebook computer).72 Veterans can access the VA mobile apps at any time, regardless of where the veteran is located. According to the VA, "VA Mobile Health aims to improve the health of [v]eterans by providing technologies that expand clinical care beyond the traditional office visit [via mobile apps]."73
VA Mobile has four overall functions: first, it allows veteran patients to connect and schedule medical appointments with VA providers; second, it provides veterans with access to health care information on topics such as mental health and weight management; third, it allows VA providers to provide case management of veteran patients' disabilities/illnesses from afar; and fourth, it allows VA providers to disseminate best practices among themselves, with the goal of improving the health outcomes of veteran patients. As a reminder, the VA does not consider VA Mobile to be one of the three modalities for the delivery of health diagnostics or health services.
 |
|
Source: Figure prepared by CRS using information from the Department of Veterans Affairs (VA), VA App Store, https://mobile.va.gov/appstore/. |
VA App Store
VA mobile apps, such as those illustrated in Figure 4, are located in the virtual VA App Store.74 The VA App Store is a public-facing web-based store that offers 47 mobile apps available to veterans, their caregivers, and VA providers. About two-thirds of the mobile apps in the virtual VA App Store are for veterans and their caregivers. The remainder of the apps are for VA providers. Veterans who are not enrolled in the VHA may access some of the VA mobile apps.
Not all of the mobile apps are specific to health care. VA mobile apps provide veterans with access to a range of VA benefit services and information, such as conferring with a VA pharmacist, reviewing current disability benefits, and obtaining information on depression. Veterans who are not enrolled in the VHA, for example, can also access social apps, such as the VA-Department of Defense (DOD) Veteran Link app, which is a secure social networking app for veterans and current servicemembers.
Required Login Credentials
The public can view the different VA mobile apps in the VA App Store; however, only veterans, their caregivers, and VA providers with certain access accounts can download and use the apps. To download VA mobile apps, a veteran must have login credentials for at least one of the following three accounts: (1) a DOD Self-Service Logon (DS Logon) account, (2) a My HealtheVet account, or (3) an ID.me account.75 A general overview of each of the three accounts, which are all free to veterans, is provided below.76
DOD Self-Service Logon (DS Logon) Account is a federal account that authenticates a veteran's affiliation with the VA and DOD.77 This secure self-service account allows the veteran to access multiple VA and DOD websites and apps. The veteran can request either a Level 1 (Basic) or a Level 2 (Premium) account, both of which are free.
- Level 1(Basic) Account allows a veteran to view general information located on a VA and DOD website.
- Level 2 (Premium) Account allows a veteran to view personal information on VA and DOD websites. The veteran must prove his or her identity to get a Premium Account by answering a set of questions.
MyHealtheVet Premium Account is a federal account that authenticates a veterans' enrollment in VA care.78 It authorizes a veteran patient to complete health care-related tasks, such as viewing his or her electronic health record, reordering medications, and contacting his or her health care provider via a secure messaging technology.
ID.me Account is a private sector account that, in this context, authenticates a veterans' affiliation to the VA and DOD. This account "provides secure identity proofing, authentication, and group affiliation verification for government and businesses across sectors."79 It is also free to veterans.
Required Operating Platforms
The veteran's electronic device must operate using either a web-based platform, an iOS platform, or an Android platform for a VA mobile app to work on the device.80 A web-based platform refers to an operating system that has a web-browser such as Internet Explorer and Google Chrome.81 A VA web-based app such as MyHealtheVet, which is the electronic health record (EHR) for veterans, is accessible over the internet.
An iOS platform refers to the operating system installed on Apple, Inc. (Apple) electronic devices such as the iPhone and iPad.82 A VA iOS-app is available to veterans who use Apple devices. A veteran who has an Apple device can download VA iOS apps from the VA App Store and from the Apple App Store.83 A veteran who does not have an Apple electronic device will not be able to access a VA iOS app on a non-Apple device.
An Android platform refers to the operating system installed on non-Apple electronic devices (e.g., companies such as Samsung and LG).84 A VA Android app is available to veterans with devices that do not have the iOS operating platform installed on them. A veteran who has an electronic device with an Android operating system can download VA Android apps from the VA App Store and the Google Play Store, which is a mobile app on an Android device.85 A veteran who does not have an Android device will not be able to access a VA Android app on a non-Android electronic device.
VA Video Connect (VVC)
The VA Video Connect (VVC) is a mobile app that veteran patients can download from the virtual VA App Store. The VVC app functions by allowing a veteran patient to connect via live video with a VA provider regardless of where the veteran or provider is located, through the CVT modality.86 The veteran patient can use the VVC app on a mobile device. To access the VVC app, the veteran patient's mobile device must contain a web camera, speakers, and microphone.87 In addition, the device must be able to connect to and have access to the Internet. According to the VA, the VVC "uses encryption to ensure privacy in each session."88 The VA launched the VVC app in August 2017 and has recorded 105,300 telehealth visits via the VVC app from October 2017 to September 2018.89
The VA's Partnerships with Philips Healthcare and T-Mobile
The VA has partnered with private sector vendors Philips Healthcare and T-Mobile to expand veterans' access to the VVC app. Philips Healthcare currently partners with the VA by providing veterans with a "virtual connected care" through the company's Virtual Medical Center.90 This new partnership with Philips Healthcare aims to place telehealth information and communication technology equipment in 10 posts at the facilities of two veteran service organizations (VSOs) recognized by the President, Congress, and the VA Secretary for the representation of veterans: Veterans of Foreign Wars and the American Legion.91 The placement of the equipment in the VSO posts would expand VA telehealth services to veterans who are likely to be members of and who frequently visit those two VSOs. However, the program would not exclude non-VSO members from accessing VA telehealth services at the VSO sites. A positive outcome from this pilot program could encourage veterans who are not members of VSOs to visit VSO sites to access VA telehealth services.
The VA's partnership with T-Mobile would allow veterans with this wireless service to access the VVC app via their mobile device without incurring additional charges or reducing plan data allotments.92 According to a VA press release, "veterans will be able to connect to appointments on their mobile devices for no extra charge, regardless of their current data plan."93 The VA did not provide in its press release the amount of the "extra charge" that veteran patients would have incurred from accessing the VVC app on their mobile devices. It is likely that other veterans who do not have T-Mobile as their wireless service provider would incur the unknown extra charge for accessing the VVC app. The VA has not yet announced any plans to partner with all wireless service providers to ensure that veteran patients who access the VVC app on their mobile devices will not incur additional charges.
VA Telehealth Services
The telehealth services that the VA provides to veteran patients align with their respective VA in-patient care services. A VA health care service does not change when a VA provider delivers the service via telehealth. For example, a veteran patient who chooses to access telemental health services via the VVC app on a mobile device would receive the same type of mental health services he or she would have received in-person.
According to the VA Secretary, the VHA is the largest U.S. provider of telehealth services, having provided 2.29 million telehealth episodes of care to 782,000 veteran patients in FY2018.94 Of those 782,000 veteran patients, 9% of them were female and 45% of them live in rural areas.95 Veteran patients can access a range of telehealth services through the VHA. These telehealth services can be grouped into the following seven categories, in alphabetical order:96
- 1. consultative and evaluative telehealth services,
- 2. disease and illness-specific telehealth services,
- 3. gender-specific telehealth services,
- 4. preventative telehealth services,
- 5. rehabilitative telehealth services,
- 6. rural-specific telehealth services, and
- 7. wellness telehealth services.
According to the VA, the agency will provide general VA health care services to veteran patients and refer them to private health care providers for health care services that those providers provide "most effectively and efficiently."97 The VA's decision to refer such services to the private sector might stem from the agency's shortage of VA providers.98
A veteran can access VA telehealth services from various VA sites of care, such as VA medical facilities, mobile telehealth clinics, and non-VA sites of care such as the homes, work places, and schools of veterans. A veteran, who seeks VA care, including VA telehealth services at non-VA medical facilities and nonfederal facilities from non-VA providers, must receive prior authorization from the VA before accessing such services. The VA generally authorizes a veteran to seek VA care from a non-VA provider when
[the existing] VA facilities or other government facilities are not capable of furnishing economical hospital care or medical services because of geographic inaccessibility or are not capable of furnishing care or services required.99
The VA continues to develop new telehealth services to meet the needs of veterans. According to the VA FY2019 funding and FY2020 advanced appropriations budget request to Congress, for example, the Comprehensive Opioid Management in Patient Aligned Care Teams (COMPACT) team is "testing a telehealth-based self-management training system to promote improved care for [v]eterans receiving chronic opioid therapy."100
The VA's Partnership with Walmart
On December 6, 2018, the VA announced a new partnership with Walmart that aims to reduce access barriers to VA care that underserved veterans experience.101 Through this partnership, which is part of the VA's Advancing Telehealth through Local Access Stations program, the VA is establishing a pilot program whereby underserved veterans in certain locations would access VA telehealth services in donated spaces at Walmart retail stores.102 Walmart would provide the VA with operational support. According to Walmart, the prospective locations will be based on "the number of veterans and the health resources offered."103
The VA has stated that its decision to partner with Walmart is based on the fact that more Americans live near a Walmart store than a VA medical center (VAMC). According to the VA,
[90%] of Americans live within ten miles of a Walmart. Ninety percent of veterans [do not] live within ten miles of a [VAMC].104
The VA reported to Congress that there were an estimated 172 VAMCs in 2019.105 For that same calendar year, the VA also reported to Congress that there were other VA medical facilities within the VA health care system, including 23 health care centers, 300 vet centers, and 728 community-based outpatient clinics. The VA has not yet stated how many veterans live near other VA medical facilities in relation to Walmart stores. This information would be helpful to Congress as it considers measures relating to the use of existing VA spaces.106 This prospective pilot program has raised some concerns, however, because according to the Veterans Rural Health Advisory Committee (VRHAC), Walmart is encountering some of the same challenges that the VHA has met when expanding telehealth services to rural veterans, such as keeping pace with technology for virtual care and the expansion of bandwidth.107 However, such challenges could be location-specific and not representative of all Walmart retail store locations.
VA Teleconsultations
Current law (Chapter 17 of Title 38 of the U.S. Code)108 refers to teleconsultation as "the use by a health care specialist of telecommunications to assist another health care provider in rendering a diagnosis or treatment." The law defines teleconsultation in relation to VA's delivery of mental health and traumatic brain injury assessments. The VA extends its use of teleconsultations in the delivery of VA care with the goal of improving veteran patients' health care outcomes, particularly those of rural veterans.
For example, the VA has adopted and modified the Project Extension for Community Healthcare Outcomes (Project ECHO) learning model, which the Expanding Capacity for Health Outcomes Act (P.L. 114-270) required the HHS Secretary to examine and report on, to create a Specialty Care Access Network-Extension for Community Healthcare Outcomes (SCAN-ECHO) learning model.109,110 Project ECHO is a global, technology-enabled collaborative learning model, whereby medical educators and specialty care health care providers disseminate best practices to primary care and rural health care providers, with the goal of improving the health outcomes of rural and underserved patients.111 The best practices are disseminated through different modalities such as teleECHO, which is the delivery of medical education such as patient case-based learning through a virtual network. TeleECHO is delivered through a hub-and-spoke model, which refers to a structure whereby a central point (the "hub") disseminates information to different connecting points (the "spokes").
The VA launched SCAN-ECHO in 2011, with the goal of expanding VA care to rural veterans and veterans that live in medically underserved areas.112 According to the VA, SCAN-ECHO refers to
an approach to provide specialty care consultation, clinical training, and clinical support from specialty care teams to rural primary care providers (PCPs) using video teleconferencing equipment.113
VA teleconsultations generally transpire under SCAN-ECHO using the hub-and-spoke model. The "hubs" are the specialty care providers who are on specialty care teams, and the "spokes" are the PCPs who are on patient aligned care teams (PACTs). According to the VA, SCAN-ECHO transpires when
[PCPs] present a patient's case using multi-site videoteleconferencing equipment. Providers then take information back to the patient for discussion and collaborative decision making. The specialty care team collaborates, culminating in a recommended treatment plan. In addition to case presentations, formal clinical education is provided.114
The Expanding Capacity for Health Outcomes Act (ECHO Act; P.L. 114-270) required the HHS Secretary to examine technology-enabled collaborative learning and capacity-building models and report the findings to Congress no later than two years after enactment.115
In February 2019, the Office of the Assistant Secretary for Planning and Evaluation (ASPE), within HHS, submitted the required report to Congress. ASPE retrieved information about SCAN-ECHO from the VA and found that the VA has evaluated the use of SCAN-ECHO for medical conditions and health care services such as chronic liver disease, diabetes, and women's and transgender health care services.116 For example, ASPE found that the VA studied the difference in health outcomes of 62,750 veterans with chronic liver disease between 2011 and 2015.117 Of those 62,750 veteran patients, 513 of them had received virtual teleconsultations with VA providers who were participating in SCAN-ECHO. According to ASPE, "those receiving the intervention were much less likely to die than those who had no SCAN-ECHO consultation over the same time period."118 SCAN-ECHO is an example of the VA's efforts to expand the capability of VA telehealth to "underproductive providers to assist access-challenged providers."119
Issues for Congress
The VA is leveraging the use of telehealth with the goal of expanding veterans' access to VA care. Based on its experience with telehealth to date, the VA has stated that increased access to telehealth could reduce the use of VA travel benefits by veterans and reduce hospital admissions.120 Telehealth is not a new form of health care delivery. It is a multibillion dollar industry in both the federal and private sectors, showing upward trends in telehealth access, utilization, innovation, and spending.121
Discussed below are three issues that Congress may choose to examine while considering additional topics related to veterans and telehealth services: (1) access barriers to in-person VA care continues to exist, (2) some veterans lack access to the internet, and (3) VA providers' guidelines for prescribing controlled substances via telehealth are different.
Access Barriers to In-Person VA Care Continue to Exist
According to the VA, the agency cannot meet veterans' demand for VA in-patient care.122 Congress and the VA have considered measures and initiatives to expand veterans' access to VA care using telehealth.123 The expansion of VA telehealth does not address the access barriers that veteran patients' face when seeking in-person VA care. Instead, telehealth provides veterans with an alternate way to access health care services through the VHA.
The VA is predicting that the U.S. veteran population will decrease by 32%—from 20.0 million veterans in 2017 to 13.6 million veterans in 2037.124 This prediction does not equate to a lower number of veterans seeking, enrolling in, and accessing VA care in the future. For example, more than three-fourths of the 13.6 million veterans that the VA projects will be in the U.S. veteran population in 2037 might choose to enroll in and access care through the VA health care system. Congress may consider whether the VA should continue to expand veterans' access to VA in-person care in VA brick-and-mortar buildings and/or through VA telehealth services by assessing how such modes of delivery effect the cost and quality of care (in addition to timely access).
Some Veterans Lack Access to the Internet
The overarching goal of the MISSION Act and VA final rule on telemedicine is to expand veteran patients' access to care using telehealth. The use of telehealth services requires that veteran patients have access to the internet to connect to VA telehealth providers. Veteran patients who do not have readily accessible internet connections would likely have difficulty reaching their VA providers. According to the National Center for Veterans Analysis and Statistics (NCVAS), an estimated 20.1% of veterans did not have internet access in 2016.125 In April 2018, for example, the GAO found that some veterans who live on the U.S. Pacific Islands such as Guam and American Samoa, could not access the internet because of damaged cables and equipment failures that occurred during inclement weather.126 The VA is investigating ways to expand veteran patients' access to VA telehealth services to address veterans' lack of access to the internet. Specifically, the agency is evaluating the feasibility of non-VA facilities (e.g., libraries, schools, and post offices) serving as internet/online hotspots, and retaining VA kiosks where veteran patients can access telehealth services.127
Congress and the President have responded to this divide by enacting measures such as the Repack Airwaves Yielding Better Access for Users of Modern Services Act of 2018 (P.L. 115-141; RAY BAUM's Act of 2018). The RAY BAUM's Act of 2018 required, among other things, the Federal Communications Commission (FCC) to submit a report to Congress on promoting broadband internet access to veterans, particularly to rural veterans and veterans with low incomes. The FCC submitted the report to the Senate Committee on Commerce, Science, and Transportation and the House Committee on Energy and Commerce in May 2019.128 According to the FCC's report, the 2.2 million veteran households that do not have access to broadband internet experience barriers when adopting broadband such as the inability to pay for the service and the lack of broadband development in their geographic location.129 In future discussions regarding this issue, Congress may consider the costs associated with deploying broadband infrastructure in underserved geographic areas.130 According to the VA, some veteran patients are given tablets "that operate over 4G LTE mobile broadband to support VA Video Connect," where infrastructure is lacking.131
Conflicting Guidelines for Prescribing Controlled Substances via Telehealth across State Lines
Congress continues to address concerns regarding the prescribing of controlled substances such as opioids.132 The VA MISSION Act and the VA's final rule do not address the prescribing of controlled substances to veteran patients who are not receiving services from within VA medical facilities, or who are not in the same state as the prescribing physician, as permitted under the Ryan Haight Online Pharmacy Consumer Protection Act of 2008 (Ryan Haight Act; P.L. 110-425). Section 311(h)(1) of the Controlled Substance Act (CSA),133 which was added by Section 3 of the Ryan Haight Act, authorized the special registration for telemedicine with the goal of increasing patients' access to practitioners that can prescribe controlled substances via telemedicine in limited circumstances.134 Current law defines a practitioner as
a physician, dentist, veterinarian, scientific investigator, pharmacy, hospital, or other person licensed, registered, or otherwise permitted, by the United States or the jurisdiction in which he practices or does research, to distribute, dispense, conduct research with respect to, administer, or use in teaching or chemical analysis, a controlled substance in the course of professional practice or research.135
The registration would enable a practitioner to deliver, distribute, dispense, or prescribe via telemedicine a controlled substance to a patient who has not been medically examined in person by the prescribing practitioner.136 While the CSA authorized the special registration for telemedicine, practitioners have not been able to apply for this special registration. The Drug Enforcement Administration (DEA) has yet to finalize a rule on the registration's application process and procedures and the limited circumstances that warrant it.137
The Ryan Haight Act expressly exempts VA providers and VA-contracted providers from needing to obtain a special registration in each state where the providers choose to practice, if they meet two conditions. First, the providers must prescribe the controlled substance within the scope of their employment at the VA. Second, the providers must either (1) hold at least one state registration to prescribe a controlled substance or (2) prescribe in a VA health care facility while using the registration of that facility.
The special registration, though not implemented yet by the DEA, the MISSION Act, or the VA's final rule on telehealth, might confuse VA providers about whether they must hold a license in each state where they intend to prescribe controlled substances to veteran patients. The special registration would allow a VA provider to prescribe a controlled substance in a state where the provider is not licensed to practice. The MISSION Act and the VA's final rule on telehealth, in contrast to the special registration, do not preempt state laws regarding the prescribing of controlled substances. VA providers must be licensed in each state where the provider intends to prescribe a controlled substance.138 Congress could consider encouraging the VA to develop guidelines on how its providers would prescribe controlled substances to veteran patients who are not receiving telehealth services from within VA health care facilities.
Appendix A. Abbreviations Used in This Report
|
ASPE |
Office of the Assistant Secretary for Planning and Evaluation, of the Department of Health and Human Services (HHS) |
|
ASPPB |
Association of State and Provincial Psychology Boards |
|
ATLAS |
Advancing Telehealth through Local Access Stations |
|
CCTV |
Closed-circuit television |
|
CMOP |
Consolidated Mail Outpatient Pharmacy |
|
CMS |
Centers for Medicare and Medicaid Services, of HHS |
|
COMPACT |
Comprehensive Opioid Management in Patient Aligned Care Team |
|
CSA |
Controlled Substance Act (P.L. 91-513; as amended) |
|
CVT |
Clinical Video Telehealth Modality |
|
DEA |
Drug Enforcement Agency |
|
DHP |
Digital Health Platform |
|
DOD |
Department of Defense |
|
DOJ |
Department of Justice |
|
DS Logon |
Department of Defense Self-Service Logon |
|
DSL |
Digital Subscriber Lines |
|
DTC |
Direct-to-consumer telehealth |
|
ECHO |
Extension for Community Healthcare Outcomes |
|
EHR |
Electronic health record |
|
ePHI |
Electronic protected health information |
|
FCC |
Federal Communications Commission |
|
FDA |
Food and Drug Administration, of HHS |
|
GPO |
Government Publishing Office |
|
HHS |
Department of Health and Human Services |
|
HRSA |
Health Resources and Services Administration, of HHS |
|
HT |
Home Telehealth Modality |
|
IMLC |
Interstate Medical Licensure Compact |
|
IT |
Information technology |
|
MAT |
Medication assisted therapy |
|
MGH |
Massachusetts General Hospital |
|
NCVAS |
National Center for Veterans Analysis and Statistics |
|
NTIA |
National Telecommunications and Information Administration |
|
OAI |
White House Office of American Innovation |
|
OCC |
Office of Connected Care |
|
ORH |
Office of Rural Health |
|
PACTs |
Patient Aligned Care Teams |
|
PCPs |
Primary Care Providers |
|
Project ECHO |
Project Extension for Community Healthcare Outcomes |
|
PSYPACT |
Psychology Interjurisdictional Compact |
|
PTSD |
Posttraumatic stress disorder |
|
RAY BAUM's Act of 2018 |
Repack Airwaves Yielding Better Access for Users of Modern Services Act of 2018 (P.L. 115-141) |
|
RVAP |
Rural Veterans Health Access Program |
|
SCAN-ECHO |
Specialty Care Access Network-Extension for Community Healthcare Outcomes |
|
SFT |
Store-and-Forward Telehealth Modality |
|
VA |
Department of Veterans Affairs |
|
VAMC |
VA Medical Center |
|
VA MISSION Act |
The VA Maintaining Internal Systems and Strengthening Integrated Outside Networks of 2018 (P.L. 115-182) |
|
VA Mobile |
VA Mobile Health |
|
VVC |
VA Video Connect |
|
VHA |
Veterans Health Administration |
|
VRHAC |
Veterans Rural Health Advisory Committee |
|
VSO |
Veteran Service Organization |
Appendix B. History of VA Telehealth
For decades, the VA has provided telehealth services to veteran patients to improve health care access and to address delivery challenges, such as shortages of in-patient beds and health care providers skilled in the delivery of veteran-centric care. In the 1950s and 1960s, for example, the VA had difficulties in recruiting psychiatrists and neurologists.139 In FY1961, there were 18,722 eligible veterans on a waiting list to receive VA inpatient care for psychiatric and neurological health care conditions.140 That same year, the VA started testing the use of telehealth, with the goal of addressing the aforementioned challenges that veteran patients were experiencing when trying to access VA in-person care for psychiatry and neurology services.
According to the VA's Annual Report for FY1961, the VA tested the use of telehealth by using the closed-circuit television (CCTV) technology as a telehealth modality. The CCTV technology refers to a system that "links a camera to a video monitor using a direct transmission system."141 VA physicians and therapists at a VA medical facility in Oklahoma City, OK, had used the CCTV technology to disseminate best practices and trainings on therapy and psychiatry with the goal of improving veteran patients' health care outcomes.142 According to the VA, its use of telehealth using the CCTV technology was a success because
[t]he results indicate that this form of communication can be a valuable tool in the treatment of psychiatric patients and in the training of personnel in psychiatric service. In addition, it shows the potential in a number of other medical applications, such as, for example, an education technique in surgical training.143
Since then, the VA has aimed to address veterans' access barriers to VA in-person care using updated telehealth technologies and equipment, which are discussed under the "VA Telehealth Components" heading in this report.
Legislative History of VA Telehealth144
The Congress has passed several laws that address VA telehealth. Provided below is a high-level legislative history of VA telehealth, to help inform any future congressional discussion on this issue. For each Congress, beginning with the 109th (January 3, 2005 to January 3, 2007) there is a brief narrative summarizing at least one legislative provision that aims to address VA telehealth. This list may not be comprehensive.
Veterans Benefits, Health Care, and Information Technology Act of 2006 (109th Congress)
The Veterans Benefits, Health Care, and Information Technology Act of 2006 (P.L. 109-461), among other things, required the VA Secretary to increase the number of VA medical facilities that are capable of providing readjustment counseling services via telehealth.145
Veterans' Mental Health and Other Care Improvements Act of 2008 (110th Congress)
The Veterans' Mental Health and Other Care Improvements Act of 2008 (P.L. 110-387), among other things, required the VA Secretary to develop a pilot program to assess the feasibility and advisability of providing certain veterans with peer outreach, peer support, readjustment counseling and other mental health services, using telehealth to the extent practicable.146
Caregivers and Veterans Omnibus Health Services Act of 2010 (111th Congress)
The Caregivers and Veterans Omnibus Health Services Act of 2010 (P.L. 111-163), among other things, allows the VA Secretary to contract with community mental health centers and other qualified health entities with the goal of expanding veterans' access to VA telehealth services.147
Honoring America's Veterans and Caring for Camp Lejeune Families Act of 2012 (112th Congress)
The Honoring America's Veterans and Caring for Camp Lejeune Families Act of 2012 (P.L. 112-154), among other things, allows the VA Secretary to waive veteran patients' copay requirements for telehealth.148
The Veterans Access, Choice, and Accountability Act of 2014 (113th Congress)
The Veterans Access, Choice, and Accountability Act of 2014 (P.L. 113-146), among other things, requires the VA Secretary to improve veterans' access to VA telehealth via mobile vet centers and mobile medical facilities.149
The Faster Care for Veterans Act of 2016 (114th Congress)
The Faster Care for Veterans Act of 2016 (P.L. 114-286), among other things, requires the VA Secretary to ensure that veteran patients can schedule their own medical appointments for VA telehealth services.150
John S. McCain III, Daniel K. Akaka, and Samuel R. Johnson VA Maintaining Internal Systems and Strengthening Integrated Outside Networks Act of 2018 (115th Congress)
The John S. McCain III, Daniel K. Akaka, and Samuel R. Johnson VA Maintaining Internal Systems and Strengthening Integrated Outside Networks Act of 2018 (P.L. 115-182; VA MISSION Act of 2018), among other things, removes all geographic barriers to VA telehealth and therefore allows veterans to access VA telehealth services in their communities from any location in the United States, U.S. territories, District of Columbia, and Commonwealth of Puerto Rico.151
Appendix C. VA Provider Authority to Provide Telehealth Services Anywhere
Veteran patients who cannot access telehealth because of provider shortage gaps may benefit from having access to out-of-state telehealth providers in non-VA health care facilities. Generally, states determine whether a health care provider can provide a health care service across state lines because states handle provider licensure. Each state has the authority to establish its own licensure requirements, and each state licensing board has its own eligibility requirements for health care providers. Due to state-specific licensing laws, a health care provider licensed and certified in one state may not be able to provide health care services to patients located in another state where the provider is not licensed. State licensing laws can cause some health care providers to experience geographical and licensing-related barriers to providing health care services across state lines to rural and underserved populations.
On August 3, 2017, the White House and the VA announced the Anywhere to Anywhere initiative, which aims to remove the geographic barriers that veterans might experience when accessing VA care. Under this initiative, a veteran patient can access VA telehealth services anywhere from a VA provider located outside of a VA health care facility. The initiative is a joint effort between the VHA, the White House Office of American Innovation,152 and the Department of Justice.153 The VA's attempt to expand veterans' access to VA care via telehealth under this initiative was threatened by its providers' experiences of geographic and licensing barriers to delivering the services across state lines.154 On October 30, 2017, a House Committee on Veterans Affairs report found that
the continued expansion of telemedicine across the VA health care system is constrained by restrictions on the ability of VA providers to practice telemedicine across state lines without jeopardizing their state licensure and facing potential penalties for the unauthorized practice of medicine.155
On May 11, 2018, the VA published a final rule in the Federal Register to exempt its providers who deliver care via telehealth from certain state licensing laws and regulations.156 Two major elements of the final rule changed the VHA's existing practice delivery: (1) VA providers may deliver telehealth services outside of VA health care facilities and (2) state licensing boards may no longer deny or revoke a VA provider's license if he or she provides a telehealth service in a state where the provider is not licensed to practice in non-VA health care facilities. According to the VA, the prohibition addresses the concerns of some VA providers that chose not to provide telehealth services across state lines in non-VA health care facilities because their state licensing boards might take action against their licenses for doing so.157 In March 2018, for example, the VA Pacific Island Health Care System reported to the GAO that it had concerns about delivering a telehealth service to a veteran patient in his or her home because a state could require VA providers to be licensed in the state where the patient resides.158 The final rule does not preempt state laws regarding the prescribing of controlled substances, nor does it extend beyond the telehealth provider's employment at the VA or extend to VA-contracted providers.159 A VA-contracted provider must continue to practice under the laws and regulations of his or her state of licensure.
The rule became effective on June 11, 2018, five days after the enactment of the VA MISSION Act. The VA MISSION Act, among other things, removed all geographic barriers to VA telehealth and therefore, allowed veterans to access VA telehealth services in their communities from any location in the United States, U.S. territories, District of Columbia, and Commonwealth of Puerto Rico.160 According to Chapter 17 of Title 38 of the U.S. Code,
(d) Relation to State Law. (1) The provisions of this section shall supersede any provisions of the law of any State to the extent that such provision of State law are inconsistent with this section. (2) No State shall deny or revoke the license, registration, or certification of a covered health care professional who otherwise meets the qualifications of the State for holding the license, registration, or certification on the basis that the covered health care professional has engaged or intends to engage in activity covered by subsection (a).161
The VA MISSION Act codified the core principles of the above-mentioned final rule with the goal of protecting VA providers against possible liability issues stemming from state licensure laws.162 This authority is given only to VA providers that meet the statutory requirement of a "covered health care professional." According to the VA, nearly 10,000 VA providers gained the authority to provide out-of-state telehealth services to veteran patients in non-VA health care facilities in states where the provider is not licensed to practice.163
Appendix D. Total Number of Veteran Patients who Had Received VA Telehealth Services and Total Number of Telehealth Encounters that Transpired, FY2009-FY2018
Table D-1. Total Number of Veteran Patients Who Had Received VA Telehealth Services and Accessed the Services Through Each VA Telehealth Modality, FY2009-FY2018
|
Fiscal Year |
VA Telehealth Modalities |
||
|
Home Telehealth (HT) |
Store-and-Forward Telehealth (SFT) |
Clinical Video Telehealth (CVT) |
|
|
2009 |
56,484 |
166,633 |
58,600 |
|
2010 |
66,175 |
172,505 |
72,600 |
|
2011 |
91,281 |
191,388 |
96,900 |
|
2012 |
119,368 |
232,164 |
148,400 |
|
2013 |
143,043 |
257,904 |
202,800 |
|
2014 |
156,822 |
277,871 |
248,800 |
|
2015 |
155,446 |
282,929 |
282,300 |
|
2016 |
150,237 |
292,130 |
307,000 |
|
2017 |
145,318 |
297,472 |
336,000 |
|
2018 |
136,741 |
314,487 |
393,370 |
|
Totals |
1,220,915 |
2,485,483 |
2,146,770 |
Source: Table prepared by CRS using data from on an email that CRS received from the Veterans Health Administration of the Department of Veterans Affairs, January 14, 2019.
Note: None of the data were rounded by CRS.
Table D-2. Total Number of Telehealth Encounters that Transpired Through Each VA Telehealth Modality, FY2009-FY2018
|
Fiscal Year |
VA Telehealth Modalities |
||
|
Home Telehealth (HT) |
Store-and-Forward Telehealth (SFT) |
Clinical Video Telehealth (CVT) |
|
|
2009 |
Data are unavailable |
194,750 |
149,500 |
|
2010 |
Data are unavailable |
192,445 |
189,700 |
|
2011 |
Data are unavailable |
212,056 |
250,200 |
|
2012 |
786,697 |
256,476 |
387,500 |
|
2013 |
941,440 |
274,430 |
542,600 |
|
2014 |
1,068,313 |
297,135 |
659,600 |
|
2015 |
1,071,569 |
300,133 |
758,000 |
|
2016 |
1,007,709 |
314,048 |
837,900 |
|
2017 |
956,000 |
322,851 |
898,000 |
|
2018 |
872,705 |
344,853 |
1,074,422 |
|
Totals |
6,704,433 |
2,709,177 |
5,747,422 |
Source: Table prepared by CRS using data from on an email that CRS received from the Veterans Health Administration of the Department of Veterans Affairs, January 14, 2019.
Notes: None of the data were rounded by CRS. According to the VA, the telehealth encounter data for the HT modality is unavailable from FY2009-FY2011.
Author Contact Information
Acknowledgments
The U.S. Department of Veterans Affairs provided information and data on VA telehealth for this report.
Amber Wilhelm, CRS Visual Information Specialist, created the data charts and the graphic illustrated in this report.
Carol D. Davis, CRS Senior Research Librarian, performed the legislative search and provided valuable resources on VA telehealth for this report.
Mariam Ghavalyan, CRS Research Assistant, provided invaluable assistance with the data presented in this report.
Footnotes
| 1. |
Department of Veterans Affairs (VA), FY2020 Budget In Brief, 2020 Congressional Submission, pp. BiB-3, 10. |
| 2. |
VA, FY2020 Funding and FY2021 Advance Appropriations, Volume II Medical Programs and Information Technology Programs, p. VHA-277. |
| 3. |
VA, Quality of Care, https://www.va.gov/QUALITYOFCARE/new-approach/improving-access.asp, and Steve Walsh, Patricia Murphy, and Stephan Bisaha, "VA Hospitals Still Struggling with Adding Staff Despite Billions From Choice Act," National Public Radio (NPR), January 31, 2017, Morning. |
| 4. |
CRS Report R44562, The Veterans Choice Program (VCP): Program Implementation, and CRS Report R45390, VA Maintaining Internal Systems and Strengthening Integrated Outside Networks Act of 2018 (VA MISSION Act; P.L.115-182). |
| 5. |
VHA, Patient Care Data Capture, Directive 1082, March 23, 2015, p. 8. This report uses the term "telehealth," as does the VA, even though the Congress uses the term "telemedicine." The term "telehealth" generally refers to the delivery of clinical and nonclinical health care services via a technological method. This term is often used interchangeably with the term "telemedicine," which generally refers to the delivery of only clinical health care services via a technological method. See 38 U.S.C. §1730C and Office of the National Coordinator for Health Information Technology within the Department of Health and Human Services (HHS), What is telehealth? How is telehealth different from telemedicine?, https://www.healthit.gov/faq/what-telehealth-how-telehealth-different-telemedicine. |
| 6. |
Medicare Payment Advisory Commission (MedPAC), Mandated Report: Telehealth Services and the Medicare Program, March 2018, pp. 475, 491-495. |
| 7. |
130 Stat. 1460. The U.S. Food and Drug Administration (FDA) of HHS, classifies some mobile apps as "medical devices" and thus regulates the safety and effectiveness of those mobile apps. See FDA, Medical Devices: Mobile Medical Applications, https://www.fda.gov/medicaldevices/digitalhealth/mobilemedicalapplications/default.htm; and FDA, Examples of Mobile Apps for Which the FDA Will Exercise Enforcement Discretion, https://www.fda.gov/medicaldevices/digitalhealth/mobilemedicalapplications/ucm368744.htm. |
| 8. |
For example, see Representative Gus M. Bilirakis, "Veterans E-Health and Telemedicine Support Act of 2017," remarks in the House, Congressional Record, daily edition, vol. 163, part 81 (November 7, 2017), p. H8557. |
| 9. |
VA, FY2020 Budget In Brief, 2020 Congressional Submission, pp. BiB-10, 16. |
| 10. |
VA, FY2020 Funding and FY2021 Advance Appropriations, Volume II Medical Programs and Information Technology Programs, p. VHA-127. |
| 11. |
Federal Communications Commission (FCC), Wireline Competition Bureau Seeks Comment on Promoting Broadband Internet Access Service for Veterans, Public Notice, September 12, 2018, p. 2. |
| 12. |
For example, see Senator Johnny Isakson, "Veterans Healthcare," remarks in the Senate, Congressional Record, daily edition, vol. 163, part 209 (December 21, 2017), p. S8194; and Representative Jeff Fortenberry, "Year-End Report," remarks in the House, Congressional Record, daily edition, vol. 165, part 4 (January 9, 2019), p. H353. |
| 13. |
VA, "Debunking the VA Privatization Myth," press release, April 5, 2018. |
| 14. |
38 U.S.C. §1730C. |
| 15. |
VA, "National Telehealth Summit to Increase Health Care Access for Veterans," press release, December 6, 2018; and VAntage Point, Telehealth: Adapting Tech to Improve VA Health Care, New Partnerships Set Stage for VA Telehealth Innovation and Expansion, VA, December 20, 2018, https://www.blogs.va.gov/VAntage/55049/va-telehealth/. |
| 16. |
VA, "Telehealth Services and Connected Care," VHA Telehealth Quarterly, January 2016, p. 2, Winter Edition. |
| 17. |
This list was adapted from VA, Connected Care, https://connectedcare.va.gov/terms/connected-health/single/About. |
| 18. |
130 Stat. 1460. The U.S. Food and Drug Administration (FDA) of HHS classifies some mobile apps as "medical devices" and thus regulates the safety and effectiveness of those mobile apps. See FDA, Medical Devices: Mobile Medical Applications, https://www.fda.gov/medicaldevices/digitalhealth/mobilemedicalapplications/default.htm; and FDA, Examples of Mobile Apps for Which the FDA Will Exercise Enforcement Discretion, https://www.fda.gov/medicaldevices/digitalhealth/mobilemedicalapplications/ucm368744.htm. |
| 19. |
VA, FY2020 Funding and FY2021 Advance Appropriations, Volume II Medical Programs and Information Technology Programs, p. VHA-134. |
| 20. |
CRS In Focus IF10555, Introduction to Veterans Health Care. |
| 21. |
38 C.F.R. §17.46. |
| 22. |
38 C.F.R. §17.38. |
| 23. |
CRS in Focus IF 10555, Introduction to Veterans Health Care. |
| 24. |
VA, FY2020 Budget In Brief, 2020 Congressional Submission, p. BiB-10. |
| 25. |
38 C.F.R. §17.42. |
| 26. |
U.S. Congress, House Committee on Appropriations, Subcommittee on Military Construction, Veterans Affairs, and Related Agencies, The State of Veterans Affairs, Statement of the Honorable Robert L. Wilkie, Secretary of Veterans Affairs, 116th Cong., 1st sess., February 26, 2019, pp. 8-9. |
| 27. |
Based on an email that CRS received from the VHA, January 14, 2019. |
| 28. |
130 Stat. 1460. |
| 29. |
U.S. Government Accountability Office (GAO), VA Health Care: Independent Verification and Validation of Patient Self-Scheduling Systems Was Consistent with the Faster Care for Veterans Act of 2016, GAO-18-442R, June 13, 2018, p. 3. |
| 30. |
Based on an email that CRS received from the VHA, January 14, 2019. |
| 31. |
38 U.S.C. §1701. |
| 32. |
38 C.F.R. §17.108(c)(2). |
| 33. |
Based on an email that CRS received from the VHA, January 14, 2019. |
| 34. |
38 C.F.R. §17.108(d). |
| 35. |
Ibid. |
| 36. |
Based on an email that CRS received from the VHA, January 14, 2019. |
| 37. |
38 U.S.C. §1722B. |
| 38. |
38 U.S.C. §523. |
| 39. |
The term "state" means each of the 50 States, territories, and possessions of the United States, the District of Columbia, and the Commonwealth of Puerto Rico. See 38 U.S.C. §101. |
| 40. |
38 U.S.C. §1730C(b)(4). |
| 41. |
38 U.S.C. §1730C. |
| 42. |
This list was adapted from 38 U.S.C. §1730C(b). |
| 43. |
38 U.S.C. §1730C. |
| 44. |
Based on an email that CRS received from the VHA, January 14, 2019; and Office of Enterprise Integration (OEI) within the VA, FY2019/FY2017 Annual Performance Plan and Report, February 2018, p. Appendix-3. |
| 45. |
Based on an email that CRS received from the VHA, January 14, 2019. |
| 46. |
Grace Huang, Ph.D., Benjamin Muz, M.P.P., Sharon Kim, M.P.P., et al., 2017 Survey of Veteran Enrollees' Health and Use of Health Care: Data Findings Report, Westat, April 2018, p. xvll. |
| 47. |
Ibid. |
| 48. |
There are seven types of high-speed internet services: (1) Digital Subscriber Lines, (2) cable modems, (3) fiber optic service, (4) satellite, (5) mobile wireless, (6) fixed wireless, and (7) Wi-Fi hotspots. To learn about each type of high-speed internet service, see Federal Trade Commission, Shopping for High-Speed Internet Service, https://www.consumer.ftc.gov/articles/0022-shopping-high-speed-internet-service. |
| 49. |
CRS In Focus IF10559, Cybersecurity: An Introduction. |
| 50. |
U.S. Federal Bureau of Investigations, What We Investigate: Cyber Crime, https://www.fbi.gov/investigate/cyber. |
| 51. |
VHA, VA Cybersecurity Program, VHA Directive 6500, January 23, 2019, p. 19, https://www.va.gov/vapubs/viewPublication.asp?Pub_ID=1003&FType=2. |
| 52. |
Federal Communications Commission, Report on Promoting Broadband Internet Access Service for Veterans, Pursuant to the Repack Airwaves Yielding Better Access for Users of Modern Services Act of 2018, May 2019, https://docs.fcc.gov/public/attachments/DOC-357270A1.pdf. |
| 53. |
VHA, VA Cybersecurity Program, VHA Directive 6500, January 23, 2019, p. 4, https://www.va.gov/vapubs/viewPublication.asp?Pub_ID=1003&FType=2. |
| 54. |
CRS In Focus IF10473, Digital Health Information and the Threat of Cyberattack. |
| 55. |
Center for Connected Health Policy, What is Telehealth?, http://www.cchpca.org/what-is-telehealth. |
| 56. |
VA, FY2017 Funding and FY2018 Advance Appropriations, Volume II Medical Programs and Information Technology Programs, p. VHA-252. |
| 57. |
U.S. Congress, House Committee on Veterans' Affairs, Subcommittee on Health, Statement of Keven Galpin, M.D. Acting Executive Director for Telehealth, hearing on Technology and Treatment: Telemedicine in the VA Health Care System, 115th Cong., 2nd sess., August 9, 2016, H.Hrg. 3 (Washington, DC: GPO, 2016). |
| 58. |
VA, About VA Mobile Health, https://mobile.va.gov/about#. |
| 59. |
OEI, FY2019/FY2017 Annual Performance Plan and Report, February 2018, pp. Appendix-2, 3. |
| 60. |
U.S. Congress, House Committee on Veterans' Affairs, Subcommittee on Health, Statement of Keven Galpin, M.D. Acting Executive Director for Telehealth, hearing on Technology and Treatment: Telemedicine in the VA Health Care System, 115th Cong., 2nd sess., August 9, 2016, H.Hrg. 4 (Washington, DC: GPO, 2016). |
| 61. |
Based on an email that CRS received from the VHA, January 14, 2019. See Table D-1 in Appendix D. |
| 62. |
The VA does include the obligatory requirements for the other two telehealth modalities, store-and-forward telehealth and clinical video telehealth, in the agency's FY2020 funding and FY2021 advanced appropriations budget request to Congress. |
| 63. |
VA, FY2020 Funding and FY2021 Advance Appropriations, Volume II Medical Programs and Information Technology Programs, p. VHA-134. |
| 64. |
U.S. Congress, House Committee on Veterans' Affairs, Subcommittee on Health, Statement of Keven Galpin, M.D. Acting Executive Director for Telehealth, hearing on Technology and Treatment: Telemedicine in the VA Health Care System, 115th Cong., 2nd sess., August 9, 2016, H.Hrg. 4 (Washington, DC: GPO, 2016). |
| 65. |
Based on an email that CRS received from the VHA, January 14, 2019. See Table D-1. |
| 66. |
U.S. Congress, House Committee on Veterans' Affairs, Subcommittee on Health, Statement of Keven Galpin, M.D. Acting Executive Director for Telehealth, hearing on Technology and Treatment: Telemedicine in the VA Health Care System, 115th Cong., 2nd sess., August 9, 2016, H.Hrg. 7 (Washington, DC: GPO, 2016). |
| 67. |
VA, FY2020 Funding and FY2021 Advance Appropriations, Volume II Medical Programs and Information Technology Programs, pp. VHA-174-175. |
| 68. |
U.S. Congress, House Committee on Veterans' Affairs, Subcommittee on Health, Statement of Keven Galpin, M.D. Acting Executive Director for Telehealth, hearing on Technology and Treatment: Telemedicine in the VA Health Care System, 115th Cong., 2nd sess., August 9, 2016, H.Hrg. 3 (Washington, DC: GPO, 2016). |
| 69. |
Based on an email that CRS received from the VHA, January 14, 2019. See Table D-1. |
| 70. |
VA, Fact Sheet: TeleMental Health in the Department of Veteran Affairs, February 2018, https://www.va.gov/anywheretoanywhere/docs/TeleMental_Health_factsheet.PDF. |
| 71. |
VA, VA Mobile Health FAQs, https://mobile.va.gov/content/va-mobile-health-faqs. |
| 72. |
NCVAS, Profile of Veterans: Internet Use Deep Dive, Data from the 2016 American Community Survey, April 2018, p. 2. |
| 73. |
VA, About VA Mobile Health, https://mobile.va.gov/about. |
| 74. |
To view the virtual VA App Store, see VA, VA App Store, https://mobile.va.gov/appstore/. |
| 75. |
VA, Get Your Secure Logon: Logging into VA Apps, https://mobile.va.gov/login-information#info-dslogon. |
| 76. |
Ibid. |
| 77. |
Department of Defense (DOD), My Access Center: Your DS Logon Self-Service Site, https://myaccess.dmdc.osd.mil/identitymanagement/authenticate.do?execution=e8s1. |
| 78. |
VA, Login to My HealtheVet, https://www.myhealth.va.gov/mhv-portal-web/user-login; and VA, FY2020 Funding and FY2021 Advance Appropriations, Volume II Medical Programs and Information Technology Programs, p. VHA-136. |
| 79. |
ID.me, Inc., About Us, https://www.id.me/about. |
| 80. |
VA, VA App Store, https://mobile.va.gov/appstore/. |
| 81. |
VA, Apps for Web Browsers, https://mobile.va.gov/appstore/web. |
| 82. |
VA, Apps for iOS Devices, https://mobile.va.gov/appstore/iOS. |
| 83. |
Ibid. |
| 84. |
VA, Apps for Android Devices, https://mobile.va.gov/appstore/android. |
| 85. |
Ibid. |
| 86. |
U.S. Congress, House Committee on Veterans' Affairs, Subcommittee on Health, Statement of Keven Galpin, M.D. Acting Executive Director for Telehealth, hearing on Technology and Treatment: Telemedicine in the VA Health Care System, 115th Cong., 2nd sess., August 9, 2016, H.Hrg. 4-3 (Washington, DC: GPO, 2016).; and VA, VA Video Connect, https://mobile.va.gov/app/va-video-connect. |
| 87. |
VA, Frequently Asked Questions: What Type of Equipment Do I Need to Use VA Video Connect?, https://mobile.va.gov/app/va-video-connect#AppFAQ. |
| 88. |
VA, VA Video Connect, https://mobile.va.gov/app/va-video-connect. |
| 89. |
VA, "VA Video Connect Expands Veterans' Access to Health Care," press release, April 30, 2018; and VA, "VA Exceeds 1 Million Video Telehealth Visits in FY2018," press release, February 7, 2019. |
| 90. |
Philips Healthcare, Virtual Medical Center, https://www.usa.philips.com/a-w/government/va-telehealth.html?gclid=EAIaIQobChMIusOR0cWn3wIVEo_ICh1DCQ0BEAAYAyAAEgICpfD_BwE&gclsrc=aw.ds. |
| 91. |
38 U.S.C. §101; 38 U.S.C. §5902; and VAntage Point, Telehealth: Adapting Tech to Improve VA Health Care, New Partnerships Set Stage for VA Telehealth Innovation and Expansion, VA, December 20, 2018, https://www.blogs.va.gov/VAntage/55049/va-telehealth/. |
| 92. |
VAntage Point, Telehealth: Adapting Tech to Improve VA Health Care, December 20, 2018, https://www.blogs.va.gov/VAntage/55049/va-telehealth/. |
| 93. |
Ibid., and VA, VA Video Connect: App Description, https://mobile.va.gov/app/va-video-connect#AppDescription. |
| 94. |
U.S. Congress, House Committee on Appropriations, Subcommittee on Military Construction, Veterans Affairs, and Related Agencies, The State of Veterans Affairs, Statement of the Honorable Robert L. Wilkie, Secretary of Veterans Affairs, 116th Cong., 1st sess., February 26, 2019, pp. 8-9. |
| 95. |
Ibid; and based on an email that CRS received from the VHA, January 14, 2019. |
| 96. |
CRS developed these categories based on the VA's research on telehealth. See VA Health Services Research and Development, Research Topics: eHealth/Telehealth, https://www.hsrd.research.va.gov/research_topics/ehealth.cfm. |
| 97. |
VA, FY2019 Budget In Brief, 2019 Congressional Submission, p. BiB-6. |
| 98. |
VA, FY2020 Funding and FY2021 Advance Appropriations, Volume II Medical Programs and Information Technology Programs, pp. VHA-174-175. |
| 99. |
38 C.F.R. §17.52(a). |
| 100. |
VA, FY2019 Funding and FY2020 Advance Appropriations, Volume II Medical Programs and Information Technology Programs, p. VHA-464. |
| 101. |
VA, "National Telehealth Summit to Increase Health Care Access for Veterans," press release, December 6, 2018; and VAntage Point, Telehealth: Adapting Tech to Improve VA Health Care, New Partnerships Set Stage for VA Telehealth Innovation and Expansion, VA, December 20, 2018. |
| 102. |
Kendra Weaver, Psy.D., VA Telemental Health Innovations: Improving Access to Care, VA, PowerPoint Presentation, May 2018, p. Slide 52. |
| 103. |
Walmart, "U.S. Department of Veteran Affairs and Walmart Announce Telehealth Collaboration to Research Underserved Veterans," press release, December 6, 2018, https://news.walmart.com/2018/12/06/us-department-of-veteran-affairs-and-walmart-announce-telehealth-collaboration-to-reach-underserved-veterans. |
| 104. |
VAntage Point, Telehealth: Adapting Tech to Improve VA Health Care, New Partnerships Set Stage for VA Telehealth Innovation and Expansion, VA, December 20, 2018, https://www.blogs.va.gov/VAntage/55049/va-telehealth/. |
| 105. |
VA, FY2020 Funding and FY2021 Advance Appropriations, Volume II Medical Programs and Information Technology Programs, p. VHA-277. |
| 106. |
The 109th Congress, for example, passed the Veterans Benefits, Health Care, and Information Technology Act of 2006 (P.L. 109-461), which required the VA Secretary, among other things, to expand veterans' access to telehealth services by increasing the number of readjustment counseling service centers (commonly referred to as "Vet Centers") that link to VA medical facilities. See 38 U.S.C. §1712A note. |
| 107. |
Veterans Rural Health Advisory Committee (VRHAC), Presentation: Veteran Integrated Service Network 16 South Central VA Health Care Network, Meeting Notes, May 23, 2018, p. 2. |
| 108. |
38 U.S.C. §1709A(3)(b). |
| 109. |
HHS, Report to Congress: Current State of Technology-Enabled Collaborative Learning and Capacity Building Models, February 2019, https://aspe.hhs.gov/system/files/pdf/260691/ECHOAct-ConsolidatedReportToCongress.pdf. |
| 110. |
VA, VA Uses Technology to Provide Rural Veterans Greater Access to Specialty Care Services, In the Spotlight, https://www.patientcare.va.gov/In_the_Spotlight.asp. |
| 111. |
University of New Mexico, School of Medicine, About [Extension for Community Healthcare Outcomes (ECHO)], https://echo.unm.edu/about-echo-2/. To see where Project ECHOs are located in the United States and globally, see University of New Mexico, School of Medicine, Locations, https://echo.unm.edu/locations-2/. |
| 112. |
VA, VA Uses Technology to Provide Rural Veterans Greater Access to Specialty Care Services, In the Spotlight, https://www.patientcare.va.gov/In_the_Spotlight.asp. |
| 113. |
Office of Rural Health within the VHA, Rural Expansion of Specialty Care Access Networks Extension for Community Health Care Outcomes (SCAN-ECHO), Request for Proposals, November 2012, p. 1. |
| 114. |
VA, VA Uses Technology to Provide Rural Veterans Greater Access to Specialty Care Services, In the Spotlight, https://www.patientcare.va.gov/In_the_Spotlight.asp. |
| 115. |
130 Stat. 1395. |
| 116. |
Office of the Assistant Secretary for Planning and Evaluation (ASPE) within HHS, Current State of Technology-Enabled Collaborative Learning and Capacity Building Models, Report to Congress, February 2019, pp. 79-100. |
| 117. |
Ibid., p. 39. |
| 118. |
Ibid. |
| 119. |
VA, FY2019 Funding and FY2020 Advance Appropriations, Volume II Medical Programs and Information Technology Programs, p. VHA-70. |
| 120. |
VA, VA Telehealth Services: Fact Sheet, https://www.va.gov/COMMUNITYCARE/docs/news/VA_Telehealth_Services.pdf. |
| 121. |
Grand View Research (GVR) Inc., Telemedicine Market Size & Trend Analysis By Product (Hardware, Connectivity & Network), By Region (North America, Europe, Asia Pacific, Latin America, Middle East & Africa), and Segment Forecasts, 2018-2025, Report ID: GVR-1-68038-313-3, April 2017; VAntage Point, Telemedicine: An Important Tool for Veterans Health, September 13, 2017, https://www.blogs.va.gov/VAntage/41153/telemedicine-important-tool-veterans-health/; and MedPAC, Mandated Report: Telehealth Services and the Medicare Program, March 2018, p. 480 (Table 16-1). |
| 122. |
VA, "Debunking the VA Privatization Myth," press release, April 5, 2018. |
| 123. |
Appendix B provides a brief narrative summarizing at least one legislative activity that aims to address VA telehealth, for each of the 109th-115th Congresses. |
| 124. |
National Center for Veterans Analysis and Statistics (NCVAS) of the VA, Veteran Population Projections 2017-2037, https://www.va.gov/vetdata/docs/Demographics/New_Vetpop_Model/Vetpop_Infographic_Final31.pdf. |
| 125. |
NCVAS, Profile of Veterans: Internet Use Deep Dive, Data from the 2016 American Community Survey, April 2018, p. 2. |
| 126. |
GAO, Veterans Health Administration: Opportunities Exist for Improving Veterans' Access to Health Care Services in the Pacific Islands, GAO-18-288, April 12, 2018, p. 45. |
| 127. |
VA, Visualizing Health Care for Rural Veterans with GIS, PowerPoint, July 11, 2017, p. slide 8; and Jared Serbu, "VA Wants to Make Telehealth Part of Its Day-to-Day Business, But Says State Licensing Laws Stand in the Way," Federal News Radio, May 8, 2017, https://federalnewsradio.com/veterans-affairs/2017/05/va-wants-to-make-telehealth-part-of-its-day-to-day-business-but-says-state-licensing-laws-stand-in-the-way/. |
| 128. |
FCC, Report on Promoting Broadband Internet Access Service for Veterans, Pursuant to the Repack Airwaves Yielding Better Access for Users of Modern Services Act of 2018, May 2019, https://docs.fcc.gov/public/attachments/DOC-357270A1.pdf. |
| 129. |
Ibid., pp. 12-13. |
| 130. |
CRS Report RL30719, Broadband Internet Access and the Digital Divide: Federal Assistance Programs. |
| 131. |
VA, FY2020 Funding and FY2021 Advance Appropriations, Volume II Medical Programs and Information Technology Programs, p. VHA-135. |
| 132. |
CRS Report R44987, The Opioid Epidemic and Federal Efforts to Address It: Frequently Asked Questions. |
| 133. |
The primary federal law governing the manufacture, distribution, and use of prescription and illicit opioids is the CSA, a statute that the Drug Enforcement Administration (DEA) is principally responsible for administering and enforcing. See CRS Report R45164, Legal Authorities Under the Controlled Substances Act to Combat the Opioid Crisis. |
| 134. |
CRS Report R45240, The Special Registration for Telemedicine: In Brief, and Letter from Senator Claire McCaskill, Senator Lisa Murkowski, and Senator Dan Sullivan to Robert W. Patterson, Acting Administrator, DEA, January 30, 2018. |
| 135. |
21 U.S.C. §802(21). |
| 136. |
21 U.S.C. §831(h); and 21 U.S.C. §829(e). |
| 137. |
21 U.S.C. §831(h)(2). |
| 138. |
38 U.S.C. §1730C(e); and VA, "Authority of Health Care Providers to Practice Telehealth," 83 Federal Register 21904, May 11, 2018. |
| 139. |
VA, Annual Report for Fiscal Year Ending June 30 1954, March 15, 1955, p. 41; and VA, Annual Report 1961, January 5, 1962, p. 170. |
| 140. |
VA, Annual Report 1961, January 5, 1962, p. 30. |
| 141. |
CCTV technologies are generally used for security surveillance activities. See Department of Homeland Security, CCTV Technology Handbook, July 2013, p. 1. |
| 142. |
VA, Annual Report 1961, January 5, 1962, p. 170. |
| 143. |
VA, Annual Report 1962, January 9, 1963, p. 159. A year after completing the CCTV technology testing, in another example, the VA began testing telehealth using telephone lines as a telehealth modality in 1962. Using the telephone lines, the VA had electronically transmitted veteran patients' electrocardiograms between a VA medical facility in Brooklyn, NY, and a VA medical facility in Baltimore, MD. See VA, Annual Report 1962, January 9, 1963, pp. 159-160. |
| 144. |
Carol D. Davis, a Senior Research Librarian in the Domestic Social Policy Division, performed the legislative search for this report. |
| 145. |
120 Stat. 3411. |
| 146. |
122 Stat. 4116-4117. |
| 147. |
124 Stat. 1150. |
| 148. |
38 U.S.C. §1722B. |
| 149. |
128 Stat. 1778. |
| 150. |
130 Stat. 1460. |
| 151. |
38 U.S.C. §1730C. |
| 152. |
President Donald J. Trump established the White House Office of American Innovation (OAI) in 2017. The OAI provides the President with recommendations on how to improve government operations and polies. See U.S. President (Trump), "Presidential Memorandum on the White House Office of American Innovation," 115th Cong., 1st sess., March 27, 2017. |
| 153. |
The Department of Justice (DOJ) is responsible for enforcing federal laws in the United States. To learn more about DOJ, see CRS Report R44424, FY2017 Appropriations for the Department of Justice, by Nathan James. The White House and the VHA, "Telehealth Technology," press release, August 3, 2017. |
| 154. |
Jared Serbu, "VA Wants to Make Telehealth Part of Its Day-to-Day Business, But Says State Licensing Laws Stand in the Way," Federal News Radio, May 8, 2017. |
| 155. |
U.S. Congress, House Committee on Veterans' Affairs, VA Maintaining Internal Systems and Strengthening Integrated Outside Networks Act of 2018, report to accompany H.R. 5674, 115th Cong., 2nd sess., H.Rept. 115-161 (Washington, DC: GPO, 2018), pp. 13-14. The VA has identified the following seven situations when its providers' practice of telehealth may be inconsistent with state laws: (1) the veteran patient and VA provider are physically located in different states during the telehealth episode of care; (2) the veteran patient is receiving a VA telehealth service from a VA provider in a state where the provider is not licensed to practice; (3) the VA provider is delivering a VA telehealth service to a veteran patient in a state where the provider is not licensed to practice; (4) the VA provider is delivering a telehealth service on a non-VA property; (5) the veteran patient is receiving a telehealth service on a non-VA property; (6) the veteran patient has not been previously assessed, in person, by the VA provider who is delivering the telehealth service; and (7) other state requirements would prevent or impede the practice of health care providers delivering telehealth to veteran patients. See 38 C.F.R. § 17.417(b)(2). |
| 156. |
VA, "Authority of Health Care Providers to Practice Telehealth," 83 Federal Register 21897-21907, May 11, 2018. |
| 157. |
VA, "Authority of Health Care Providers to Practice Telehealth," 82 Federal Register 45757, October 2, 2017. |
| 158. |
GAO, Veterans Health Administration: Opportunities Exist for Improving Veterans' Access to Health Care Services in the Pacific Islands, GAO-18-288, April 12, 2018, p. 46. |
| 159. |
VA, "Authority of Health Care Providers to Practice Telehealth," 83 Federal Register 21904, May 11, 2018. |
| 160. |
38 U.S.C. §1730C. |
| 161. |
38 U.S.C. §1730C(d). |
| 162. |
VA, "Authority of Health Care Providers to Practice Telehealth," 83 Federal Register 21901, May 11, 2018. |
| 163. |
Kevin Galpin, MD, Impact Analysis for RIN 2900-AQ06, VA, May 14, 2018, p. 5. |