Social Security Disability Insurance (SSDI) and Supplemental Security Income (SSI): Eligibility, Benefits, and Financing
The Social Security Administration (SSA) is responsible for administering two federal entitlement programs established under the Social Security Act that provide income support to individuals with severe, long-term disabilities: Social Security Disability Insurance (SSDI) and Supplemental Security Income (SSI). SSDI is a work-related social insurance program authorized under Title II of the act that provides monthly cash benefits to nonelderly disabled workers and their eligible dependents, provided the workers accrued a sufficient number of earnings credits during their careers in jobs subject to Social Security taxes. In contrast, SSI is a need-based public assistance program authorized under Title XVI of the act that provides monthly cash payments to aged, blind, or disabled individuals (including blind or disabled children) who have limited assets and little or no Social Security or other income. In 2017, SSDI and SSI combined paid an estimated $199 billion in federally administered benefits to 14.5 million qualified disabled individuals and 1.5 million non-disabled dependents of disabled workers.
SSDI is part of the federal Old-Age, Survivors, and Disability Insurance (OASDI) program, commonly known as Social Security. OASDI benefits are based on an insured worker’s career-average earnings in jobs covered by Social Security and designed to replace a portion of the income lost to a family due to the worker’s retirement, disability, or death. Workers become insured against these events by acquiring a certain number of earnings credits during their careers in covered employment or self-employment. The SSDI component of the program provides benefits to disabled workers who are under Social Security’s full retirement age and to their eligible spouses and children. The Old-Age and Survivors Insurance (OASI) component also provides disability benefits to eligible disabled dependents of retired workers and to eligible disabled survivors of deceased beneficiaries and deceased insured workers. Although these individuals are not technically disability insurance beneficiaries, they are often included in the term SSDI because they receive Social Security benefits due to a qualifying impairment. SSDI and OASI disability benefits are paid from the Social Security trust funds, which are financed primarily by payroll and self-employment taxes levied on the earnings of covered workers.
SSI is a federal assistance program that provides needy aged, blind, or disabled individuals with a guaranteed minimum income to meet their basic living expenses. Although there are no work or contribution requirements to qualify for payments, the program is based on need and therefore is restricted to individuals with limited financial means. SSI is commonly known as a program of “last resort” because claimants must first apply for most other benefits for which they may be eligible; cash assistance is awarded only to those whose assets and other income (if any) are within prescribed limits. The basic federal SSI payment is the same for all recipients and is reduced by the amount of other income that an individual receives. Some states supplement the federal SSI payment with solely state funds. Unlike Social Security, SSI is financed by appropriations from general revenues.
Most claimants are considered disabled for SSDI and SSI eligibility purposes if they are unable to engage in any substantial gainful activity (SGA) by reason of any medically determinable physical or mental impairment that is expected to last for at least 12 months or to result in death. In 2018, the SGA earnings limit is $1,180 per month for most individuals. Claimants generally qualify if they have an impairment (or combination of impairments) of such severity that they are unable to perform any kind of substantial work that exists in significant numbers in the national economy, taking into consideration their age, education, and work experience. If a claimant’s application for benefits is denied at any point during the disability determination process, the claimant has the right to appeal the determination or decision.
Social Security Disability Insurance (SSDI) and Supplemental Security Income (SSI):
Eligibility, Benefits, and Financing
Jump to Main Text of Report
Contents
- Introduction
- Social Security Disability Insurance (SSDI)
- Eligibility Requirements for Disabled Workers
- Disability-Insured Status
- Under the Full Retirement Age (FRA)
- Eligibility Requirements for Dependents and Survivors
- SSDI Spouses
- SSDI Minor Children
- SSDI Student Children
- SSDI Disabled Adult Children
- OASI Disabled Widow(er)s
- OASI Disabled Adult Children
- Termination Events
- Cash Benefits
- Social Security Benefit Formula
- Maximum Family Benefit Limits
- Workers' Compensation and Public Disability Benefit (WC/PDB) Offset
- Average and Total Monthly Benefit Levels
- When SSDI Benefits Start (The Five-Month Waiting Period)
- Exceptions to the Five-Month Waiting Period for Cash Benefits
- Retroactive Benefits
- Medicare
- 24-Month Waiting Period
- Exceptions to the 24-Month Waiting Period
- Financing
- Supplemental Security Income (SSI)
- Eligibility Requirements
- Categorical Requirements
- Financial Requirements
- Countable Income Limits
- Countable Resource (Asset) Limits
- Deeming of Income and Resources from Certain Close Family Members
- Residency Requirements
- Citizenship Requirements
- Other Requirements
- Termination Events
- Cash Payments
- Federal Benefit Rate (FBR)
- State Supplementary Payments (SSPs)
- Basic Payment Calculation Example
- Gross Income Breakeven Points
- Reduced SSI Payment for Residents of Certain Medical Facilities
- Average and Total Monthly Payment Levels
- When SSI Payments Start
- Medicaid
- 1634 States
- SSI Criteria States
- 209(b) States
- SNAP
- Financing
- Concurrent Disability Beneficiaries
- Definition of Disability
- SSDI and Adult SSI Claimants
- Child SSI Claimants
- Substantial Gainful Activity (SGA) Earnings Limits
- Drug Addiction and Alcohol (DAA)
- Following Prescribed Treatment
- Comparisons with Other Program Definitions of Disability
- Application and Initial Determination Process
- Disability Determinations for SSDI and Adult SSI Claimants
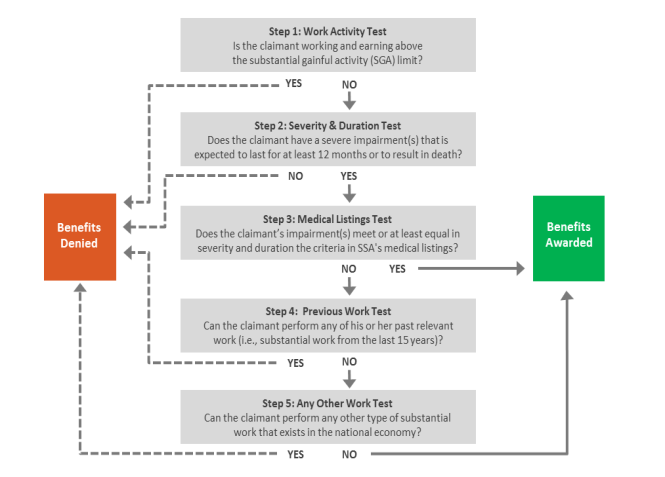
- Step 1. Work Activity Test
- Step 2. Severity and Duration Test
- Step 3. Medical Listings Test
- Step 4. Previous Work Test
- Step 5. Any Work Test
- Disability Determinations for Child SSI Claimants
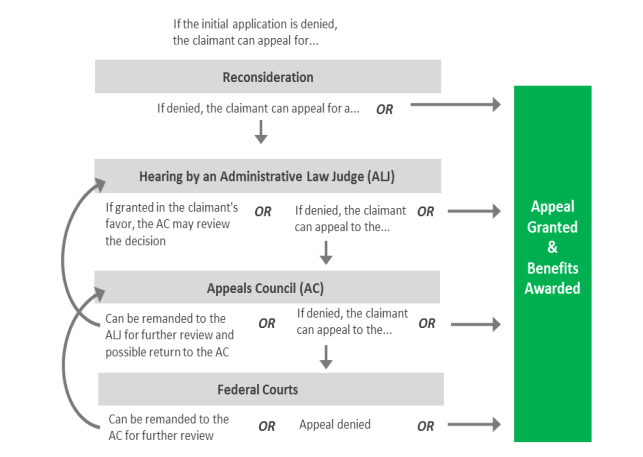
- Appeals Process
- Step 1. Reconsideration
- Step 2. Hearing Before an Administrative Law Judge (ALJ)
- Step 3. Appeals Council (AC)
- Step 4. Federal Courts
- Determinations of Continuing Eligibility
- Continuing Disability Reviews (CDRs)
- Age-18 Disability Redeterminations
- Work CDRs
- SSI Redeterminations
Figures
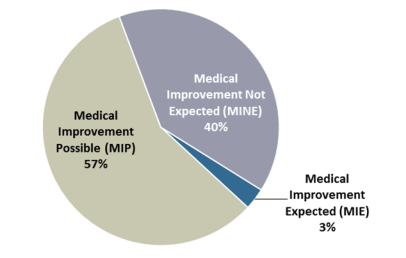
- Figure 1. Social Security Beneficiaries, by Type, December 2017
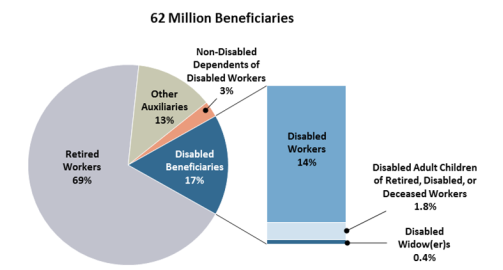
- Figure 2. SSI Recipients, by Eligibility Pathway and Age Group, December 2017
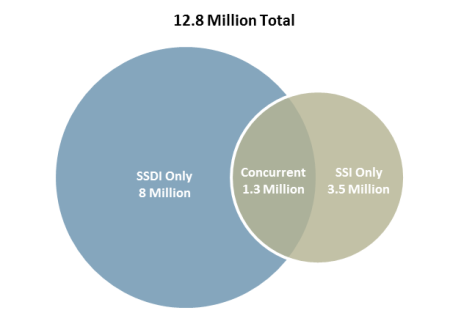
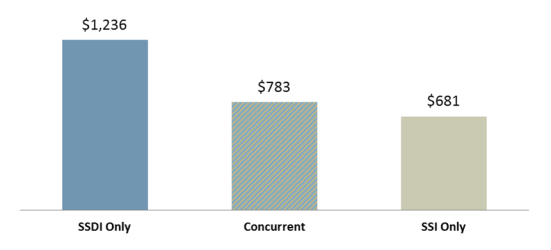
- Figure 3. SSDI Beneficiaries and SSI Disability Recipients Aged 18-64, December 2016
- Figure 4. Average Monthly Benefit Amount for Disability Beneficiaries Aged 18-64, by Type of Disability Beneficiary, December 2016
- Figure 5. Initial Disability Determination Process for SSDI and Adult SSI Claimants
- Figure 6. Initial Disability Determination Process for Child SSI Claimants
- Figure 7. Appeals Process
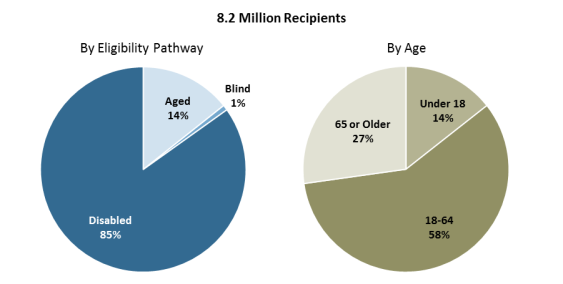
- Figure 8. CDR Diary Classification for SSDI Beneficiaries and SSI Disability Recipients, July 2017
Tables
- Table 1. Number and Share of Disabled Workers Terminated from SSDI and the Annual Termination Rate, by Reason for Termination, 2016
- Table 2. Average and Total Monthly Benefit Amounts of SSDI and OASI Disability Beneficiaries, by Type of Beneficiary, December 2017
- Table 3. Operations of the Social Security Trust Funds, 2017
- Table 4. Number and Share of Nonelderly Blind or Disabled SSI Recipients Terminated and the Annual Termination Rate, by Age Group and Reason for Termination, 2016
- Table 5. Calculating a SSI Payment
- Table 6. Average and Total Monthly Payment Amounts of SSI Recipients, by Type of Payment and Age Group, December 2017
- Table 7. Number of Concurrent Disability Beneficiaries Aged 18-64 and Average Benefit Amount, by Type of SSDI Beneficiary, December 2016
- Table A-1. Comparison of the SSDI and SSI Programs
Summary
The Social Security Administration (SSA) is responsible for administering two federal entitlement programs established under the Social Security Act that provide income support to individuals with severe, long-term disabilities: Social Security Disability Insurance (SSDI) and Supplemental Security Income (SSI). SSDI is a work-related social insurance program authorized under Title II of the act that provides monthly cash benefits to nonelderly disabled workers and their eligible dependents, provided the workers accrued a sufficient number of earnings credits during their careers in jobs subject to Social Security taxes. In contrast, SSI is a need-based public assistance program authorized under Title XVI of the act that provides monthly cash payments to aged, blind, or disabled individuals (including blind or disabled children) who have limited assets and little or no Social Security or other income. In 2017, SSDI and SSI combined paid an estimated $199 billion in federally administered benefits to 14.5 million qualified disabled individuals and 1.5 million non-disabled dependents of disabled workers.
SSDI is part of the federal Old-Age, Survivors, and Disability Insurance (OASDI) program, commonly known as Social Security. OASDI benefits are based on an insured worker's career-average earnings in jobs covered by Social Security and designed to replace a portion of the income lost to a family due to the worker's retirement, disability, or death. Workers become insured against these events by acquiring a certain number of earnings credits during their careers in covered employment or self-employment. The SSDI component of the program provides benefits to disabled workers who are under Social Security's full retirement age and to their eligible spouses and children. The Old-Age and Survivors Insurance (OASI) component also provides disability benefits to eligible disabled dependents of retired workers and to eligible disabled survivors of deceased beneficiaries and deceased insured workers. Although these individuals are not technically disability insurance beneficiaries, they are often included in the term SSDI because they receive Social Security benefits due to a qualifying impairment. SSDI and OASI disability benefits are paid from the Social Security trust funds, which are financed primarily by payroll and self-employment taxes levied on the earnings of covered workers.
SSI is a federal assistance program that provides needy aged, blind, or disabled individuals with a guaranteed minimum income to meet their basic living expenses. Although there are no work or contribution requirements to qualify for payments, the program is based on need and therefore is restricted to individuals with limited financial means. SSI is commonly known as a program of "last resort" because claimants must first apply for most other benefits for which they may be eligible; cash assistance is awarded only to those whose assets and other income (if any) are within prescribed limits. The basic federal SSI payment is the same for all recipients and is reduced by the amount of other income that an individual receives. Some states supplement the federal SSI payment with solely state funds. Unlike Social Security, SSI is financed by appropriations from general revenues.
Most claimants are considered disabled for SSDI and SSI eligibility purposes if they are unable to engage in any substantial gainful activity (SGA) by reason of any medically determinable physical or mental impairment that is expected to last for at least 12 months or to result in death. In 2018, the SGA earnings limit is $1,180 per month for most individuals. Claimants generally qualify if they have an impairment (or combination of impairments) of such severity that they are unable to perform any kind of substantial work that exists in significant numbers in the national economy, taking into consideration their age, education, and work experience. If a claimant's application for benefits is denied at any point during the disability determination process, the claimant has the right to appeal the determination or decision.
Eligibility, Benefits, and Financing
Introduction
The Social Security Administration (SSA) is responsible for administering two federal entitlement programs that provide income support to individuals with severe, long-term disabilities: Social Security Disability Insurance (SSDI) and Supplemental Security Income (SSI).1 SSDI is a work-related social insurance program that provides monthly cash benefits to nonelderly disabled workers and their eligible dependents, provided the workers accrued a sufficient number of earnings credits during their careers in jobs subject to Social Security taxes. In contrast, SSI is a need-based public assistance program that provides monthly cash payments to aged, blind, or disabled individuals (including blind or disabled children) who have limited assets and little or no Social Security or other income. Both programs use the same basic definition of disability to determine eligibility; however, by virtue of design, each program serves a somewhat different population. In 2017, SSDI and SSI combined paid an estimated $199 billion in federally administered benefits to 14.5 million qualified disabled individuals and 1.5 million non-disabled dependents of disabled workers.2
This report discusses the rules and processes used to determine eligibility for SSDI and SSI. It also explains how benefit amounts are computed, the types of non-cash benefits available to individuals who meet SSA's disability standards, and how each program is financed. For a quick overview of SSDI and SSI, see CRS In Focus IF10506, Social Security Disability Insurance (SSDI), and CRS In Focus IF10482, Supplemental Security Income (SSI).
Social Security Disability Insurance (SSDI)
Old-Age, Survivors, and Disability Insurance (OASDI), commonly known as Social Security, is a federal social insurance program established under Title II of the Social Security Act that provides workers and their families with a measure of protection against the loss of income due to the worker's retirement, disability, or death.3 Workers obtain insurance protection by working for a sufficient number of years in jobs where their earnings are subject to Social Security taxes and therefore are creditable for program purposes. Social Security is financed largely on a pay-as-you-go basis, which means that payroll and self-employment tax contributions from current workers, their employers, and self-employed individuals are used to make monthly benefit payments to today's beneficiaries. In 2017, an estimated 173 million people (or about 94% of all workers) worked in paid employment or self-employment covered by Social Security, and the program paid monthly benefits to approximately 62 million beneficiaries (Figure 1).4
The SSDI component of the program, which was enacted in 1956 and implemented in 1957, provides monthly benefits to statutorily disabled workers who are under Social Security's full retirement age (FRA) and to their eligible spouses, divorced spouses, minor children, student children, and disabled adult children. The Old-Age and Survivors Insurance (OASI) component of Social Security also provides benefits to eligible disabled dependents of retired workers and to eligible survivors of deceased beneficiaries and deceased insured workers. Although these individuals are not technically disability insurance beneficiaries, they are often included in the term SSDI, because they receive Social Security benefits due to a qualifying impairment. In December 2017, the SSDI component of Social Security paid benefits to 10.4 million individuals, including 8.7 million disabled workers and 1.7 million of their dependents.5 That same month, the OASI component paid benefits to 1.2 million OASI disability beneficiaries.6
|
Figure 1. Social Security Beneficiaries, by Type, December 2017 |
 |
|
Source: Congressional Research Service (CRS), based on Social Security Administration (SSA), Office of the Chief Actuary (OCACT), "Benefits Paid by Type of Beneficiary," https://www.ssa.gov/oact/ProgData/icp.html. Notes: Subtotals may not sum to totals due to rounding. The term other auxiliaries refers to non-disabled dependents and survivors under the Old-Age and Survivors Insurance (OASI) component of the program. |
Eligibility Requirements for Disabled Workers
To qualify for SSDI, disabled workers must (1) be insured in the event of disability, (2) be under Social Security's FRA, (3) have a qualifying impairment (see the "Definition of Disability" section of this report), and (4) have filed an application for benefits.7
Disability-Insured Status
Workers become insured for Social Security by acquiring a certain number of quarters of coverage (QCs) during their careers in paid employment or self-employment covered by Social Security. A worker's job is considered covered if the services performed in that job or net earnings derived by the individual result in wages or net earnings from self-employment income that are taxable and creditable for insured status and benefit computation purposes. In 2018, workers receive one QC for each $1,320 in covered earnings, up to the maximum of four QCs per year, regardless of when the money is earned.8 Thus, if a worker earns $5,280 in covered wages or net earnings from self-employment income during the first week of January 2018, then he or she would be credited with the maximum number of QCs for the calendar year. The amount of earnings needed for one QC is adjusted annually for average earnings growth in the national economy, as measured by SSA's Average Wage Index (AWI).9 Requiring individuals to have earned a certain number of QCs to qualify for cash benefits ensures that such individuals contribute a minimum amount to the insurance system via payroll and self-employment taxes on each QC's worth of covered earnings.
To be insured in the event of disability, known as disability insured, covered workers must be both fully insured for Social Security and meet a recency-of-work requirement. To be fully insured for SSDI, covered workers must have at least one QC for each calendar year after they turned 21 years old and before the year they became disabled.10 The minimum number of QCs for fully insured status is six for the youngest workers (or 1.5 years of covered work); the minimum number of QCs needed for workers aged 62 or older is 40 (or 10 years of covered work). In effect, individuals must have worked in covered employment or self-employment for about a quarter of their adult lives to be fully insured.
To meet the recency-of-work requirement, disabled workers generally need QCs during the 40-quarter period immediately before the onset of the disability.11 In other words, individuals must have worked in covered employment or self-employment for five of the 10 years before becoming disabled. However, workers under 31 years old may meet the recency-of-work requirement with fewer QCs based on their age.12 In 2017, SSDI provided disability insurance coverage to 154 million workers, with about 89% of covered workers aged 21-64 insured for SSDI.13
Under the Full Retirement Age (FRA)
An insured worker must also be under Social Security's FRA to be entitled to SSDI, which for workers born from 1943 through 1954 is age 66.14 FRA is the age at which unreduced Social Security retired-worker benefits are first payable. Upon attaining FRA, disabled workers are automatically transitioned from disabled-worker benefits (or SSDI) to retired-worker benefits (or OASI); however, this change generally does not affect the amount of Social Security benefits paid to them or their dependents. Under current law, Social Security's FRA increases in two-month increments for workers born from 1955 through 1959 until reaching the age of 67 for workers born in 1960 or later. SSDI is not available to workers who have already attained FRA.
Eligibility Requirements for Dependents and Survivors
In addition to the disabled worker's own benefit, SSDI provides benefits to certain family members of the worker. Social Security pays benefits to family members because workers with one or more dependents are presumed to have greater financial need when they retire, become disabled, or die than similarly situated workers who are single. The OASI component also provides benefits to eligible disabled dependents of retired workers and to eligible survivors of deceased insured workers. The term deceased insured workers includes deceased individuals who received Social Security retired or disabled-worker benefits and non-beneficiary workers who were insured for Social Security at the time of their deaths.
SSDI Spouses
Validly married spouses of disabled workers qualify for benefits if they (1) are aged 62 or older or are any age and have an eligible child in their care who is under the age of 16 or disabled, (2) are not entitled to a retired or disabled-worker benefit equal to or larger than the spousal benefit, and (3) have filed an application for benefits.15 Spouses also must have been married to the worker for at least one continuous year immediately before the day on which the claimant's application is filed.16 This provision is known as a duration-of-marriage requirement.
Divorced spouses of disabled workers may qualify if they (1) are aged 62 or older, (2) are unmarried unless the remarriage occurred after attainment of age 60 or age 50 and the claimant was entitled to disabled widow(er)'s benefits, (3) are not entitled to a retired or disabled-worker benefit equal to or larger than the spousal benefit, and (4) have filed an application for benefits.17 Divorced spouses must have been married to the worker for at least 10 years immediately before the date the divorce became final.18
SSDI Minor Children
Eligible minor children of disabled workers qualify for benefits if they (1) are unmarried, (2) are under the age of 18, and (3) have filed an application for benefits.19 An eligible child is the natural (i.e., biological) child, adopted child, stepchild, equitably adopted child, grandchild, or step-grandchild of the insured worker on whose earnings record the claim is based.20 For certain child claims, such as those involving stepchildren, an explicit dependency requirement must be met, which generally involves the insured worker providing evidence that the child is living with the worker or is receiving at least one-half of his or her support from the worker.21 Otherwise, the child is presumed to be dependent on the insured worker for his or her support. For more information on the rules governing a child's status for purposes of SSDI entitlement, see "GN 00306.001 Determining Status as Child," in SSA's policy manual, the Program Operations Manual System (POMS).22
SSDI Student Children
Eligible student children of disabled workers qualify for benefits if they (1) are unmarried, (2) are aged 18-19, (3) are a full-time student at an elementary or secondary school, and (4) have filed an application for benefits.23 To be considered a full-time student, the child's scheduled attendance must generally be at the rate of at least 20 hours per week (certain exceptions apply).24 Benefits usually continue until the child graduates or until two months after the child attains the age of 19, whichever occurs first. (Social Security benefits for students aged 18-21 enrolled in post-secondary education [i.e., college] were phased out during the 1980s.)
SSDI Disabled Adult Children
Eligible disabled adult children of disabled workers qualify for benefits if they (1) are unmarried, (2) are aged 18 or older, (3) have a qualifying impairment that began before they attained the age of 22, and (4) have filed an application for benefits.25 Disabled adult children (DACs) are also called Childhood Disability Beneficiaries (CDB) by SSA. DAC beneficiaries must meet same the disability standard as disabled workers (discussed later in this report). Although DAC beneficiaries must generally be unmarried to be entitled to benefits, the law provides that they may marry other DAC beneficiaries, along with most other types of Social Security beneficiaries.26 This exception does not apply if the marriage was to a minor or student Social Security beneficiary or to a SSI-only recipient.
OASI Disabled Widow(er)s
Disabled surviving spouses of deceased insured workers qualify for benefits if they (1) are at least 50 years of age but not yet 60 years of age, (2) are unmarried unless the remarriage occurred after attainment of age 50 and the claimant was disabled at the time of the remarriage, (3) are not entitled to a retired-worker benefit equal to or larger than the divorced spousal benefit, (4) have a qualifying impairment that began within seven years of the insured worker's death or within seven years of a previous entitlement to such benefits, and (5) have filed an application for benefits.27
The disabled surviving spouse must also have married to the worker for at least nine months. The duration-of-marriage requirement may be waived, however, if the worker was reasonably expected to live for nine months at the time of the marriage and (1) the worker's death was accidental, (2) the worker's death was in the line of duty while he or she was a member of a military serving on active duty, or (3) the claimant was married to the worker for at least nine months as a result of a previous marriage.28 Disabled divorced surviving spouses may qualify if they were married to the deceased insured worker for at least 10 years immediately before the date the divorce became final.29 As with disabled adult children, disabled widow(er)s must meet same the disability standard as disabled workers.
OASI Disabled Adult Children
Eligible disabled adult children of retired or deceased insured workers qualify for benefits if they (1) are unmarried, (2) are aged 18 or older, (3) have a qualifying impairment that began before they attained the age of 22, and (4) have filed an application for benefits.30 (The same provisions governing SSDI DAC beneficiaries also govern OASI DAC beneficiaries.) Unlike most types of Social Security beneficiaries, there is no maximum age limit for disabled adult children. In December 2016, there were 11,260 DAC beneficiaries aged 80 or older, all of whom were dependents or survivors of retired or deceased insured workers.31
Termination Events
In general, disabled workers continue to receive SSDI benefits until they (1) die, (2) attain FRA, (3) no longer meet the statutory definition of disability (i.e., medically improve), or (4) return to work (i.e., have monthly earnings that exceed certain thresholds discussed later in this report). In 2016, the SSDI termination rate—the ratio of disabled-worker terminations to the average number of disabled-worker beneficiaries during the year—was 9.3% (Table 1). The majority of disabled-worker terminations in 2016 were due to attainment of FRA.
Table 1. Number and Share of Disabled Workers Terminated from SSDI and the Annual Termination Rate, by Reason for Termination, 2016
|
Reason for Termination |
Terminations |
Termination Rate |
|
|
Number |
Share |
||
|
Total |
820,372 |
100.0% |
9.3% |
|
Attainment of Full Retirement Age (FRA) |
470,320 |
57.3 |
5.3 |
|
Death of Beneficiary |
251,492 |
30.7 |
2.8 |
|
Return to Work |
47,887 |
5.8 |
0.5 |
|
Medical Improvement |
37,623 |
4.6 |
0.4 |
|
Other |
13,050 |
1.6 |
0.1 |
Source: Congressional Research Service (CRS), based on the following data sources: Social Security Administration (SSA), Office of Research, Evaluation, and Statistics (ORES), Annual Statistical Report on the Social Security Disability Insurance Program, 2016, October 2017, Table 50, https://www.ssa.gov/policy/docs/statcomps/di_asr/2016/sect03f.html#table50; and SSA, Office of the Chief Actuary (OCACT), "Benefits Paid by Type of Beneficiary," https://www.ssa.gov/oact/ProgData/icp.html.
Notes: The term termination rate is the ratio of the number of terminations to the average number of disabled-worker beneficiaries during the year. In 2016, the average number of disabled-worker beneficiaries was 8,862,068. The term return to work means that the disabled worker's termination was due to monthly earnings above the substantial gainful activity (SGA) threshold, which in 2016 was $1,130 per month for most workers.
With the exception of certain divorced spouses, receipt of SSDI dependents' benefits is linked to the disabled worker's entitlement to Social Security. If a disabled worker's benefits are terminated, benefits payable on his or her earnings record are also generally terminated. Dependents and survivors who no longer meet the relevant entitlement factors are terminated from the rolls as well.32
Cash Benefits
Social Security Benefit Formula
Initial monthly Social Security benefits are based on an insured worker's creditable, career-average earnings in Social Security-covered employment or self-employment. The Social Security benefit formula is progressive, replacing a greater share of career-average earnings for low-wage or intermittent workers than for high-wage workers. In computing the initial benefit amount, a worker's annual taxable earnings are indexed (i.e., adjusted) to reflect changes in national earnings levels over his or her career, up to the second calendar year before the year of eligibility (i.e., the year a worker attains age 62, becomes disabled, or dies).33 Next, years with the highest earnings in the applicable computation period are summed and then divided over the number of months in that period to produce the worker's average indexed monthly earnings (AIME).34 A formula is then applied to the worker's AIME to compute the primary insurance amount (PIA), which is the worker's basic benefit before any adjustments are made. In 2018, the PIA is determined using the following formula:
- 90% of the first $895 of AIME, plus
- 32% of AIME over $985 and through $5,397 (if any), plus
- 15% of AIME over $5,397 (if any).35
The dollar amounts used in this formula are adjusted annually for average earnings growth in the national economy, as measured by the AWI. The worker's PIA is subsequently adjusted to account for inflation through cost-of-living adjustments (COLAs), as measured by the Consumer Price Index for Urban Wage Earners and Clerical Workers (CPI-W).36
Spouses and dependent children of disabled workers each receive up to 50% of the worker's basic benefit amount (i.e., the PIA). These supplementary benefits effectively increase the worker's overall replacement rate—the ratio of benefits received to the worker's previous earnings—to account for additional expenses associated with each dependent. Benefits for dependents are less than the worker's own benefit because a family is assumed to have economics of scale.
Disabled widow(er)s receive up to 71.5% of a deceased worker's PIA. Disabled adult children of retired workers receive up to 50% of the worker's PIA, and disabled adult children of deceased insured workers receive up to 75% of the worker's basic benefit. Initial benefits for survivors are higher than benefits for dependents because a family of a deceased worker experiences a complete loss of that worker's earnings, whereas a family of a retired or disabled worker is compensated partially through the worker's own Social Security benefit.
Maximum Family Benefit Limits
Monthly benefits for retired or disabled workers and their eligible family members and for survivors of deceased insured workers are subject to family maximum provisions, which limit the total amount of benefits that can be paid on a worker's earnings record. Therefore, a dependent's or survivor's payable benefit amount may be less than the maximum share of the worker's PIA for that type of benefit. The family maximum for a disabled worker is the smaller of (1) 85% of the worker's AIME (or 100% of the PIA if larger) or (2) 150% of the PIA.37 If the total amount of all family benefits exceeds the maximum amount, then the benefit of each family member (other than the worker) is reduced proportionately. In December 2016, 27% of all disabled-worker families were receiving maximum family benefits.38 A different family maximum formula applies to OASI disability beneficiaries.39
Workers' Compensation and Public Disability Benefit (WC/PDB) Offset
Disabled workers who also receive workers' compensation (WC) or certain other public disability benefits (PDB) may have their SSDI benefits reduced.40 The Social Security Act contains a provision that reduces the SSDI benefits of disabled workers whose combined disability benefits from SSDI and WC/PDB exceed 80% of their average earnings prior to the onset of disability.41 PDBs do not include disability compensation or pension benefits administered by the Department of Veterans Affairs (VA), disability benefits based on need (e.g., SSI, state or local general assistance [GA]), disability payments made to public employees based on employment covered by Social Security (except for WC), or wholly private pensions or private disability insurance benefits.42 The purpose of this provision is to reduce the attractiveness of SSDI benefits for concurrently eligible individuals who could otherwise remain in the labor force. The WC/PDB offset no longer applies once the disabled worker attains FRA and converts to retired-worker benefits.43 In 17 states and the Commonwealth of Puerto Rico, the direction of the offset is reversed, resulting in a reduction in the WC or PDB payment instead of the SSDI benefit.44 In December 2016, approximately 5.2% of disabled workers were eligible for WC or PDB payments, and about 1.2% of disabled workers were subject to the WC/PDB offset.45
Average and Total Monthly Benefit Levels
In December 2017, the average monthly SSDI benefit was $1,197 for disabled workers, which on an annualized basis was $14,364 (Table 2).46 The average monthly benefit for SSDI dependents ranged from $335 to $499. That month, SSDI paid out over $11 billion in benefits. For OASI disability beneficiaries, the average benefit that month was $800, and total monthly benefits were $992 million.
Table 2. Average and Total Monthly Benefit Amounts of SSDI and OASI Disability Beneficiaries, by Type of Beneficiary, December 2017
|
Type of Beneficiary |
Number of Beneficiaries |
Average Monthly Benefit |
Estimated Total Monthly Benefits (in thousands) |
|
Social Security Disability Insurance (SSDI) |
|||
|
Disabled Workers |
8,695,475 |
$1,197 |
$10,407,353 |
|
Spouses of Disabled Workers |
126,154 |
335 |
42,315 |
|
Minor Children of Disabled Workers |
1,418,446 |
351 |
497,761 |
|
Student Children of Disabled Workers |
47,920 |
499 |
23,898 |
|
Disabled Adult Children of Disabled Workers |
123,257 |
493 |
60,782 |
|
Total |
10,411,252 |
$1,060 |
$11,032,075 |
|
Old-Age and Survivors Insurance (OASI) |
|||
|
Disabled Widow(er)s |
258,286 |
729 |
188,404 |
|
Disabled Adult Children of Retired Workers |
319,162 |
696 |
222,255 |
|
Disabled Adult Children of Deceased Workers |
662,986 |
877 |
581,419 |
|
Total |
1,240,416 |
$800 |
$992,063 |
Source: CRS, based on SSA, OCACT, "Benefits Paid by Type of Beneficiary," https://www.ssa.gov/oact/ProgData/icp.html.
Notes: Average and total monthly benefit amounts are rounded to the nearest whole dollar. Total monthly benefits are derived by multiplying the number of beneficiaries by the unrounded average benefit amount. These estimates are nearly identical to the rounded total monthly benefit data reported in Table 2 of SSA's "Monthly Statistical Snapshot." Estimated data are used because the snapshot does not provide data for the same beneficiary categories used in this report.
When SSDI Benefits Start (The Five-Month Waiting Period)
For disabled workers47 and disabled widow(er)s,48 entitlement to cash benefits begins five full consecutive calendar months after their disability onset date. This requirement is known as the five-month waiting period. The onset date is the first day that a claimant meets the definition of disability under Title II of the Social Security Act in addition to all relevant entitlement factors. If SSA establishes an onset date after the first day of the month, the five-month waiting period starts on the first day of the following month. For example, if a claimant's onset date were April 11, the waiting period would begin on May 1 and would end on September 30. Benefits would first be payable for the month of October, which is the sixth full month after the disability onset date. Because SSA pays Social Security benefits in the month following the month for which they are due, the individual would receive October's payment on one of several possible payment dates in November (i.e., the seventh month after the onset of disability).49
Exceptions to the Five-Month Waiting Period for Cash Benefits
Disabled adult children are not subject to the five-month waiting period; their entitlement to benefits begins the month after their disability onset date, provided they meet all other entitlement factors.50 In addition, former disabled workers do not have to serve a new waiting period if they become disabled again within 60 months (or five years) after their previous entitlement to cash benefits or period of disability ended.51 A similar provision applies to disabled widow(er)s who become disabled again before age 60, and the new period of disability began within 84 months (or seven years) of the month they were last entitled to disabled-widow(er) benefits.52 Furthermore, disabled widow(er)s may count months of eligibility for SSI or federally administered state supplementary payments (discussed later in this report) toward the five-month waiting period.53 Under current law, there are no exceptions to the five-month waiting period for claimants with specific medical conditions, even those considered terminal.
Retroactive Benefits
SSDI provides retroactive benefits for up to 12 months immediately before the month the disabled worker files an application, provided the worker met all other entitlement factors prior to the filing date. Because of the five-month waiting period for cash benefits, the earliest effective date for a SSDI application can be no more than 17 months before the month in which the application is filed.54 The retroactivity provision was established because an early study of the program found that a large share of claimants did not file for benefits in the first month for which they were eligible. Retroactive benefits should not be confused with past-due benefits, which include both retroactive benefits and benefits owed to claimants for months in which they met all relevant entitlement factors in or after the month of application.
Medicare
In addition to cash benefits, Social Security disability beneficiaries (i.e., disabled workers, disabled widow[er]s, and disabled adult children) qualify for health coverage under Medicare.55 Established under Title XVIII of the Social Security Act, Medicare is a federal social insurance program that pays for covered health care services for most individuals aged 65 or older, the majority of Social Security disability beneficiaries and railroad disability annuitants under 65 years old, and certain other individuals who have qualifying impairments.56 (Medicare is not provided to non-disabled dependents under 65 years old.) As with Social Security, workers earn Medicare coverage by working and paying taxes for a sufficient number of years in covered employment or self-employment. For most individuals, entitlement to Medicare is linked to entitlement to Social Security benefits. Social Security disability beneficiaries under 65 years old are provided Medicare because they generally have medical conditions that require significant health care resources. However, many beneficiaries are often unable to work enough to gain health insurance through an employer or to pay for such insurance on their own. In 2013, annual Medicare spending per disabled beneficiary under 65 years old was about $12,776.57
24-Month Waiting Period
Social Security disability beneficiaries under the age of 65 are entitled to Medicare after 24 months of entitlement to cash benefits.58 This requirement is known as the 24-month waiting period. After factoring in the five-month waiting period for cash benefits, disabled workers and disabled widow(er)s typically become entitled to Medicare 29-full calendar months after their disability onset date (i.e., the first day of the 30th full month following disablement). For example, if a claimant's onset date were January 11, 2016, the five-month waiting period for cash benefits would be February 2016 through June 2016, with entitlement to cash benefits beginning July 2016. The claimant would become entitled to Medicare on July 1, 2018, which is the first day of the 25th month of disability benefit entitlement. Disabled adult children are not subject to the five-month waiting period for cash benefits and therefore generally become entitled to Medicare 24 full calendar months after the onset of disability. Due in part to the 24-month waiting period, only 68% of all disabled beneficiaries under 65 years old reported entitlement to Medicare in 2016.59
Exceptions to the 24-Month Waiting Period
General
Social Security disability beneficiaries may count months in which they were previously entitled (or deemed entitled) to cash benefits toward the current Medicare waiting period if their previous entitlement ended within 60 months (or five years) before the month of current onset for disabled workers or 84 months (or seven years) before the month of current onset for disabled widow(er)s and disabled adult children.60 Disability beneficiaries who meet the criteria above and were previously entitled to Medicare do not have to serve a second waiting period for Medicare, because they received cash benefits for at least 24 months during their previous period of disability benefit entitlement and therefore have a sufficient number of months to credit toward the new waiting period. Individuals who become disabled again after the prescribed period may still be able to count months of previous disability benefit entitlement toward the Medicare waiting period if their current impairment is the same, or directly related to, the impairment that served as the basis for disability during a previous period of entitlement.61
In addition, disabled widow(er)s may count months of eligibility for SSI or federally administered state supplementary payments (discussed later in this report) toward the Medicare waiting period.62 It is worth noting that Social Security disability beneficiaries aged 65 or older are entitled to Medicare on the basis of age and thus are not subject to the 24-month waiting period.63
Impairment Related
The Social Security Act specifically excludes disability beneficiaries with amyotrophic lateral sclerosis (ALS; also known as Lou Gehrig's Disease) from having to satisfy the 24-month waiting period requirement.64 Most disability beneficiaries with ALS become entitled to Medicare the first day of the month that entitlement to cash benefits begins, which for disabled workers and disabled widow(er)s is five full calendar months after the onset of disability.
The Social Security Act also contains separate Medicare entitlement provisions for individuals with end-stage renal disease (ESRD)65 or certain medical conditions caused by exposure to qualifying environmental health hazards,66 meaning that individuals who meet the relevant entitlement factors may enroll in Medicare without having to be entitled (or deemed to be entitled) to Social Security benefits. Neither of these entitlement provisions requires eligible individuals to satisfy a 24-month waiting period requirement, although individuals with ESRD may have to satisfy a three-month waiting period requirement if they are on dialysis and do not self-dialyze on a regular basis.67 Social Security disability beneficiaries who meet the requirements specific to these separate entitlement provisions generally receive Medicare coverage in the month they become entitled to cash benefits.
Financing
Social Security's receipts and outlays are accounted for through two legally distinct trust funds: the Federal Disability Insurance (DI) Trust Fund and the Federal Old-Age and Survivors Insurance (OASI) Trust Fund. In the federal accounting structure, a trust fund is an accounting mechanism used by the Department of the Treasury to track and report receipts dedicated for spending on specific purposes, as well as expenditures made to its beneficiaries that are financed by those receipts, in accordance with the terms of a statute that designates the fund as a trust fund. The DI trust fund records receipts and outlays associated with disabled workers and their dependents, and the OASI trust fund records receipts and outlays associated with retired workers and their dependents as well as survivors of deceased insured workers. Administrative costs are also drawn from the trust funds. Each trust fund is a separate account in the U.S. Treasury, and the two funds may not borrow from one another under current law.
Social Security is financed primarily by dedicated payroll and self-employment taxes levied on the earnings of workers in jobs covered by Social Security. Federal Insurance Contributions Act (FICA) taxes are split evenly between employees and employers, while Self-Employment Contributions Act (SECA) taxes are borne fully by self-employed individuals.68 The overall Social Security payroll tax rate is 12.4% of a worker's earnings (6.2% for employees and employers, each), up to a maximum annual amount, which in 2018 is $128,400.69 Of the 12.4%, 2.37% is allocated to the DI trust fund and 10.03% is allocated to the OASI trust fund.70 The two trust funds are also credited with income from the taxation of a portion of some Social Security benefits71 and from interest earned on special-issue U.S. securities held by the trust funds for years when receipts exceeded outlays.72
In 2017, total receipts to the Social Security trust funds were $997 billion, with $171 billion (or 17%) credited to the DI trust fund (Table 3). That same year, total outlays from the trust funds were $952 billion, with $146 billion (or 15%) coming from the DI trust fund. The trust funds held a combined balance of $2.9 trillion in U.S. securities at the end of 2017, with $71 billion (or 2%) credited to the DI trust fund. In 2017, 98% of the DI trust fund's outlays were for benefit payments, with 1.9% for administrative expenses, and 0.1% for certain transfers.
In their 2017 report and under current law, the Social Security trustees project that the trust funds on a hypothetical combined basis will be able to pay benefits in full and on time until 2034.73 However, as noted earlier, the two trust funds are legally distinct entities. Individually, the trustees project that the DI trust fund will be depleted in 2028 and the OASI trust fund will be depleted in 2035. Upon depletion, the trustees project that continuing revenues to the DI trust fund would be sufficient to pay about 93% of benefits scheduled under law, declining to 82% by 2091.
Under its June 2017 baseline and under current law, the Congressional Budget Office (CBO) projected that the trust funds on a hypothetical combined basis would be depleted in calendar year (CY) 2030, with the DI trust fund depleted in FY2023 and the OASI trust fund in CY2031.74 Under its April 2018 baseline, CBO now projects that the DI trust fund will be depleted in early FY2025.75 Upon depletion, CBO projects that continuing revenues to the DI trust fund would be sufficient to pay about 88% of benefits scheduled under law.
|
Category |
Old-Age and Survivors Insurance (OASI) Trust Fund |
Disability Insurance (DI) Trust Fund |
Hypothetical Combined OASDI Trust Funds |
|||
|
Receipts |
||||||
|
Payroll Taxes |
|
|
|
|||
|
Income from Taxation of Benefits |
|
|
|
|||
|
Interest |
|
|
|
|||
|
Other Income |
|
|
|
|||
|
Total Receipts |
|
|
|
|||
|
Outlays |
||||||
|
Benefit Payments |
|
|
|
|||
|
Administrative Expenses |
|
|
|
|||
|
Transfers |
|
|
|
|||
|
Total Outlays |
|
|
|
|||
|
Asset Reserves at End of the Year |
|
|
|
|||
Source: CRS, based on SSA, OCACT, "Financial Data for a Selected Time Period," https://www.ssa.gov/oact/ProgData/allOps.html.
Supplemental Security Income (SSI)
Established under Title XVI of the Social Security Act in 1972 and implemented in 1974, SSI is a means-tested federal assistance program that provides monthly cash payments to the needy individuals and couples who are aged, blind, or disabled.76 The program is intended to provide a guaranteed minimum income to adults who have difficulty covering their basic living expenses due to age or disability and who have little or no Social Security or other income. It is also designed to supplement the support and maintenance of needy children who have severe disabilities. SSI is commonly known as a program of "last resort" because claimants must first apply for most other benefits for which they may be eligible; cash assistance is awarded only to those whose assets and other income (if any) are within prescribed limits. The basic federal SSI payment is the same for all recipients and is reduced by most other income that an individual receives. Some states supplement the federal payment using state funds. In December 2017, SSA issued federally administered payments to 8.2 million SSI recipients, including 1.2 million children under 18 years old, 4.8 million adults aged 18-64, and 2.2 million seniors aged 65 or older.77
As shown in Figure 2, the vast majority of SSI recipients enter the program through the disability pathway. In other words, most individuals become eligible for SSI due to a qualifying impairment other than blindness. Blind or disabled SSI recipients who attain age 65 continue to be classified by SSA as blind or disabled, even though they meet the categorical requirements to be classified as aged. To avoid confusion, this report focuses primarily on blind or disabled SSI recipients under 65 years old.
|
Figure 2. SSI Recipients, by Eligibility Pathway and Age Group, December 2017 |
 |
|
Source: CRS, based on SSA, "SSI Monthly Statistics, 2017," January 2018, Table 2, https://www.ssa.gov/policy/docs/statcomps/ssi_monthly/2017/index.html. Notes: The share of blind SSI recipients is estimated based on 2016 administrative data. See SSA, Office of Research, Evaluation, and Statistics (ORES), SSI Annual Statistical Report, 2016, Table 5, https://www.ssa.gov/policy/docs/statcomps/ssi_asr/. |
Eligibility Requirements
To qualify for SSI, a person must (1) be aged, blind, or disabled as defined in the Social Security Act, (2) have limited income and resources, (3) meet certain other requirements, and (4) have filed an application for payments.78
Categorical Requirements
Public assistance programs usually limit eligibility to certain groups or categories of people who often have difficulty providing for themselves. Under the SSI program, an individual or couple must be aged, blind, or disabled to qualify for payments.79 Aged refers to individuals who are aged 65 or older.80 Blind refers to individuals of any age who have central visual acuity of 20/200 or less in the better eye with the use of a correcting lens or a limitation in the fields of vision so that the widest diameter of the visual field subtends an angle of 20 degrees or less (i.e., tunnel vision).81 Individuals are considered disabled if they meet SSI's age-specific definition of disability (see the "Definition of Disability" section of this report).
Financial Requirements
In addition to meeting one of the aforementioned categories, an individual or couple must have limited income and other financial resources. Income is defined as anything one receives in cash or in kind that can be used to meet one's needs for food and shelter.82 Resources are cash or other liquid assets or any real or personal property that an individual (or spouse, if any) owns and could convert to cash to be used for his or her support and maintenance.83 Under SSI, a person's countable income and resources must be within the program's statutory limits. Because certain income and resources are disregarded (i.e., not counted), a person may have gross income or resources above the countable limits and still be eligible for the program. In addition to the person's own income and resources, the income and resources of certain ineligible family members (such as a spouse or parent) may be deemed available to meet the needs of the person, and as such, may be included in his or her countable income and resources.
Countable Income Limits
The limit for countable income—gross income minus all applicable exclusions—is equal to the federal benefit rate (FBR), which is the maximum monthly SSI payment available to qualified individuals and couples who have no other income.84 In 2018, the FBR is $750 per month for an individual living in his or her own household and $1,125 per month for a couple living in their own household if both members are SSI eligible.85 The FBR is adjusted annually for inflation by the same COLA applied to Social Security benefits.86 Countable income is subtracted from the FBR in determining eligibility for SSI and the amount of the cash payment. In general, individuals and couples are eligible for SSI if their countable income is less than or equal to the FBR.87 In states that have an agreement with SSA for the agency to administer their state supplementation program (primarily California, Nevada, New Jersey, and Vermont), a person is considered eligible for SSI if his or her countable income is less than the FBR plus the amount of the applicable federally administered state supplementary payment.
Income That is Counted
Under the SSI program, all income is counted unless excluded under federal law or, if provided in statute, at the discretion of the Commissioner of Social Security through agency regulations or subregulatory guidance. SSI classifies income as either earned or unearned. Earned income includes wages, net earnings from self-employment, payments for services performed in a sheltered workshop (now known as a Community Rehabilitation Program [CRP]), and certain royalties and honoraria.88 Unearned income refers to all income that is not earned income (i.e., income not derived from current work), such as Social Security, benefits administered by the VA, unemployment insurance (UI),89 benefits administered by the Railroad Retirement Board (RRB),90 the individual's share of the Temporary Assistance for Needy Families (TANF) grant,91 workers' compensation, public or private pensions, interest income, cash from family or friends, and in-kind support and maintenance (i.e., the value of non-cash benefits such as food or shelter).92
Income That is Not Counted
Certain income is disregarded in determining eligibility for and the amount of assistance provided by SSI.93 For example, the program excludes the following:
- the first $20 per month of any income (earned or unearned), other than unearned income based on need that is totally or partially funded by the federal government or by a non-governmental agency (e.g., TANF);94
- the first $65 per month of earned income plus one-half of any earnings above $65;95
- the first $30 per calendar quarter of infrequent or irregular earned income;96
- the first $60 per calendar quarter of infrequent or irregular unearned income;97
- food assistance provided under the Supplemental Nutrition Assistance Program (SNAP) and the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) program;98
- energy assistance provided under the Low Income Home Energy Assistance Program (LIHEAP);99
- housing assistance provided by most federally funded housing programs;100
- federal tax refunds and advanced tax credits, including the Earned Income Tax Credit (EITC) and the child tax credit (CTC);101
- assistance based on need that is funded wholly by a state or local entity;102
- the first $2,000 received during a calendar year as compensation for participation in a clinical trial involving research and testing of treatments for a rare disease or condition;103
- impairment-related work expenses (IRWEs) for disabled recipients and blind work expenses (BWEs) for blind recipients;104 and
- any income used to fulfill a plan to achieving self-support (PASS).105
For a more detailed list of unearned income exclusions, see "SI 00830.099 Guide to Unearned Income Exclusions" in POMS.106
The $20 per month general income exclusion and the $65 per month earned income exclusion are not indexed to inflation and have remained at their current levels since the SSI program was enacted in 1972.
Treatment of In-Kind Support and Maintenance (ISM)
SSA defines in-kind support and maintenance (ISM) as food or shelter that a person receives from someone else who pays for it.107 Shelter includes room, rent, mortgage payments, real property taxes, heating fuel, gas, electricity, water, sewerage, and garbage collection services.108 ISM is treated as unearned income subject to special rules based on a person's living arrangement. If a person lives throughout a month in another's household and receives both food and shelter from others living in the household, the FBR is reduced by one third. This reduction is known as the value of the one-third reduction (VTR) and is not rebuttable.109 In 2018, the VTR is $250 per month for an individual ($750 x 1/3) and $375 per month for a couple ($1,125 x 1/3).110 The $20 per month general income exclusion does not apply to ISM reduced under the VTR.
However, if a person receives ISM but does not receive both food and shelter from the household in which the individual lives (either his or her own household or the household of another), then the FBR is reduced by the presumed maximum value (PMV) rule.111 The PMV is a regulatory cap on ISM designed to address situations in which an individual receives ISM but is not subject to the statutory VTR. The reduction under the PMV is equal to one-third of the FBR plus $20, which in 2018 is $270 per month for an individual ($750 x 1/3 + $20) and $395 per month for a couple ($1,125 x 1/3 + $20). Unlike the VTR, the PMV is rebuttable. If the SSI recipient can show that the value of food or shelter received is less than the PMV reduction, then SSA reduces the FBR by the actual value of food or shelter received. Some ISM is disregarded, such as federal housing assistance.112 According to SSA, only about 9% of SSI recipients have ISM reductions.113
Countable Resource (Asset) Limits
The limit for countable resources—gross resources minus all applicable exclusions—is $2,000 for an individual and $3,000 for a couple.114 Individuals and couples are eligible for SSI if their countable resources are less than or equal to the applicable statutory limit at any given time.115 Claimants and recipients who transfer (i.e., sell or give away) resources at less than fair market value (FMV) may become ineligible SSI for up to 36 months.116 The look-back period for determining if a transfer was made at less than FMV is also 36 months. Unlike the FBR, the countable resource limits are not adjusted for inflation and have remained at their current levels since 1989.
Resources That Are Counted
As with income, all resources are counted under the SSI program unless excluded federal law or, if provided in statute, at the discretion of the Commissioner of Social Security through agency regulations or subregulatory guidance. The person must have the right, authority, or power to liquidate the property (or his or her share of the property) for the asset to be considered a resource. Countable resources include the following:
- cash retained as of the first moment of the month following the month of receipt;
- bank savings or checking accounts;
- stocks, bonds, mutual funds, and certificates of deposit;
- tractors, boats, machinery, livestock, buildings, and land;
- individual retirement accounts (IRAs) and 401(k) plans under certain conditions;
- unrestricted health savings accounts (HSAs); and
- most types of trusts established with the assets of an individual on or after January 1, 2000.117
Resources That Are Not Counted
Certain resources are excluded in determining SSI eligibility.118 For example, the program excludes the following:
- the person's primary residence;119
- household goods and personal effects;120
- one automobile used for transportation;121
- property essential to self-support (PESS);122
- health flexible spending arrangements (FSAs);123
- resources needed to fulfill a PASS;124
- federal tax refunds and advanced tax credits for a 12-month period;125
- all life insurance policies on a person up to a combined face value of $1,500;126
- up to $1,500 in burial funds set aside for burial expenses of the individual or the individual's spouse;127
- special needs trusts (SNTs) or pooled trusts (PTs) that meet the requirements of Medicaid law;128 and
- the first $100,000 in an Achieving a Better Life Experience (ABLE) account.129
For a more detailed list of resource exclusions, see "SI 01130.050 Guide to Resources Exclusions" in POMS.130
Deeming of Income and Resources from Certain Close Family Members
As a program of "last resort," SSI expects close family members to provide support to low-income aged, blind, and disabled individuals in determining their level of need. Specifically, the income and resources of certain ineligible family members are deemed to be available to meet the basic needs of eligible individuals, and as such, may be included in the individual's countable income or resources for purposes of determining SSI eligibility and the amount of assistance. This process, known as deeming, is used instead of determining the amount of ISM provided by a deemor (i.e., the ineligible family member whose income and resources are subject to deeming) under the VTR or PMV rule. The Social Security Act specifies that deeming applies to the following types of relationships.
- Spouse-to-Spouse. An eligible individual resides in the same household with his or her ineligible spouse.
- Parent-to-Child. An eligible child under 18 years old resides in the same household with his or her ineligible natural (i.e., biological) or adoptive parent(s) or with his or her ineligible natural parent and the spouse of a parent (i.e., a stepparent).
- Sponsor-to-Alien. An eligible alien has a sponsor (usually a relative) who assumes financial responsibility for him of her for purposes of the alien being lawfully admitted to the United States.131
In determining the amount of the deemor's income and resources available to the eligible individual, SSA first applies the basic income and resource exclusions mentioned previously. Next, the agency deducts from the income of the ineligible family member an allocation for his or her living expenses, as well as an allocation for each ineligible child under 18 years old (or under 22 years old and a student) living in the household. This allocation does not apply, however, if the ineligible family member receives public income-maintenance payments, such as TANF or VA pensions based on need.132 In 2018, the allocation is $375 for an ineligible spouse, $375 for each ineligible child, $750 for one ineligible parent, and $1,125 for two ineligible parents. (Different income allocation rules apply to sponsors of aliens.) Finally, SSA charges the remaining countable income of the deemor (if any) to the eligible individual's unearned income and then applies the normal income counting rules to determine SSI eligibility and the amount of the payment. Under deeming, the countable resource limits are $3,000 for an eligible individual with an ineligible spouse, $4,000 for an eligible child with one ineligible parent, $5,000 for an eligible child with two ineligible parents, $2,000 for an alien with an unmarried sponsor, and $3,000 for an alien with a married sponsor.133 For more information on deeming, see Virginia Commonwealth University's National Training and Data Center's page titled, "Understanding the Supplemental Security Income (SSI) Program."134
Residency Requirements
To qualify for SSI, individuals or couples must reside in United States, which the program defines as the 50 states, the District of Columbia, and the Commonwealth of the Northern Mariana Islands.135 People residing in Puerto Rico, Guam, the U.S. Virgin Islands, American Samoa, or any other territory or possession of the United State (other than the Northern Mariana Islands) are considered to be residing outside of the United States and thus are ineligible for SSI. However, residents of these territories may become eligible for SSI if they move to one of the 50 states, the District of Columbia, or the Northern Mariana Islands, establish residency there, and meet the physical presence requirement.
|
Cash Assistance for the Aged, Blind, and Disabled in the Territories The Supplemental Security Income (SSI) program is not available in Puerto Rico, Guam, and the U.S. Virgin Islands. Instead, these territories continue to operate the joint federal-state programs for the aged, blind, and disabled, which SSI replaced in the 50 states and the District of Columbia in 1974. These programs offer federal funds (up to a specified amount) to the territories in the form of capped categorical matching grants to help pay for the costs of providing cash assistance to needy aged, blind, or disabled adults aged 18 or older. Guam and the U.S. Virgin Islands operate separate programs of Old-Age Assistance (OAA), Aid to the Blind (AB), and Aid to the Permanently and Totally Disabled (APTD) under Titles I, X, and XIV of the Social Security Act, respectively.136 Puerto Rico operates the consolidated program of Aid to the Aged, Blind, or Disabled (AABD) under Title XVI as it existed prior to reenactment by P.L. 92-603.137 The Administration for Children and Families (ACF) within the Department of Health and Human Services (HHS) oversees the matching-grant programs at the federal level. Neither SSI nor the matching-grant programs are available in American Samoa. SSI was extended to the Commonwealth of the Northern Mariana Islands as part of its 1976 covenant (P.L. 94-241), effective January 1978. |
Individuals or couples are generally ineligible for SSI for months in which they are not physically present in the United States (as defined above). A person who leaves the United States for 30 consecutive days or more is treated as remaining outside the United States until he or she has returned to and remained in the United States for a period of 30 consecutive days.138 The physical presence requirement does not apply to blind or disabled children of military personnel assigned to permanent duty ashore outside the United States139 or to certain students who are temporarily abroad.140
Citizenship Requirements
In addition to the residency requirement, a person must be a citizen or national of the United States or an eligible noncitizen.141 For the purposes of this report, an eligible noncitizen is an alien who (1) has been granted a qualifying legal status by the federal government (i.e., is a qualified alien) and (2) meets certain other requirements.142 As a result of changes made to federal law under the Personal Responsibility and Work Opportunity Reconciliation Act of 1996 (PRWORA; P.L. 104-193) as well as legislation enacted shortly thereafter,143 SSI eligibility for noncitizens is limited largely to lawful permanent residents (LPRs, also known as green card holders) with significant past work history in jobs covered by Social Security, "grandfathered aliens" who received SSI when PRWORA was enacted, certain aliens who are exempted by law from PRWORA's requirements, and refugees and asylees.144 Eligible noncitizens do not include aliens who are not authorized to be present in the United States (i.e., "illegal aliens"), nor do they include aliens with certain types of legal (or quasi-legal) status.145 For example, SSI is not available to aliens lawfully admitted to the United States on tourist visas or to beneficiaries of the Deferred Action for Childhood Arrivals (DACA) policy.
Eligible noncitizens are often classified into two groups: (1) those without a time limit and (2) those subject to a seven-year limit. Eligible noncitizens without a time limit include, but are not limited to, the following categories:
- LPRs who (1) have satisfied a five-year waiting period requirement from the date of entry and (2) have 40 qualifying quarters of coverage from earnings based on Social Security-covered work (or can be credited with such qualifying quarters from a parent or spouse);
- qualified aliens who are (1) active duty military members, (2) honorably discharged veterans, or (3) the dependents of active duty military members or honorably discharged veterans;
- qualified aliens who are lawfully residing in the United States and were receiving SSI on August 22, 1996;
- qualified aliens who were lawfully residing in the United States on August 22, 1996, and who meet SSI's blindness or disability standard, regardless of the onset date;
- American Indians born in Canada who are admitted to the United States under certain conditions; and
- American Indians who are members of federally-recognized tribes and who meet certain conditions.146
Eligible noncitizens subject to a seven-year limit from the date their status was acquired include, but are not limited to, the following categories:
- refugees and asylees who meet certain conditions;
- Cuban/Haitian entrants and Amerasian immigrants who meet certain conditions;147
- quailed aliens whose deportation is being withheld or whose removal has been withheld (subject to certain conditions);
- Iraqi or Afghan nationals who are admitted to the United States under special immigrant visa (SIV) programs;148 and
- aliens who are deemed to be victims of severe forms of human trafficking and who meet certain other conditions.149
In December 2016, eligible noncitizens made up 6.1% of the total SSI recipient population.150 About 11% of all noncitizen recipients received time-limited payments.151 The average federally administered payment made to all noncitizen recipients that month was $510.152 Roughly 71% of all noncitizen SSI recipients were aged 65 or older, and about 58% of all noncitizen recipients resided in the United States for at least 10 years before applying for SSI.153 Since the enactment of PRWORA, both the number and share of noncitizen SSI recipients has fallen.
Other Requirements
Residents of public institutions (such as a jail, prison, or other facility operated directly or indirectly by a governmental entity) are ineligible for SSI for any month throughout which they reside in such institution.154 In other words, a person is ineligible to receive SSI for any full calendar month in which they are in residence. This requirement does not apply to publicly operated community residences that serve 16 or fewer residents.155 It also does not apply to medical treatment facilities in which more than 50% of the cost of care is paid for by Medicaid or, in the case of a child under 18 years old, by any combination of Medicaid and private health insurance.156 In addition, a person is required to file for all other applicable benefits for which he or she may be eligible.157 Furthermore, a person must not be fleeing to avoid (1) prosecution for certain felonies, (2) custody or confinement after conviction for certain felonies, or (3) recapture because of escape from custody.158 Finally, a person must allow SSA to contact his or her financial institutions for purposes of determining or redetermining eligibility.159
Termination Events
In general, SSI payments are suspended for any month during which a recipient fails to meet the aforementioned eligibility requirements. After 12 consecutive months of payment suspension, most recipients are terminated from the SSI rolls and must file a new application.160 In 2016, the SSI termination rate—the ratio of the number of terminations to the average number of SSI recipients during the year for a given age group—was 7.7% for children and 10.0% for working-age adults (Table 4). In 2016, the majority of SSI terminations for children were due to excess income or no longer meeting the applicable definition of disability. For working-age adults that year, most terminations were due to excess income or death.
Table 4. Number and Share of Nonelderly Blind or Disabled SSI Recipients Terminated and the Annual Termination Rate, by Age Group and Reason for Termination, 2016
|
Reason for Termination |
Under 18 Years Old |
Aged 18-64 |
||||||||||||||
|
Terminations |
Termination Rate |
Terminations |
Termination Rate |
|||||||||||||
|
Number |
Share |
Number |
Share |
|||||||||||||
|
Total |
|
|
|
|
|
|
||||||||||
|
Excess Income |
|
|
|
|
|
|
||||||||||
|
Death |
|
|
|
|
|
|
||||||||||
|
Whereabouts Unknown |
|
|
|
|
|
|
||||||||||
|
Excess Resources |
|
|
|
|
|
|
||||||||||
|
In Public Institution |
|
|
|
|
|
|
||||||||||
|
Failed to Furnish Report |
|
|
|
|
|
|
||||||||||
|
Outside United States |
|
|
|
|
|
|
||||||||||
|
No Longer Disabled |
|
|
|
|
|
|
||||||||||
|
Other |
|
|
|
|
|
|
||||||||||
Source: CRS, based on the following sources: SSA, ORES, SSI Annual Statistical Report, 2016, November 2017, Table 77, https://www.ssa.gov/policy/docs/statcomps/ssi_asr/2016/sect11.html#table77; and SSA, "SSI Monthly Statistics, December 2017," January 2018, Table 2.
Notes: The termination rate is the ratio of the number of terminations to the average number of SSI recipients during the year for a given age group. In 2016, the average number of SSI recipients under 18 years old was 1,201,455, and the average number of SSI recipients aged 18-64 was 4,833,829.
Cash Payments
Federal Benefit Rate (FBR)
In 2018, the federal benefit rate (FBR) is $750 per month for an individual living in his or her own household and $1,125 per month for a couple living in their own household.161 On an annualized basis, the FBR in 2018 is $9,000 for an individual and $13,500 for a couple. Individuals and couples with no countable income receive the maximum SSI payment; those with countable income below the applicable FBR have their SSI payment reduced so that their own income plus the reduced SSI payment equals at least the FBR.162 In this way, the FBR acts as an income floor, providing a minimum level of support in 2018 equal to at least 74% of the federal poverty level (FPL) for an individual and 82% of FPL for a couple.163 As noted earlier, the FBR is adjusted annually for inflation by the same COLA applied to Social Security benefits.164 The COLA effective for SSI payments at the start of 2018 was 2.0%, which raised the FBR for an individual from $733 to $750 per month and the FBR for a couple from $1,103 to $1,125 per month.165
State Supplementary Payments (SSPs)
Some states complement federal SSI payments with state supplementary payments (SSPs) that are made solely with state funds.166 SSPs are intended to help individuals whose basic needs are not met fully by the FBR. States may provide SSPs to all SSI recipients, or they may limit payments to certain recipients, such as blind individuals or residents of domiciliary-care homes. Currently, 43 states and the District of Columbia have optional state supplementation programs.167 Most states are required to continue to operate mandatory minimum supplementation programs for certain individuals who were converted to SSI in 1974 from the former federal-state cash assistance programs for the aged, blind, and disabled.168 North Dakota, the Northern Mariana Islands, and West Virginia do not operate any supplementation programs.169
States may self-administer their supplementation programs or contract with SSA for the agency to issue SSPs to eligible recipients on the states' behalf.170 In states that contract with SSA to administer their supplementation programs, SSI recipients receive a single payment composed of the federal SSI payment and the SSP. In states that self-administer their supplementation programs, SSI recipients receive separate payments for SSI and SSP. States that elect federal administration of their supplementation program reimburse SSA for the cost of the SSPs that the agency makes to eligible recipients on behalf of the state.171 Since FY1994, SSA has charged participating states for the cost of administering their program by assessing a user fee on each SSP made by the agency based on a fee schedule prescribed in federal law.172
SSA administers optional SSPs for all (or nearly all) SSI recipients in California, New Jersey, Nevada, and Vermont. The agency also administers optional SSPs for a small number of SSI recipients in special living arrangements (e.g., domiciliary care homes, medical treatment facilities) in the following areas: Delaware, the District of Columbia, Hawaii, Iowa, Michigan, Montana, Pennsylvania, and Rhode Island.173 In December 2017, almost 1.5 million individuals received a federally administered SSP from SSA, approximately 84% of whom lived in California.174 All other SSI recipients live in states that (1) self-administer SSPs for their living arrangement, (2) do not provide SSPs for their living arrangement, or (3) do not operate an optional supplementation program at all. SSA stopped publishing data on SSI recipients who receive state-administered SSPs in 2011.175 Of the 44 areas that operated optional supplementation programs in 2017, only 22 provided SSPs to SSI recipients living in their own household, which is the most frequent type of living arrangement for SSI recipients.176
Basic Payment Calculation Example
As noted earlier, certain income is disregarded in determining SSI eligibility and the amount of assistance. For example, the program excludes the first $20 per month of any income (earned or unearned) and the first $65 per month of earned income plus one-half of any earnings above $65.177 After the application of the $20 general income exclusion, the offset for unearned income is $1 for $1; in other words, the SSI payment is reduced by one dollar for each dollar of unearned income. For earned income above $65 (or $85 if the individual has no unearned income), the offset is $1 for $2; that is, the SSI payment is reduced by one dollar for every two dollars of earned income.178 Income used for certain expenses is also excludable.
Table 5 shows an example of how a SSI payment is calculated for an individual living in his or her own household who receives a $361 monthly SSDI benefit and has earnings of $289 each month. The $20 general income exclusion is first applied to unearned income, meaning that only $341 of the SSDI benefit is countable. Next, the $65 earned income exclusion is applied to the $289 in earnings; the remaining $224 in earnings is counted on a 50% basis (i.e., a $1 for $2 offset). Finally, earned and unearned countable income are summed and then subtracted from the $750 FBR, which results in a monthly SSI payment of $297.
|
Step |
Amount |
Description |
|
(1) Countable Unearned Income |
$361 |
SSDI Benefit |
|
-20 |
General Income Exclusion |
|
|
$341 |
Countable Unearned Income |
|
|
(2) Countable Earned Income |
$289 |
Earnings |
|
-65 |
Earned Income Exclusion |
|
|
$224 |
||
|
-112 |
½ of Remaining Earnings |
|
|
$112 |
Countable Earned Income |
|
|
(3) Total Countable Income |
$341 |
Countable Unearned Income |
|
+112 |
Countable Earned Income |
|
|
$453 |
Total Countable Income |
|
|
(4) SSI Payment |
$750 |
2018 Federal Benefit Rate (FBR) for an Individual |
|
-453 |
Total Countable Income |
|
|
$297 |
Monthly SSI Payment |
Source: CRS.
Notes: The example is of an individual who (1) lives in his or her own household, (2) is not eligible for a SSP, and (3) uses no other income exclusions other than those shown.
Gross Income Breakeven Points
Individuals are ineligible for a monthly SSI payment if their countable income reduces the FBR to $0.179 The amount of gross income a person can have so that countable income equals the applicable FBR is known as the income breakeven point. The dollar amount of the breakeven point in 2018 depends on the type of other income that an individual or couple receives. If a person has only unearned income, the unearned income breakeven point is $770 per month for an individual and $1,145 for a couple (i.e., the applicable FBR plus the $20 general income exclusion). However, if the person has only earned income, the earned income breakeven point is $1,585 per month for an individual and $2,335 for a couple (i.e., 2 x the applicable FBR plus the combined $85 earned income exclusion).180 Depending on the composition of other income, a person who receives both earned and unearned income in 2018 faces a breakeven point somewhere between $770 and $1,585 per month for an individual and between $1,145 and $2,335 per month for a couple.181 However, most people who receive SSI have no other income, and of those recipients who do, only about 3% have any earnings from work in a given month.182
Reduced SSI Payment for Residents of Certain Medical Facilities
Residents of public institutions are generally ineligible for SSI payments, because the institution provides for their basic needs. However, residents of medical treatment facilities in which more than 50% of the cost of their care is paid for by Medicaid (or in the case of a child under 18 years old, by any combination of Medicaid and private health insurance) are eligible for a reduced SSI payment of no more than $30 per month (or $60 per month for couples in certain situations).183 The reduced SSI payment, which is also known as a personal needs allowance, is used to pay for small comfort items not provided by the facility. Any countable income reduces the $30 payment for institutionalized individuals; however, the full FBR is used in determining their eligibility for SSI ($750 per month for an individual in 2018). The reduced SSI payment is not indexed to inflation and has remained at its current level since July 1988. In December 2016, 1.5% of SSI recipients received institutional care in an approved medical facility.184
Average and Total Monthly Payment Levels
As shown in Table 6, the average SSI payment in December 2017 was $542, which on an annualized basis was $6,504. That month, SSA made about $4.7 billion in payments. These amounts include federally administered SSPs but exclude state-administered SSPs. Payments are generally lower for seniors because some of them receive Social Security, which is counted as unearned income against the FBR (or the FBR plus the amount of the applicable federally administered SSP). Payments for children are typically higher because they often do not have income of their own.
Table 6. Average and Total Monthly Payment Amounts of SSI Recipients, by Type of Payment and Age Group, December 2017
|
Age Group |
Number |
Payment Amount |
Total Monthly Payments (in thousands) |
|
Total |
8,227,676 |
$542 |
$4,754,456 |
|
Under 18 Years Old |
1,182,593 |
647 |
810,752 |
|
Aged 18-64 |
4,805,112 |
564 |
2,959,560 |
|
Aged 65 or Older |
2,239,971 |
437 |
984,144 |
Source: CRS, based on SSA, ORES, "SSI Monthly Statistics, 2017." January 2018, Tables 2, 6, and 7.
When SSI Payments Start
Unlike SSDI benefits, SSI payments are not subject to a waiting period requirement. SSI payments begin (1) the first day of the month following the date the application is filed, or (2) the first day of the month following the date the individual becomes eligible for payments.185 It is important to note that SSI recipients are not eligible for retroactive payments for months in which they met all other eligibility criteria prior to the month of application. Retroactive benefits are only available under the Social Security program. However, claimants may be owed past-due payments for months in which they met all eligibility requirements after the month they filed an application through the month their claim is approved.
Medicaid
In addition to cash payments, most SSI recipients qualify for health coverage under Medicaid.186 Established under Title XIX of the Social Security Act, Medicaid is a joint federal-state program that finances the delivery of primary and acute medical services, as well as long-term services and supports (LTSS), to certain needy populations, including the aged, blind, and disabled.187 SSI recipients often have medical conditions that require significant health care resources. However, many SSI recipients are unable to work enough to gain health insurance through an employer or to pay for such insurance on their own. Medicaid provides most SSI recipients with health coverage, including some LTSS that private health insurance and Medicare do not cover, making it an important program for individuals with significant long-term care needs. In FY2015, estimated spending per disabled Medicaid enrollee under 65 years old (including children) was $19,500.188 In 2016, approximately 94% of SSI recipients aged 18-64 reported Medicaid coverage.189
SSI is a mandatory Medicaid eligibility pathway, which means that states are required by law to cover SSI recipients.190 In general, individuals in receipt of SSI for a given month are also eligible for Medicaid for that month, provided they meet all other Medicaid eligibility requirements. SSI recipients typically become ineligible for Medicaid whenever their cash payments are suspended or terminated. However, states are afforded a certain degree of flexibility in this arrangement concerning (1) the Medicaid application process for SSI recipients and (2) the specific eligibility criteria applied to SSI recipients. Consequently, states are categorized into three groups with respect to Medicaid eligibility for SSI recipients:
- states that use SSI's eligibility criteria and do not require a separate application (i.e., "1634 states");
- states that use SSI's eligibility criteria but require a separate application (i.e., "SSI criteria states"); and
- states that use more restrictive eligibility criteria than SSI's criteria and require a separate application (i.e., "209[b] states").
The following subsections discuss the three groups in more detail.
1634 States
Thirty-four states and the District of Columbia grant Medicaid coverage automatically to individuals who become eligible for SSI. Section 1634 of the Social Security Act allows states to contract with SSA for the agency to perform Medicaid eligibility determinations for their SSI recipients as part of the SSI application process.191 In other words, an SSI application in these states is also an application for Medicaid. States that elect to contract with SSA for these Medicaid determinations are known as 1634 states. In December 2017, 85.8% of all SSI recipients resided in these areas.192
SSI Criteria States
Eight states and the Northern Mariana Islands use the same income, resource, and disability standards of the SSI program to determine Medicaid eligibility for SSI recipients but require them to file a separate application for Medicaid with the state or local Medicaid office. States that elect this option are known as SSI criteria states. The eight SSI criteria states are Alaska, Idaho, Kansas, Nebraska, Nevada, Oklahoma, Oregon, and Utah. In December 2017, 4.8% of all SSI recipients resided in these areas.193
209(b) States
The remaining eight states use more restrictive eligibility criteria than SSI's criteria to determine Medicaid eligibility for SSI recipients. Under Section 1902(f) of the Social Security Act, states may elect to use at least one eligibility criterion more restrictive than SSI's criteria in making Medicaid eligibility determinations for SSI recipients, provided any state-established standard is no more restrictive than the standards used by the state's Medicaid program in 1972.194 States that elect to apply more restrictive standards are known as 209(b) states, after the section of the Social Security Amendments of 1972 (P.L. 92-603) that established the option. The eight 209(b) states are Connecticut, Hawaii, Illinois, Minnesota, Missouri, New Hampshire, North Dakota, and Virginia.195 In December 2017, 9.4% of all SSI recipients resided in these areas.196
209(b) states may use a stricter definition of blindness or disability, a lower income or resource standard, a less generous methodology for counting income or resources, or some combination of those factors. For example, New Hampshire imposes a longer duration-of-impairment requirement for individuals with a disability other than blindness (48 months instead of SSI's 12-month standard),197 while Virginia limits ownership of property contiguous to the individual's home (i.e., land other than the lot occupied by the home) to $5,000.198 However, 209(b) states that use a more restrictive income standard than the SSI program must deduct incurred medical expenses from an SSI recipient's income in determining Medicaid eligibility.199 This requirement allows SSI recipients to spend down their income to the state-established income standard.
Since the enactment of the Patient Protection and Affordable Care Act (ACA; P.L. 111-148, as amended), three states have dropped their 209(b) status as part of larger efforts to reform their Medicaid programs. Specifically, Oklahoma elected to become a SSI criteria state effective October 1, 2015,200 while Indiana and Ohio elected to become 1634 states effective June 1, 2014,201 and August 1, 2016, respectively.202
SNAP
Because SSI recipients are by definition low income, the Supplemental Nutrition Assistance Program (SNAP; formerly the Food Stamp Program) confers eligibility automatically to SSI eligible individuals in certain living situations. SNAP is a federally funded assistance program, administered jointly with the states, that provides benefits to eligible households on an electronic benefit transfer (EBT) card, which can be redeemed for foods at authorized retailers.203 Under SNAP law, individuals living in pure SSI households—those in which all members receive SSI payments—are categorically eligible for SNAP.204 SSI recipients living in mixed households may also qualify for SNAP if their household meets SNAP's traditional eligibility requirements.205 In 2016, an estimated 52% of SSI recipients aged 18-64 lived in households that received SNAP benefits.206 (California provides SSI recipients with a higher federally administered SSP in lieu of SNAP benefits.)207
Financing
Federal SSI payments and administrative costs are financed from the general fund of the U.S. Treasury. SSPs are financed solely with state funds. States reimburse SSA for the cost of SSPs made to their eligible recipients and for the cost of administering their supplementation program. In FY2017, total federal SSI outlays were $58.7 billion, with $54.6 billion for benefit payments and $4.1 billion for administrative and other costs.208 Spending on federally administered SSPs in FY2017 was $2.6 billion.209 In 2016, about 93% of spending on federally administered SSPs was attributable to SSI recipients living in California.210
In their August 2017 report and under current law, SSA's actuaries project that spending on federal SSI payments will increase (in CPI-indexed 2017 dollars) from $54.6 billion in 2017 to $61.5 billion in 2041.211 As a share of gross domestic product (GDP), SSA's actuaries project that spending on federal SSI payments will decrease from 0.28% in 2017 to 0.20% in 2041.212 Under its April 2018 baseline and under current law, CBO projects that spending on federal SSI payments will increase (in nominal dollars) from $54.6 billion in FY2017 to $80.8 billion in FY2028.213
Concurrent Disability Beneficiaries
(Hereinafter the term SSDI beneficiary refers to disabled workers, disabled widow[er]s, and disabled adult children of retired, disabled, or deceased insured workers. In addition, the term SSI disability recipient refers to blind or disabled SSI recipients under 65 years old.)
In December 2016, about 12.8 million adults aged 18-64 received SSDI or SSI due to a qualifying impairment (Figure 3). Of those, more than 1.3 million (or 10%) received both types of disability benefits. About one in seven SSDI beneficiaries aged 18-64 received SSI concurrently. At the same time, about a quarter of SSI disability recipients aged 18-64 also received SSDI. For this report, individuals who receive both SSDI and SSI due to a qualifying impairment are referred to as concurrent disability beneficiaries. Assuming they meet the applicable eligibility requirements, concurrent disability beneficiaries receive health coverage under Medicare and Medicaid. Individuals who qualify for both health care programs are known as dual eligibles.
The average combined benefit for concurrent disability beneficiaries in December 2016 was $783 (Table 7). Of that amount, $538 was from SSDI and $245 was from SSI. Because average benefits for concurrent disability beneficiaries were below the FBR for an individual ($733 per month in 2016) and because SSDI benefits generally offset SSI payments on a dollar-for-dollar basis, combined benefit levels for each type of concurrent SSDI beneficiary were about the same. Thus, disabled workers (who have higher average SSDI benefit amounts) received lower average SSI payments, and disabled adult children (who have lower average SSDI benefit amounts) received higher SSI payments, resulting in roughly the same combined disability benefit amount across all three beneficiary types.
Table 7. Number of Concurrent Disability Beneficiaries Aged 18-64 and Average Benefit Amount, by Type of SSDI Beneficiary, December 2016
|
Type of SSDI Beneficiary |
Number of Concurrent Beneficiaries |
Average Monthly Benefit |
||
|
Combined |
SSDI |
SSI |
||
|
Total |
1,310,459 |
$783 |
$538 |
$245 |
|
Disabled Workers |
951,118 |
784 |
560 |
225 |
|
Disabled Widow(er)s |
29,784 |
787 |
544 |
244 |
|
Disabled Adult Children |
329,557 |
777 |
475 |
303 |
Source: CRS, based on SSA, ORES, SSI Annual Statistical Report, 2016, November 2017, Tables 15 and 16.
Notes: Subtotals may not sum to totals due to rounding. The term SSDI includes disabled workers, disabled widow(er)s, and disabled adult children of retired, disabled, or deceased workers.
As shown in Figure 4, the average benefit amount for concurrent disability beneficiaries is higher than that for SSI-only recipients but is lower than that for SSDI-only beneficiaries. The purpose of SSI for adults is generally twofold: (1) to provide cash assistance to aged, blind, or disabled individuals who have no income and (2) to supplement the incomes of those who have low Social Security benefits. For SSDI beneficiaries with minimal benefits and other income, SSI increases their overall monthly disability benefit from SSA.
Definition of Disability
SSDI and Adult SSI Claimants
SSDI and SSI use a total work-limiting definition of disability for adults; in other words, an individual's impairment(s) must significantly interfere with his or her ability to earn a living.214 Most adults are considered disabled for SSDI and SSI eligibility purposes if they are "unable to engage in any substantial gainful activity by reason of any medically determinable physical or mental impairment that can be expected to result in death or that has lasted or can be expected to last for a continuous period of not less than 12 months."215 Adults generally qualify as disabled for SSDI and SSI purposes if they have an impairment (or combination of impairments) of such severity that they are unable to perform any kind of substantial work that exists in significant numbers in the national economy, taking into consideration their age, education, and work experience. The work need not exist in the immediate area in which the claimant lives nor must a specific job vacancy exist for the individual.
Child SSI Claimants
The SSI program uses a special definition of disability for children because minors are generally not expected to work. Individuals under 18 years old must have "a medically determinable physical or mental impairment, which results in marked and severe functional limitations, and which can be expected to result in death or which has lasted or can be expected to last for a continuous period of not less than 12 months."216 Children typically qualify as disabled if they have a severe impairment (or combination of impairments) that limits their ability to engage in age-appropriate childhood activities at home, in childcare, at school, or in the community. In addition, the child must be unable to perform substantial gainful activity (SGA).
Substantial Gainful Activity (SGA) Earnings Limits
Under SSA's regulations for SGA, work activity is considered substantial if it involves doing significant physical or mental activities, even if it is done on a part-time basis.217 Work activity is considered gainful if an individual does it for pay or profit, regardless of whether the profit is realized or legal.218
SSA uses a monetary threshold to determine whether an individual's work activity constitutes SGA, which the agency adjusts annually to reflect changes in national earnings levels. For SSDI, the SGA earnings threshold in 2018 is $1,180 per month for most individuals and $1,970 per month for statutorily blind individuals.219 Under the SSI program, SGA rules do not apply to statutorily blind individuals. Because of certain SSI work incentives, the non-blind SGA earnings threshold applies to individuals with a condition other than blindness only at the time of application for SSI.220
The SGA threshold for blind individuals under the SSDI program is specified in statute,221 while the SGA threshold for non-blind individuals under the SSDI and SSI programs is specified in regulations by SSA.222 The SGA threshold for blind individuals under the SSDI program is adjusted annually for average earnings growth in the economy, provided a COLA is payable for that year. On the other hand, the SGA threshold for non-blind individuals under both programs is adjusted annually for average earnings growth in accordance with the agency's regulations, regardless of whether a COLA is payable for the year. Thus, in years when a COLA is not payable, the SGA threshold for blind individuals under the SSDI program remains the same as the amount for the previous year, while the SGA threshold for non-blind individuals is adjusted according to the formula specified in regulations, which may result in a higher threshold.
Drug Addiction and Alcohol (DAA)
Section 105 of the Contract with America Advancement Act of 1996 (P.L. 104-121) amended the Social Security Act to bar SSA from considering an individual disabled if drug addiction or alcoholism (DAA) is a contributing factor material to the determination that the individual is disabled.223 SSA's policy interpretation of this requirement is specified in Social Security Ruling (SSR) 13-2p.224 DAA is a substance use disorder as defined in the latest edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM). SSA considers an individual to have DAA if he or she has a medically determinable substance use disorder documented by objective medical evidence from an acceptable medical source. The DAA is considered material to the determination of disability if the individual would not meet the definition of disability if he or she were not using drugs or alcohol.225 It should be noted that nothing in the Social Security Act precludes an individual from qualifying for SSDI or SSI for using drugs or alcohol (including medical and recreational marijuana).226 The act simply prevents individuals from qualifying for benefits if their DAA is material to their disability determination or contributes to their inability to follow prescribed treatment (discussed below). In 2015, approximately 7.0% of all working-age SSDI beneficiaries and SSI disability recipients reported drug or alcohol abuse in the past 12 months.227
Following Prescribed Treatment
The Social Security Act requires individuals to follow treatment prescribed from their medical source(s) if such treatment is expected to restore their ability to work (i.e., engage in SGA).228 If an individual fails to follow the prescribed treatment without good reason, SSA will not consider the individual to be disabled for purposes of SSDI or SSI. In some instances, the individual's DAA may interfere with his or her ability to follow prescribed treatment. A 2015 report from SSA's Office of the Inspector General (OIG) noted the following case:
An individual applied for disability benefits for seizures, high blood pressure, and poor eyesight. The medical evidence showed she was prescribed three doses of an anti-seizure medication per day; however, she only took two doses. She claimed she was taking only two doses to stretch the medication. However, because evidence in the file showed she was also using cocaine and marijuana, she had the means to purchase her medication as she had the means to purchase non-prescription drugs. The evidence showed that proper medication management should significantly reduce her seizure issues. Therefore, SSA denied the claim for failure to follow prescribed treatment.229
Comparisons with Other Program Definitions of Disability
The definitions of disability under Titles II and XVI of the Social Security Act are considered total and long-term; neither program pays benefits to individuals with partial or short-term impairments. SSA's all-or-nothing definitions of disability are different from other disability standards. For example, the VA provides partial or total disability benefits to veterans with qualifying impairments on a scale from 0% to 100% (in 10% increments).230 In addition, state workers' compensation pays benefits for total or partial occupational-related injuries and illnesses that are permanent or temporary.231 According to SSA, the Social Security Act's "purpose and specific eligibility requirements for disability and blindness differ significantly from the purpose and eligibility requirements of other programs."232
Application and Initial Determination Process233
The process begins when a claimant files an initial application for SSDI or SSI using one of four methods: (1) submitting an application in person at one of SSA's more than 1,200 nationwide field offices; (2) contacting a SSA teleservice representative over the phone and relaying the necessary information; (3) sending a paper application by mail; or (4) filing an electronic application on ssa.gov (for SSDI and certain concurrent claims only). If the agency requires more information to process the application, it will contact the claimant by phone or arrange for an in-person interview at the local field office. Claimants must inform and submit all evidence to SSA related to their impairment as a condition of their application for benefits.234
Claims representatives at SSA's field offices screen claimants to make sure they meet the applicable non-medical entitlement factors. For SSDI, non-medical factors include disability-insured status, the work activity test (i.e., SGA earnings limit), and the claimant's relationship to certain family members. For SSI, such factors include income, resources, living arrangements, the work activity test (for non-blind claimants), citizenship, residency, and the requirement to apply for all other benefits. In general, claimants who do not meet the applicable non-medical entitlement factors are found to be ineligible for benefits and do not receive a disability determination. SSA field office personnel notify claimants whose applications are denied due to non-medical factors.
Applications that meet the applicable non-medical entitlement factors are forwarded to the disability determination services (DDS) office in the area that has jurisdiction for the disability determination (generally the state in which the claimant resides).235 DDSs, which are fully funded by the federal government, are state agencies tasked with reviewing the medical and vocational evidence and issuing the disability determination for SSA.236 Although DDS workers are state employees, they make the disability determinations based on federal law, regulations, and SSA's policy guidance. DDSs are located in the 50 states, the District of Columbia, Puerto Rico, Guam, and the Virgin Islands, and they employ approximately 15,000 state workers.
The disability determination for both types of benefits is made based on evidence gathered in an individual's case record. Disability examiners—with the help of medical or psychological consultants (who are licensed physicians, psychiatrists, or psychologists)—typically use evidence collected from the claimant's own medical sources to evaluate the existence and severity of the claimant's impairment(s).237 However, if the medical evidence is unavailable or insufficient to make a determination, disability examiners can schedule a physical or mental examination or test from a medical source to obtain the necessary information. In such cases, SSA pays for the consultative examination (CE).238 The initial review generally does not involve a face-to-face meeting between the claimant and the adjudicator (i.e., the claim is decided based solely on the evidence in the claims file). After considering all medical and other evidence, the DDS agency issues a disability determination and returns the case to the SSA field office. If the claim is approved, the SSA field office sends out the initial award notice and begins processing the claim. If the claim is denied, the DDS agency prepares a personalized disability explanation and notifies the claimant of the decision.
Disability Determinations for SSDI and Adult SSI Claimants
The Social Security Act gives the Commissioner of Social Security broad authority to promulgate regulations specifying the standards, administrative requirements, and procedures used in conducting disability determinations.239 Under its regulations, SSA employs a five-step sequential evaluation process to determine whether a claimant's medical condition meets the definition of disability prescribed in the act for SSDI and adult SSI claimants (Figure 5).240
Each step in the process is followed in a set order. If SSA finds a claimant disabled or not disabled at a given step, the initial disability determination process is completed and a decision by the agency is made. If SSA cannot find a claimant disabled or not disabled at a given step, the agency proceeds to the next step.
Step 1. Work Activity Test
The SSA field office assesses whether a claimant's level of work activity constitutes SGA.241 In 2018, most claimants are found able to engage in SGA if their countable earnings average more than $1,180 per month.242 Countable earnings equal gross earnings minus applicable exclusions. Blind SSDI claimants are found able to perform SGA if their countable earnings average more than $1,970 per month. (SGA rules do not apply to statutorily blind SSI claimants.)
To determine countable earnings, SSA first documents a claimant's gross earnings for each month during the relevant period of work.243 The agency then considers whether the claimant's work was performed under any special conditions, such as in sheltered employment or under certain government-sponsored job training or employment programs. Earnings or other compensation derived from work performed under special conditions may be deducted (in part or in whole) from gross earnings. Reasonable costs for certain impairment-related work expenses (IRWE)—such as attendant care services or medical equipment—may also be deducted if the claimant needs such expenses to work. Once a claimant's countable earnings have been calculated and added together, SSA divides them over the number of months in the relevant review period to produce a monthly average. Claimants with countable monthly earnings at or below the applicable SGA limit proceed to the next step of the disability determination process. Those with countable monthly earnings above the applicable SGA limit are found not disabled, and their application is denied.
Step 2. Severity and Duration Test
The DDS agency determines whether available medical evidence establishes a physical or mental impairment (or combination of impairments) of sufficient severity to prevent the claimant from engaging in SGA and, if so, whether the impairment(s) can be expected to last for at least 12 months or to result in death. In making this determination, the DDS agency first verifies the existence of a medically determinable impairment using objective medical evidence (i.e., medical signs or laboratory findings) from the claimant's acceptable medical sources.244 A claimant is considered to have a medically determinable impairment if such evidence shows the existence of one or more anatomical, physiological, or psychological abnormalities.
Once a medically determinable impairment has been established, the adjudicative team evaluates the severity of the impairment using all available evidence, including medical opinions and statements of symptoms from the claimant. Symptoms, such as pain or fatigue, are considered if the objective medical evidence from acceptable medical sources shows that the impairment(s) could reasonably be expected to produce the symptoms.245 The DDS agency then evaluates the intensity and persistence of the claimant's symptoms to determine the extent to which such symptoms interfere with the claimant's ability to work. A claimant's impairment(s) is ultimately considered severe if it significantly limits his or her physical or mental ability to do basic work activities. Basic work activities include the following: walking, standing, sitting, lifting, pushing, pulling, reaching, carrying, or handling; seeing, hearing, and speaking; understanding, carrying out, and remembering simple instructions; use of judgment; responding appropriately to supervision, coworkers, and usual work situations; and dealing with changes in a routine work setting.246 A claimant's impairment(s) is considered not severe if it has only a "minimal effect" on his or her ability to perform basic work activities required in most jobs.
In evaluating the claim at Step 2, the DDS agency is required to consider the combined effect of all the claimant's impairments without regard to whether any such impairment, if considered separately, would be of sufficient severity.247 Thus, a claimant may meet the severity requirement if he or she has multiple non-severe impairments that when combined, have the same effect on the claimant's ability to function as a single severe impairment. Lastly, in addition to being severe, the claimant's medically determinable impairment(s) must be expected to result in death or have lasted or be expected to last for a continuous period of not less than 12 months.248 Claimants who meet the severity and duration requirements proceed to the next step. Those who do not are found not disabled and their application is denied.
Step 3. Medical Listings Test
At Step 3, the DDS agency determines whether the claimant's medically determinable impairment(s) meets the medical criteria of an impairment specified in SSA's Listing of Impairments (also known as the Blue Book).249 The listings describe medically determinable impairments for each body system that the agency considers severe enough to prevent a claimant from performing any gainful activity, regardless of the claimant's age, education, or work experience.250 Most listed impairments are permanent or expected to result in death. All other listed impairments are expected to last for at least 12 months or for a specific duration.
The listings for adults (Part A) are categorized across 14 major body systems, with each category containing examples of common qualifying impairments as well as specific evaluative criteria for confirming their existence. Each listing outlines the impairments applicable to the body system, the medical and other documentation required to evaluate the claim, and the rules used to evaluate the specific impairment, including related symptoms, effects of treatment, and loss of function. For impairments that can be objectively measured, the listing may describe the minimum threshold for a particular diagnostic test. For those that are more subjective to measure, the listing may describe the minimum functional criteria. The listings were created to quickly screen relatively clear-cut cases, leaving adjudicators more time to evaluate more difficult cases at the latter stages of the process.
Claimants qualify at Step 3 of the disability determination process in one of two ways: (1) by meeting the criteria of a specific listing or (2) by equaling the criteria of a specific listing. For claimants to meet a listing, their medically determinable impairment(s) must satisfy all of the criteria described in the listing; a diagnosis alone is insufficient to meet a listing. In other words, claimants must have an impairment described in the listing, meet the objective medical and other findings, and meet the duration requirement.
If claimants are unable to meet a listing, they may be able to equal a listing if their medically determinable impairment(s) at least equals in severity and duration the criteria of any listed impairment.251 Specifically, if the claimant's impairment(s) is described in the listings but he or she does not exhibit one or more findings specific for the listing (or one of the findings does not meet the specified severity), the DDS will find the claimant's impairment(s) medically equivalent to the listing, provided the claimant has other findings related to his or her impairment(s) that are at least of equal medical significance to the required criteria. If the claimant's impairment is not described in the listings but is closely analogous to a listed impairment, the DDS will find the claimant's impairment(s) medically equivalent to the analogous listing if the findings related to the claimant's impairment(s) are at least of equal medical significance to those of the listed impairment.252
Claimants with impairments that meet or equal a listing are found disabled and awarded benefits. Those with impairments that do not meet or equal a listing proceed to Step 4.
Step 4. Previous Work Test
Claimants with severe impairments that do not meet or equal a listed impairment proceed to an individual assessment that examines their remaining ability to work. To make this determination, the adjudicative team conducts a residual functional capacity (RFC) assessment, which is a function-by-function assessment of a claimant's ability to perform sustained, work-related physical or mental activities despite the limitations and restrictions caused by his or her medically determinable impairment(s).253 In general, RFC is a claimant's maximum remaining ability to do sustained work activities in an ordinary work setting on a regular and continuing basis (i.e., eight hours a day, five days a week, or an equivalent work schedule). The RFC assessment is based on all available evidence in the claimant's case record, such as objective medical evidence, activities of daily living (ADL), and statements provided by the claimant or other lay sources (e.g., family, friends, neighbors). In evaluating a claimant's RFC, the DDS agency considers the effects of pain and other symptoms, as well as any non-severe impairments, on the claimant's ability to function in a work setting.
Once the assessment is complete, the DDS evaluates the claimant's RFC with the physical and mental demands of his or her past relevant work.254 Past relevant work is defined as work performed in the past 15 years, at SGA, and which lasted long enough for the claimant to learn to do it.255 The individual's past relevant work need not exist in significant numbers in the national economy.256 If a claimant's medically determinable impairment(s) does not prevent him or her from performing past relevant work, the claimant is found not disabled and the application is denied. If the claimant is found unable to perform past relevant work, the case proceeds to the next step.
Step 5. Any Work Test
At the final stage of the disability determination process, the DDS agency considers whether the claimant can adjust to any other type of work.257 Specifically, the claimant must be unable to do not only his or her previous work but cannot, considering his or her age, education, and work experience, engage in any other kind of substantial gainful work that exists in the national economy.258 Work that exists in the national economy means work that exists in significant numbers either in the region where the claimant lives or in several regions of the country.259 It does not matter whether the work exists in the immediate area where the claimant lives, whether a specific job vacancy exists, or whether the claimant would be hired if he or she applied for such work.
At this stage, the DDS agency uses medical-vocational rules (also known as the grids) to relate the claimant's age, education, and work experience to his or her RFC to perform work-related physical or mental activities.260 The grids cross-reference the aforementioned vocational factors by certain exertional (i.e., strength demands) and skill levels to determine the limitations and restrictions imposed by the claimant's impairment(s) and related symptoms.261 The DDS agency uses the Department of Labor's Dictionary of Occupational Titles (DOT) for information about the physical and mental demands needed for jobs in the national economy.262 Claimants with impairments that prevent them from adjusting to any other work that exists in the national economy are found disabled and awarded benefits. Claimants with impairments that allow them to adjust to a significant number of jobs in the national economy are found not disabled and their application is denied.
In general, older individuals (i.e., those aged 50 or older) who have limited education and work experience are more likely to be awarded benefits than younger individuals or those who have more education or work experience. For example, all things being equal, a 59 year old coal miner with an 8th grade education and no other work experience is more likely to be awarded benefits than a 45 year old adjunct college professor who has worked several types of jobs in the past.
Disability Determinations for Child SSI Claimants
As noted earlier, because children are generally not expected to work, the SSI program uses a special definition of disability for minors. Individuals under the age of 18 must have a medically determinable physical or mental impairment, which results in marked and severe functional limitations, and which can be expected to result in death or which has lasted or can be expected to last for a continuous period of not less than 12 months. The first part of the disability determination process for child SSI claimants is similar to the one used for SSDI and adult SSI claimants (Figure 6).263
At Step 1, the DDS agency determines whether the child's countable monthly earnings average more than the non-blind SGA earnings limit. At Step 2, the DDS agency determines whether available objective medical evidence from acceptable medical sources establishes a medically determinable impairment, and, if so, whether all medical and other evidence demonstrates that such impairment (or combination of impairments) meets the severity and duration requirements. In determining the severity of the claimant's impairment(s), the DDS agency compares the claimant's functioning to that of children his or her own age who do not have impairments. A child's medically determinable impairment(s) is considered not severe if it is a slight abnormality (or a combination of slight abnormalities) that causes no more than minimal functional limitations. At Step 3a, the DDS agency determines whether the child's medically determinable impairment(s) meets or medically equals the criteria of a specific listing. The listings for children (Part B) are categorized across 15 major body systems and like their adult counterparts, contain examples of common impairment for each body system and specific evaluative criteria for confirming the existence of a qualifying impairment.
|
Figure 6. Initial Disability Determination Process for Child SSI Claimants |
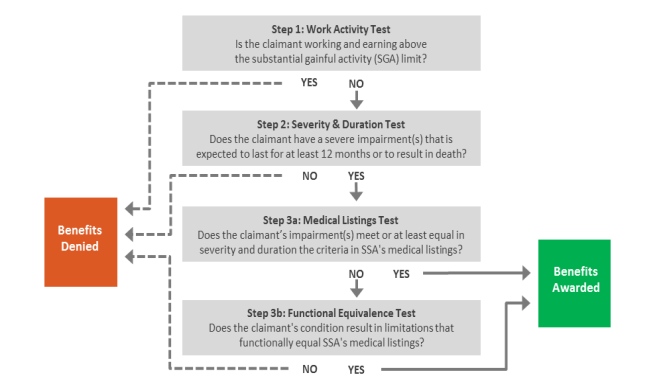 |
|
Source: CRS, based on Subpart P of 20 C.F.R. §404, Subpart I of 20 C.F.R. §416, and Chart 2 in Bernard Wixon and Alexander Strand, Identifying SSA's Sequential Disability Determination Steps Using Administrative Data, Research and Statistics Note no. 2013-01, June 2013, https://www.ssa.gov/policy/docs/rsnotes/rsn2013-01.html. Notes: In 2018, the SGA earnings limit is $1,180 per month and applies only at the time of application. |
If a child has a severe impairment that does not meet or medically equal the criteria of a specific listing, then the case proceeds to Step 3b, where the DDS agency determines whether the impairment(s) results in limitations that functionally equal the listings.264 During this process, the DDS agency assesses the extent to which a child's impairment(s) limits or restricts his or her day-to-day functioning at home, in childcare, at school, or in the community. The DDS agency evaluates a child's functioning across six domains: (1) acquiring and using information; (2) attending and completing tasks; (3) interacting and relating with others; (4) moving about and manipulating objects; (5) self-care; and (6) health and physical well-being. These domains are cross-referenced by age categories that describe age-appropriate functioning and behavior.
At this stage, a claimant's impairment (or combination of impairments) is not evaluated against a specific listing. Rather, it is evaluated on the basis of whether it causes functional limitations that are of listing-level severity, regardless of the nature of the impairment(s). A child's impairment(s) functionally equals the criteria in the listings if it results in marked limitations in at least two of the domains or an extreme limitation in one domain. A marked limitation in a domain occurs when a claimant's impairment(s) interferes seriously with his or her ability to independently initiate, sustain, or complete activities. An extreme limitation in a domain occurs when a claimant's impairment(s) interferes very seriously with his or her ability to independently initiate, sustain, or complete activities. Children are awarded benefits if their impairment(s) meets, medically equals, or functionally equals the listings.
Appeals Process
Individuals who are dissatisfied with SSA's initial determination or decision may request further review under the Social Security Act's administrative and judicial review provisions.265 The appeals process affords claimants the opportunity to present additional evidence or arguments to support their case as well as to appoint a representative to act on their behalf, such as an attorney or a qualified non-attorney.266 The claimant, his or her appointed representative, representative payee,267 or other third party on behalf of the claimant can file a request for review. The request for further review must be made, in writing, within 60 days of the date the claimant received notice of the prior determination or decision (generally five days after the date on the notice), unless SSA determines that the claimant has good cause for failing to file a timely request.268 Claimants may file their appeal using conventional SSA forms or online via the iAppeals system.
SSA's administrative appeals process is generally composed of three levels of review: (1) reconsideration of the case by a reviewer who did participate in the initial determination; (2) a hearing before an administrative law judge; and (3) a request for review by the Appeals Council (Figure 7).269 Individuals may elect to continue to receive benefit payment during this process under certain conditions.270 At each step of the appeals process, the decision-maker bases his or her decisions on provisions in the Social Security Act, SSA's regulations, and other agency guidance. Only after exhausting the administrative appeals process and receiving a final decision from SSA are claimants permitted to file a complaint against the agency in federal court.271 The following section describes each step of the appeals process in more detail.
Step 1. Reconsideration
In general, reconsideration is the first mandatory step of the administrative appeals process that a claimant must initiate in order to appeal an initial determination by SSA.272 Reconsideration involves a thorough review of all evidence in the case record from the initial determination, along with any additional evidence submitted by the claimant. Reconsideration is effectively a new review of the case by the same DDS office that conducted the initial determination except that it is performed by an official who did not participate in the initial determination.273 For cases involving the appeal of a medical determination, a new adjudicative team consisting of a disability examiner and a medical or psychological consultant reexamine the evidence from the initial determination and any new evidence submitted with the appeal. The team may request additional evidence or a new consultative examination. As with the initial level, the reconsideration level generally does not involve a face-to-face meeting between the adjudicator and the individual (i.e., case review).274 However, if the individual received benefit payments (i.e., was a beneficiary or recipient) and contests an initial determination based on medical factors that he or she is not now blind or disabled, then the individual may request a disability hearing, which is a face-to-face reconsideration of the individual's last medical determination.275 After the review has been completed, the adjudicator makes a determination based on the preponderance of the evidence in the case record. The claimant is later notified of the decision in writing.
In 1999, SSA eliminated the reconsideration level in the following states as part of the Disability Redesign Prototype Model: Alaska, Alabama, California (Los Angeles West and North Branches), Colorado, Louisiana, Michigan, Missouri, New Hampshire, New York, and Pennsylvania.276 In these 10 states, claimants who appeal the initial determination skip the reconsideration level and proceed directly to the hearing level. As part of FY2019 President's budget request to Congress, the Trump Administration proposes to reinstate the reconsideration level in the 10 prototype states.277 In addition to the legislative proposal, officials from SSA's Office of Budget informed CRS that the agency plans to use its regulatory authority to gradually reinstate the reconsideration step in the 10 prototypes over the next several years.278
Step 2. Hearing Before an Administrative Law Judge (ALJ)
The second mandatory step of the administrative appeals process (or the first mandatory step for those who reside in one of the prototype states) is to request a hearing before an administrative law judge (ALJ).279 An ALJ is an impartial hearing examiner who issues a de novo (i.e., fresh) decision with respect to the individual's claim for benefits.280 The hearing level is often the first time that a claimant has the opportunity to appeal his or her case face-to-face (either in person or via video teleconferencing). During a hearing, an ALJ investigates the merits of an appeal by informally questioning the claimant, as well as any scheduled witnesses such as medical or vocational experts. A claimant or his or her appointed representative may also present additional evidence, examine evidence used in making the determination under review, introduce witnesses, question witnesses, and present oral or written arguments in support of a favorable decision. In general, all evidence, objections, or written statements must be submitted to SSA at least five business days before the date of the hearing.281 Because SSA is not represented at the hearing, the proceeding is considered inquisitorial (i.e., non-adversarial). An ALJ issues a decision based on the preponderance of the evidence in the hearing record. In certain situations, the ALJ may dismiss a case without making a decision of its merits, such as when a claimant fails to appear for the hearing. The claimant is later notified in writing of the decision or dismissal.
Step 3. Appeals Council (AC)
The third mandatory step of the administrative appeals process is to request a review before the Appeals Council (AC).282 The AC is made up of administrative appeals judges (AAJs), appeals officers (AO), and support personnel. The AC reviews ALJ decisions and orders of dismissal, as well as processes certain court actions.283 The AC may dismiss or deny the request for review, or the AC may grant the request and either issue a decision or remand the case back to an ALJ for further proceedings. The AC may also review an ALJ decision or dismissal on its own motion within 60 days after the date of a decision or dismissal.284 Once the AC decides to review an ALJ decision on its own motion, it may affirm, reverse, or modify the decision (including a favorable decision) or remand the case back to an ALJ for further proceedings. The claimant is notified in writing of the AC's decision or reason for denial of the review.
Step 4. Federal Courts
Only after exhausting the administrative appeals process and receiving a final decision from SSA may a claimant request judicial review by filing a civil action in a federal court.285 The Social Security Act requires that such action be brought in the U.S. district court in the judicial district where the claimant resides (or has a principal place of business) or, if not applicable, the U.S. District Court for the District of Columbia. A district court may issue a decision or remand the case back to SSA for further action. Court remands are initially sent to the AC, which may assume jurisdiction and issue a decision or remand the case to an ALJ for further proceedings and a new decision. On rare occasions, disability cases are appealed beyond U.S. district court to the U.S. court of appeals and, ultimately, the U.S. Supreme Court.
Determinations of Continuing Eligibility
Continuing Disability Reviews (CDRs)
After SSA finds that a claimant is disabled, the agency evaluates his or her impairment(s) from time to time to determine if the individual is still medically eligible for payments on the basis of blindness or disability.286 This evaluation is known as a continuing disability review (CDR). The frequency of a CDR depends on the beneficiary's prospective medical improvement. SSA's regulations specify three basic types of schedules or diaries.
- Medical Improvement Expected (MIE). If medical improvement is expected, then SSA schedules a review at intervals from 6 to 18 months following the most recent decision that the individual is disabled or that disability is continuing. Examples of impairments that fall into this category include traumatic injuries and severe bone fracture.
- Medical Improvement Possible (MIP). If medical improvement is possible but cannot be accurately predicted based on current experience and the facts of the case, then SSA schedules a review at least once every three years. Examples of impairments that fall into this category include heart failure and severe diabetes with end organ damage.
- Medical Improvement Not Expected (MINE). If medical improvement is unlikely due to the severity of an individual's condition, then SSA schedules a review once every five to seven years. Examples of impairments that fall into this category include intellectual disabilities, amyotrophic lateral sclerosis (ALS) which is sufficiently severe, and Parkinson's disease which is sufficiently severe. Individuals who receive this classification are considered permanently disabled by SSA.287
As shown in Figure 8, few SSDI beneficiaries and SSI disability recipients are assigned a MIE diary.
SSA conducts two types of medical CDRs on individuals whose diaries mature: full medical CDRs and mailers.288 A full medical CDR involves SSA sending the case to the state DDS agency for a full medical review. A mailer is a questionnaire sent to the individual in order to obtain additional information, which SSA uses to determine if a full medical CDR is appropriate.289 If the answers to the mailer do not indicate likely improvement, SSA may defer a full medical CDR.
Under current law, SSA must find substantial evidence of medical improvement during a CDR to find a SSDI beneficiary or SSI disability recipient no longer disabled and therefore ineligible for benefits.290 The legal requirement for determining if disability continues during a CDR is called the medical improvement review standard (MIRS). Under a MIRS determination for adults, the agency generally considers a SSDI beneficiary or SSI disability recipient no longer disabled if the review finds considerable evidence that (1) there has been substantial medical improvement in the individual's impairment(s) related to his or her ability to work since the last favorable medical decision and (2) the individual has the ability to engage in SGA. For a child SSI recipient, SSA typically considers the child no longer disabled if the review demonstrates that there has been substantial medical improvement in the recipient's impairment(s) since his or her most recent favorable medical decision to the point in which the recipient's condition no longer meets or medically or functionally equals the severity in the listings. When a SSDI beneficiary or SSI disability recipient is found no longer disabled, he or she may appeal the decision using the process described previously.
Age-18 Disability Redeterminations
SSA reevaluates the eligibility of all child SSI recipients who attain the age of 18 under the adult standard for initial disability claims.291 These reevaluations are known as age-18 disability redeterminations. Because these reviews are a new disability determination under the adult criteria, the MIRS does not apply.292
Work CDRs
Under the SSDI program, SSA performs work CDRs to determine if a beneficiary's work activity represents SGA and if eligibility for benefits should continue. SSA typically initiates a work CDR if the agency becomes aware of the beneficiary's return to work. If a work CDR finds evidence that a beneficiary is engaging in SGA and is not participating in an approved SSA work incentive, the agency may find that the beneficiary's disability has ceased.
SSI Redeterminations
Under the SSI program, SSA conducts periodic redeterminations of a recipient's non-medical eligibility factors—such as income, resources, and living arrangements—to verify that a recipient is still eligible for SSI and receiving the correct payment amount.293 There are two types of redeterminations: scheduled and unscheduled. Unscheduled redeterminations are conducted based on a report of a change in a recipient's circumstances that may affect program eligibility or payment amount. Scheduled redeterminations are performed at periodic intervals, depending on the likelihood of payment error: (1) annually if a change in a recipient's circumstances is likely to occur or (2) once every six years if a change in circumstances is unlikely to occur.
Appendix A. Side-by-Side of SSDI and SSI
|
Social Security Disability Insurance (SSDI) |
Supplemental Security Income |
|
|
Type of Program |
Work-related social insurance. |
Need-based public assistance. |
|
Type of Beneficiary |
Disabled individuals under Social Security's full retirement age with significant past work. |
Individuals with limited assets and little or no income who (1) are aged 65 or older or (2) have a qualifying impairment, regardless of age. |
|
Definition of "Disability" |
Inability to engage in substantial gainful activity (SGA) due to any medically determinable physical or mental impairment which has lasted or is expected to last for at least 12 months or to result in death. In 2018, the SGA earnings limit is $1,180 per month for most workers. |
Adults: Same as SSDI. Children: Physical or mental impairment that causes marked and severe functional limitations with daily activities at home, in school, at daycare, or in the community. The impairment must be expected to last for at least 12 months or to result in death. The child's earnings must also be at or below the SGA limit at the time of application. |
|
Work History and Contribution Requirements |
Generally, must have worked and paid Social Security taxes for about 1/4 of adult life and for at least 5 years of the 10 years before the onset of disability. |
None. |
|
Nature of Cash Benefits |
A share of a worker's career-average earnings in jobs covered under Social Security. The share of earnings replaced by SSDI is greater for workers with low lifetime wages than for high-wage workers. The average disabled-worker benefit in 2018 is $1,197 per month. |
Maximum federal payment of $750 per month for an individual in 2018 ($1,125 for a couple). The payment is reduced by "countable income" (generally, half of earnings plus all other income). States may supplement this payment. The average SSI payment in 2018 is $552 per month. |
|
Waiting Period |
5 months. |
None. |
|
Health Coverage |
Entitled to Medicare after 24 months of entitlement to cash benefits (generally 29 months after disability onset). |
Automatically eligible for Medicaid in most states. Some states require a separate Medicaid application. Eight states use more restrictive eligibility criteria than SSI ("209[b] states") |
|
Retroactive Benefits |
Up to 12 months. |
None. |
|
Benefits for Family Members |
Certain spouses and dependent children. |
None. |
|
Means Tested |
No, but earnings must be within the SGA limit for a person to be considered disabled. (The SGA limit is an indirect test of disability.) |
Yes. Must have "countable income" at or below the maximum benefit and no more than $2,000 in "countable assets" for an individual ($3,000 for a couple). Certain income and assets are not counted for eligibility and payment purposes |
|
Financing |
Primarily by payroll taxes credited to the Disability Insurance (DI) trust fund. |
General revenues. |
Source: CRS.
Appendix B. Certain Other Benefits Available to SSDI Beneficiaries and SSI Disability Recipients
Individuals who meet the blindness or disability standards of the SSDI or SSI programs may qualify for certain federal or state benefits. The following section discusses two federal benefits for which SSDI beneficiaries and SSI disability recipients may qualify.
Achieving a Better Life Experience (ABLE) Accounts
The Stephen Beck, Jr., Achieving a Better Life Experience Act (ABLE Act; Division B of P.L. 113-295) authorizes states to establish and maintain tax-advantaged savings plans through which contributions may be made to the investment account of a designated beneficiary to pay for qualified disability expenses.294 Qualified disability expenses include costs related to education, housing, transportation, employment training and support, assistive technology and personal support services, health and wellness (including long-term services and supports), financial management and administrative services, legal fees, expenses for oversight and monitoring, funeral and burial expenses, and other expenses identified in guidance published by the IRS. To qualify for an ABLE account, an individual must either be (1) entitled to Social Security or SSI benefit payments due to blindness or disability and such impairment occurred before the date the individual attained age 26 or (2) certified by a physician that his or her impairment meets the blindness or disability standards used for children under the SSI program, regardless of the individual's age, and such impairment occurred before the date the individual attained age 26.
There are three advantages to ABLE accounts. First, earnings in an ABLE account can grow tax-free annually until they are withdrawn. Second, distributions (i.e., withdrawals) from an ABLE account are tax-free if they are used to pay for qualified disability expenses. Third, assets in and distributions from an ABLE account for qualified disability expenses are disregarded in determining a designated beneficiary's eligibility for and the amount of assistance provided by most federal assistance programs. Under the SSI program, however, only the first $100,000 in an ABLE account is excluded. The balance of an ABLE account above $100,000 is treated as a resource to the designated beneficiary and is counted against the program's resource limit. If a designated beneficiary becomes ineligible for SSI due solely to excess ABLE funds, his or her cash payments are suspended (without a time limit) until the balance of the ABLE account falls to or below $100,000. This suspension does not affect the beneficiary's eligibility for Medicaid. In addition, a distribution from an ABLE account for housing-related expenses is counted against the resource limit unless the distribution is spent in the month of receipt.
ABLE accounts allow SSI disability recipients to save for disability-related expenses without such savings jeopardizing their SSI and Medicaid eligibility. Although ABLE accounts have no effect on an individual's entitlement to SSDI, the accounts may allow beneficiaries to save and establish or maintain their eligibility for other federal programs, such as Medicaid or SNAP. The Social Security Administration (SSA),295 the Centers for Medicare & Medicaid Services (CMS),296 and the Department of Agriculture's Food and Nutrition Service (FNS)297 have all issued guidance on the treatment of ABLE accounts under SSI, Medicaid, and SNAP, respectively.
Total and Permanent Disability (TPD) Discharge of Certain Federal Student Loans
SSDI beneficiaries and SSI disability recipients may have their federal student loans discharged if they meet the requirements of the Department of Education's (ED's) Total and Permanent Disability (TPD) discharge program.298 The TPD discharge applies to obligations incurred under the following federal student loan programs: William D. Ford Federal Direct Loan (Direct Loan) program, the Federal Family Education Loan (FFEL) program, the Federal Perkins Loan program, and the Teacher Education Assistance for College and Higher Education (TEACH) Grant program. Borrowers qualify for the TPD discharge if they are determined to be totally and permanently disabled under any one of the following methods.
- VA Method. The borrower receives Department of Veterans Affairs (VA) disability compensation at the 100% rate due to one or more service-connected disabilities that the VA determined to be (1) totally disabling under its rating schedule, or (2) less than totally disabling under its rating schedule but which prevent the individual from establishing or maintaining substantially gainful employment (known as an individual unemployability [IU] rating).299
- SSA Method. The borrower is entitled to SSDI or SSI and is scheduled to receive a medical review once every five to seven years (i.e., SSA assigns the individual a Medical Improvement Not Expected [MINE] continuing disability review [CDR] diary).300
- Physician's Certification Method. The borrower is certified by a physician that he or she is unable to engage in any substantial gainful activity due to any medically determinable physical or mental impairment that has lasted, or is expected to last, for at least 60 months or is expected to result in death (i.e., the individual meets the definition of disability for adults under the Social Security Act, except that the duration of the impairment must be for at least five years instead of one).
SSDI beneficiaries and SSI disability recipients with a MINE CDR diary may request a Benefits Planning Query (BPQY) statement from SSA to demonstrate to ED that their medical review is scheduled once every five to seven years.301 In July 2017, about 40% of all SSDI beneficiaries and SSI disability recipients had a MINE CDR diary (see Figure 8). SSDI beneficiaries and SSI disability recipients with a medical improvement expected (MIE) or medical improvement possible (MIP) CDR diary may still qualify for the TPD discharge if they are determined to be totally and permanent disabled under the VA method or the physician's certification method.
Borrowers awarded a TPD discharge based on a determination of totally and permanently disabled under the SSA method or the physician's certification method are subject to a three-year monitoring period from the date the discharge is initially granted.302 During the post-discharge monitoring period, the borrower is required to have annual earnings at or below the Department of Health and Human Services' (HHS's) poverty guideline for a family of two, regardless of his or her actual family size. ED will reinstate the loan obligation if the borrower fails to meet any of the TPD discharge program's requirements during the post-discharge monitoring period. The post-discharge monitoring period does not apply to borrowers awarded a TPD discharge based on a determination of totally and permanently disabled under the VA method. For more information on the TPD discharge program, including the monitoring period, visit http://www.disabilitydischarge.com.
Computer Matching Agreements between ED and Other Federal Agencies to Improve the TPD Discharge Process
Some disability advocates and Members of Congress have expressed concern that the TPD discharge process is "cumbersome," in that it requires borrowers to independently determine whether they qualify for the discharge and to coordinate the sharing of information between federal agencies to verify that they meet the applicable requirements.303 To address such concerns, President Barack Obama issued a memorandum in March 2015 that directed the Secretary of Education and the Director of the Office of Management and Budget (OMB), in consultation with the Commissioner of Social Security, to develop a plan to proactively identity student loan borrowers who receive SSDI and determine if they qualify for the TPD discharge.304 Later that year, ED released a report that, among other things, advocated for the streamlining of the TPD discharge process by having federal agencies coordinate their efforts to notify borrowers automatically of their potential eligibility for the discharge.305
In April 2016, ED announced that it had conducted a data match with SSA to identify borrowers potentially eligible for the TPD discharge under the SSA method. The match identified 387,000 SSDI beneficiaries and SSI disability recipients with a combined loan balance of over $7.7 billion.306 Shortly thereafter, borrowers who were positively identified in the match received a customized letter from ED's TPD servicer, Nelnet, explaining their eligibility for the discharge and how to apply for it. The number of individuals identified in the data match represented about 3% of the total SSDI beneficiary and SSI disability recipient population in July 2016, and about 7% of the total population with a MINE CDR diary that month. According to the Government Accountability Office (GAO), as of July 31, 2016, "TPD discharge applications were sent to about 234,000 borrowers based on the data matching and slightly more than 19,000 applications had been submitted and approved."307
In April 2018, ED announced that it would conduct a similar data match with the VA to identify borrowers potentially eligible for the TPD discharge under the VA method.308
Recent Changes to the Federal Income Tax Treatment of Loans Discharged Under the TPD Discharge Program
Under prior law, the amount of student loan debt discharged under the TPD discharge program was included in the borrower's gross income for purposes of federal income tax in the year the discharge became final, which for borrowers approved under the SSA method or physician's certification method is at the close of the three-year monitoring period and for borrowers approved under the VA method is the date that ED approves the discharge. This resulted in some borrowers having markedly high taxable income relative to their income exclusive of the discharged student loan indebtedness for the tax year. However, during debate on the 2017 tax revision (P.L. 115-97), the Senate incorporated some of the provisions of the Stop Taxing Death and Disability Act (S. 405) into the legislation, which were ultimately enacted into law.309 Section 11031 of P.L. 115-97 excludes the amount of the discharged indebtedness under the TPD discharge from the definition of gross income for federal income tax purposes.310 These new provisions apply to loans discharged during the period from January 1, 2018, through December 31, 2025. Student loan debt discharged under the TPD discharge program may still be considered income for state income tax purposes.
Author Contact Information
Acknowledgments
CRS Research Assistant Jameson A. Carter updated much of the data in this report. CRS Graphics Specialist Amber Wilhelm produced the figures shown in the report.
Footnotes
| 1. |
See 2 U.S.C. §622 for the definition of entitlement authority. |
| 2. |
Estimates calculated by the Congressional Research Service (CRS) based on a variety of data sources available on the Social Security Administration's (SSA) website. For purposes of these estimates, the term Social Security Disability Insurance (SSDI) includes Social Security disability beneficiaries whose benefits are paid from the Old-Age and Survivors Insurance (OASI) trust fund. In addition, the term qualified disabled individuals excludes SSI-only recipients aged 65 or older. Congressional clients may contact the author for the specific methodology used in the calculations. |
| 3. |
42 U.S.C. §§401 et seq. See CRS Report R42035, Social Security Primer. |
| 4. |
SSA, Office of Legislation and Congressional Affairs (OLCA), 2018 Social Security/SSI/Medicare Information, February 15, 2018, https://www.ssa.gov/legislation/2018%20Fact%20Sheet.pdf. |
| 5. |
SSA, Office of the Chief Actuary (OCACT), "Benefits Paid by Type of Beneficiary," https://www.ssa.gov/oact/ProgData/icp.html. |
| 6. |
Ibid. |
| 7. |
Section 223(a) of the Social Security Act; 42 U.S.C. §423(a). |
| 8. |
SSA, OCACT, "Quarter of Coverage," https://www.ssa.gov/oact/cola/QC.html. |
| 9. |
SSA, OCACT, "National Average Wage Index," https://www.ssa.gov/oact/cola/AWI.html. |
| 10. |
Section 214(a) of the Social Security Act; 42 U.S.C. §414(a). See also 20 C.F.R. §404.110. |
| 11. |
Section 223(c)(1) of the Social Security Act; 42 U.S.C. §423(c)(1). See also 20 C.F.R. §404.130. |
| 12. |
Workers aged 24-30 need quarters of coverage (QCs) in at least one-half of the quarters in the period beginning with the quarter after the quarter they attained the age of 21 and ending in the quarter in which their disability began. Workers under 24 years old need at least six QCs in the 12-quarter period ending with the quarter in which they became disabled. Blind workers are exempt from the recency-of-work requirement. Special rules apply to individuals who become disabled again at age 31 or older after having had a prior period of disability established which began before age 31. See SSA, How You Earn Credits, January 2018, https://www.ssa.gov/pubs/EN-05-10072.pdf. |
| 13. |
SSA, OCACT, "Disability Insured Workers," https://www.ssa.gov/OACT/STATS/table4c2DI.html, See also SSA, OCACT, "Social Security Program Fact Sheet," March 1, 2018, https://www.ssa.gov/oact/FACTS/. |
| 14. |
Section 216(l) of the Social Security Act; 42 U.S.C. §416(l). |
| 15. |
Section 202(b) and 202(c) of the Social Security Act; 42 U.S.C. §402(b) and 402(c). See also 20 C.F.R. §404.330. |
| 16. |
Section 216(b)(2) and 216(f)(2) of the Social Security Act; 42 U.S.C. §416(b)(2) and 416(f)(2). See also 20 C.F.R. §404.330(a)(1). To determine the validity of the marriage, SSA looks to the laws of the state (as interpreted by the courts of that state) in which the insured worker is domiciled at the time of application. Alternatively, the relationship requirement is met if, under state intestate law, the applicant would be able to inherit a wife's or husband's share of the insured worker's personal property if the insured worker were to die without leaving a will. |
| 17. |
Section 202(b) and 202(c) of the Social Security Act; 42 U.S.C. §402(b) and 402(c). See also 20 C.F.R. §404.331. |
| 18. |
Section 216(d) of the Social Security Act; 42 U.S.C. §416 (d). See also 20 C.F.R. §404.331. |
| 19. |
Section 202(d)(1)(B)(i) of the Social Security Act; 42 U.S.C. §402(d)(1)(B)(i). See also 20 C.F.R. §404.350. |
| 20. |
Section 216(e) and 216(h) of the Social Security Act; 42 U.S.C. §416(e) and 416(h). See also 20 C.F.R. §§404.354-404.359. In determining a child's relationship to an insured worker, SSA looks to the laws of the state (as interpreted by the courts of that state) in which the parent is domiciled at the time of application. A child may qualify as an insured worker's child for purposes of entitlement to child's insurance benefits if he or she would inherit the parent's personal property under state intestate law. |
| 21. |
20 C.F.R. §§404.360-404.366. |
| 22. |
SSA, Program Operations Manual System (POMS), "GN 00306.001 Determining Status as Child," August 30, 2016, https://secure.ssa.gov/poms.nsf/lnx/0200306001. |
| 23. |
Section 202(d)(1)(B)(i) of the Social Security Act; 42 U.S.C. §402(d)(1)(B)(i). See also 20 C.F.R. §404.350. |
| 24. |
20 C.F.R. §404.367. |
| 25. |
Section 202(d)(1)(B)(ii) of the Social Security Act; 42 U.S.C. §402(d) (1)(B)(ii). See also 20 C.F.R. §404.350. |
| 26. |
Section 202(d)(5) of the Social Security Act; 42 U.S.C. §402(d)(5). See also 20 C.F.R. §404.352(b)(4). |
| 27. |
Section 202(e) and 202(f) of the Social Security Act; 42 U.S.C. §402(e) and 402(f). See also 20 C.F.R. §§404.335-404.336. |
| 28. |
Section 216(k) of the Social Security Act; 42 U.S.C. §416(k). See also 20 C.F.R. §404.335(a). |
| 29. |
Section 216(d)(2) and 216(d)(5) of the Social Security Act; 42 U.S.C. §416(d)(2) and 416(d)(5). See also 20 C.F.R. §404.336(a)(2). |
| 30. |
Section 202(d)(1)(B)(ii) of the Social Security Act; 42 U.S.C. §402(d) (1)(B)(ii). See also 20 C.F.R. §404.350. |
| 31. |
SSA, Office of Research, Evaluation, and Statistics (ORES), Annual Statistical Supplement, 2017, March 2018, Table 5.A1.4, https://www.ssa.gov/policy/docs/statcomps/supplement/ (hereinafter "2017 Annual Statistical Supplement"). |
| 32. |
For termination data on SSDI dependents and OASI disability beneficiaries, SSA, ORES, Annual Statistical Report on the Social Security Disability Insurance Program, 2016, October 2017, Table 50, https://www.ssa.gov/policy/docs/statcomps/di_asr/2015/index.html (hereinafter "2016 SSDI Annual Report"). |
| 33. |
CRS Report R43542, How Social Security Benefits Are Computed: In Brief. Earnings in years after the indexing year are counted at their actual value. |
| 34. |
Up to five of the worker's lowest-earning years are dropped from the computation. |
| 35. |
SSA, OCACT, "Benefit Formula Bend Points," https://www.ssa.gov/oact/cola/bendpoints.html. |
| 36. |
CRS Report 94-803, Social Security: Cost-of-Living Adjustments. Pursuant to the Department of the Treasury's 2010 rule (75 Federal Register 80315), all federal benefit payments must be made via electronic funds transfer (ETF), unless the individual can demonstrate hardship due to age, mental impairment, or geographic location. Social Security beneficiaries receive their payments by direct deposit, either to a bank account or to a Direct Express® card account. |
| 37. |
Section 203(a)(6) of the Social Security Act; 42 U.S.C. §403(a)(6). See also 20 C.F.R. §404.403d-1. |
| 38. |
2016 SSDI Annual Report, Table 30. |
| 39. |
Section 203(a)(1) of the Social Security Act; 42 U.S.C. §403(a)(1). See also 20 C.F.R. §404.403(d) and SSA, OCACT, "Formula for Family Maximum Benefit," https://www.ssa.gov/oact/cola/familymax.html. |
| 40. |
CRS Report R44580, Workers' Compensation: Overview and Issues. |
| 41. |
Section 224 of the Social Security Act; 42 U.S.C. §424a. See also 20 C.F.R. §404.408 and SSA, How Workers' Compensation and Other Disability Payments May Affect Your Benefits, https://www.ssa.gov/pubs/EN-05-10018.pdf. |
| 42. |
Section 224(a)(2)(B) of the Social Security Act; 42 U.S.C. §424a(A)(2)(B). See also 20 C.F.R. §404.408(b). |
| 43. |
Section 201 of the Stephen Beck, Jr., Achieving a Better Life Experience Act of 2014 (ABLE Act; Division B of P.L. 113-295) increased the age at which the offset no longer applies from 65 years old to full retirement age (FRA). |
| 44. |
SSA, POMS, "DI 52105.001 Reverse Offset Plans," February 12, 2018, http://policy.ssa.gov/poms.nsf/lnx/0452105001. The reverse offset also applies to railroad sickness pensions administered by the Railroad Retirement Board (RRB). |
| 45. |
2016 SSDI Annual Report, Tables 1 and 31. |
| 46. |
SSA, OCACT, "Benefits Paid by Type of Beneficiary," https://www.ssa.gov/oact/ProgData/icp.html. |
| 47. |
Section 223(a)(1) and 223(c)(2) of the Social Security Act; 42 U.S.C. §423(a)(1) and 423(c)(2). |
| 48. |
Section 202(e)(1)(F)(i), 202(e)(5)(A), 202(f)(1)(F)(i), and 202(f)(5)(A) of the Social Security Act; 42 U.S.C. §402(e)(1)(F)(i), 402(e)(5)(A), 402(f)(1)(F)(i), and 402(f)(5)(A). |
| 49. |
See 20 C.F.R. §404.1807 and SSA, "Schedule of Social Security Payments," https://www.ssa.gov/pubs/calendar.htm. |
| 50. |
There is no statutory exception to the five-month waiting period for disabled adult children. Section 202(d) of the Social Security Act (42 U.S.C. §402[d]) simply does not require claimants to serve a waiting period to be entitled to child's insurance benefits due to a disability. In the case of disabled adult child of a disabled worker, the disabled adult child's benefits start only after the disabled worker has satisfied the five-month waiting period requirement and is entitled to disabled-worker benefits. |
| 51. |
Section 223(a)(1) of the Social Security Act; 42 U.S.C. §423(a)(1). See also 20 C.F.R. §404.315(a)(4). |
| 52. |
Sections 202(e)(4)(C), 202(e)(5)(A)(ii)(II), 202(f)(4)(C), and 202(f)(5)(A)(ii)(II) of the Social Security Act; 42 U.S.C. §§402(e)(4)(C), 402(e)(5)(A)(ii)(II), 402(f)(4)(C), and 402(f)(5)(A)(ii)(II). See also 20 C.F.R. §§404.335(c)(2) and 404.336(c)(2). |
| 53. |
Section 202(e)(5)(B) and 202(f)(5)(B) of the Social Security Act; 42 U.S.C. §402(e)(5)(B) and 402(f)(5)(B). See also 20 C.F.R. §§404.335(c)(3) and 404.336(c)(3). |
| 54. |
Sections 202(e)(5)(A), 202(f)(5)(A), and 223(c)(2) of the Social Security Act; 42 U.S.C. §§402(e)(5)(A), 402(f)(5)(A), and 423(c)(2). See also 20 C.F.R. §§404.315(a)(4), 404.335(c)(2), and 404.336(c)(2). |
| 55. |
See SSA, "Medicare Information," https://www.ssa.gov/disabilityresearch/wi/medicare.htm. |
| 56. |
42 U.S.C. §§1395 et seq. For more information on Medicare, see CRS Report R40425, Medicare Primer. |
| 57. |
Medicare Payment Advisory Commission (MEDPAC), A Data Book: Health Care Spending and the Medicare Program, June 2017, p. 21, http://www.medpac.gov/docs/default-source/data-book/jun17_databookentirereport_sec.pdf. Estimate excludes spending on individuals under 65 years old who are entitled to Medicare on the basis of end-stage renal disease (ESRD). |
| 58. |
Section 226(b)(2)(A) of the Social Security Act; 42 U.S.C. §426(b)(2)(A). See also 42 C.F.R. §406.12. |
| 59. |
CRS analysis of the 2017 Current Population Survey Annual Social and Economic Supplement (CPS ASEC). |
| 60. |
Section 226(f) of the Social Security Act; 42 U.S.C. §426(f). See also 42 C.F.R. §406.12(b)(1) and 406.12(b)(2). |
| 61. |
Section 226(f) of the Social Security Act; 42 U.S.C. §426(f). See also 42 C.F.R. § 406.12(b)(3). |
| 62. |
Section 226(e)(1)(B) of the Social Security Act; 42 U.S.C. §426(e)(1)(B). |
| 63. |
Based on information provided to CRS by SSA on August 10, 2017. |
| 64. |
Section 226(h) of the Social Security Act; 42 U.S.C. §426(h). |
| 65. |
Section 226A of the Social Security Act; 42 U.S.C. § 426-1. ESRD is a stage of kidney impairment that appears to be irreversible and permanent, requiring a regular course of dialysis treatments or a kidney transplantation to maintain life. |
| 66. |
Section 1881A of the Social Security Act; 42 U.S.C. §1395rr-1. See SSA, "Libby," https://www.ssa.gov/libby/. |
| 67. |
42 U.S.C. §426-1(b) and 42 C.F.R. §406.13(e). |
| 68. |
26 U.S.C. §§3101, 3111, 1401, respectively. |
| 69. |
SSA, OCACT, "Contribution and Benefit Base," https://www.ssa.gov/oact/cola/cbb.html. |
| 70. |
Section 201(a) and 201(b) of the Social Security Act; 42 U.S.C. §401(a) and 401(b). The allocation of the tax rate between the OASI and Disability Insurance (DI) trust funds is scheduled to change in 2019. See SSA, OCACT, "Social Security Taxes Rates," https://www.ssa.gov/oact/progdata/oasdiRates.html. |
| 71. |
Section 121(e) of the Social Security Amendments of 1983 (P.L. 98-21); 42 U.S.C. §401 note. |
| 72. |
Section 201(f) of the Social Security Act; 42 U.S.C. §401(f). |
| 73. |
U.S. Congress, House Committee on Ways and Means, The 2017 Annual Report of the Board of Trustees of the Federal Old-Age and Survivors Insurance and Federal Disability Insurance Trust Funds, 115th Cong., 1st sess., July 18, 2016, H.Doc. 115-54 (Washington: GPO, 2017), p. 3, https://www.ssa.gov/oact/tr/2017/index.html. |
| 74. |
See CBO, Old-Age, Survivors, and Disability Insurance Trust Funds—CBO's June 2017 Baseline, June 2017, https://www.cbo.gov/sites/default/files/recurringdata/51309-2017-06-trustfund.pdf. |
| 75. |
CBO, The Budget and Economic Outlook: 2018 to 2028, April 9, 2018, p. 134, https://www.cbo.gov/publication/53651. Newer projections for the OASI and hypothetical combined trust funds have not been released by CBO as of the date of this report. |
| 76. |
42 U.S.C. §§1381 et seq. |
| 77. |
SSA, ORES, "SSI Monthly Statistics, 2017," January 2018, Table 2, https://www.ssa.gov/policy/docs/statcomps/ssi_monthly/2017/index.html. |
| 78. |
20 C.F.R. §416.202. |
| 79. |
Section 1602 of the Social Security Act; 42 U.S.C. §1381a. |
| 80. |
Section 1614(a)(1) of the Social Security Act; 42 U.S.C. §1382c(a)(1). See also 20 C.F.R. §416.202(a)(1). |
| 81. |
Section 1614(a)(2) of the Social Security Act; 42 U.S.C. §1382c(a)(2). See also 20 C.F.R. §§416.202(a)(2) and 416.981. |
| 82. |
20 C.F.R. §416.1102. |
| 83. |
20 C.F.R. §416.1201(a). |
| 84. |
Section 1611(a)(1)(A), 1611(a)(2)(A), and 1611(b) of the Social Security Act; 42 U.S.C. §1382(a)(1)(A), §1382(a)(2)(A), and §1382(b). |
| 85. |
SSA, OCACT, "SSI Federal Payment Amounts," https://www.ssa.gov/oact/cola/SSIamts.html. |
| 86. |
Section 1617 of the Social Security Act; 42 U.S.C. §1382f. See also 20 C.F.R. §416.405. |
| 87. |
SSA, POMS, "SI 02301.215 Summary of Posteligibility (PE) Suspension, Stop Payment and Termination Events by Payment Status Code (PSC)," February 18, 2016, http://policy.ssa.gov/poms.nsf/lnx/0502301215. |
| 88. |
Section 1612(a)(1) of the Social Security Act; 42 U.S.C. §1382a(a)(1). See also 20 C.F.R. §416.1110. |
| 89. |
CRS Report RL33362, Unemployment Insurance: Programs and Benefits. |
| 90. |
CRS Report RS22350, Railroad Retirement Board: Retirement, Survivor, Disability, Unemployment, and Sickness Benefits. |
| 91. |
CRS In Focus IF10036, The Temporary Assistance for Needy Families (TANF) Block Grant. |
| 92. |
Section 1612(a)(2) of the Social Security Act; 42 U.S.C. §1382a(a)(2). See also 20 C.F.R. §416.1120. |
| 93. |
Section 1612(b) of the Social Security Act; 42 U.S.C. §1382a(b). See also 20 C.F.R. §§416.1112, 416.1124, and the Appendix to Subpart K. |
| 94. |
Section 1612(b)(2)(A) of the Social Security Act; 42 U.S.C. §1382a(b)(2)(A). See also 20 C.F.R. §§416.1112(c)(4) and 416.1124(c)(12). |
| 95. |
Section 1612(b)(4)(A)(i), 1612(b)(4)(B)(i), 1612(b)(4)(B)(iii), and 1612(b)(4)(C) of the Social Security Act; 42 U.S.C. §1382a(b)(4)(A)(i), 1382a(b)(4)(B)(i), 1382a(b)(4)(B)(iii), and1382a(b)(4)(C). See also 20 C.F.R. §416.1112(c)(5) and 416.1112(c)(7). |
| 96. |
Section 1612(b)(3)(B) of the Social Security Act; 42 U.S.C. §1382a(b)(3)(B). See also 20 C.F.R. §416.1112(c)(5). |
| 97. |
Section 1612(b)(3)(A) of the Social Security Act; 42 U.S.C. §1382a(b)(3)(A). See also 20 C.F.R. §416.1124(c)(6). |
| 98. |
7 U.S.C. §2017(b) and 42 U.S.C. 1780(b). See also CRS Report R42505, Supplemental Nutrition Assistance Program (SNAP): A Primer on Eligibility and Benefits, and CRS Report R44115, A Primer on WIC: The Special Supplemental Nutrition Program for Women, Infants, and Children. |
| 99. |
Section 1612(b)(13) of the Social Security Act; 42 U.S.C. §1382a(b)(13). See also 42 U.S.C. §8624(f) and 20 C.F.R. §§416.1124(c)(2) and 416.1157. Moreover, see CRS Report RL31865, LIHEAP: Program and Funding. |
| 100. |
Section 1612(b)(14) of the Social Security Act; 42 U.S.C. §1382a(b)(14). See also 20 C.F.R. §416.1124(c)(14) and 42 U.S.C. §1382 note. Moreover, see CRS Report RL34591, Overview of Federal Housing Assistance Programs and Policy. |
| 101. |
26 U.S.C. §§24 note and 6409. See also 20 C.F.R. §§416.1103(d). Moreover, see CRS Report R43805, The Earned Income Tax Credit (EITC): An Overview, and CRS Report R41873, The Child Tax Credit: Current Law. |
| 102. |
Section 1612(b)(13) of the Social Security Act; 42 U.S.C. §1382a(b)(13). See also 20 C.F.R. §416.1124(c)(2). |
| 103. |
Section 1612(b)(26) of the Social Security Act; 42 U.S.C. §1382a(b)(26). |
| 104. |
Section 1612(b)(4)(A)(ii) and 1612(b)(4)(B)(ii) of the Social Security Act; 42 U.S.C. §1382a(b)(4)(A)(ii) and 1382a(b)(4)(B)(ii). See also 20 C.F.R. §416.1112(c)(6) and 416.1112(c)(8). |
| 105. |
Section 1612(b)(4)(A)(iii) and 1612(b)(4)(B)(iv) of the Social Security Act; 42 U.S.C. §1382a(b)(4)(A)(iii) and 1382a(b)(4)(B)(iv). See also 20 C.F.R. §§416.1112(c)(9) and 416.1124(c)(13). |
| 106. |
SSA, POMS, "SI 00830.099 Guide to Unearned Income Exclusions," April 23, 2013, https://secure.ssa.gov/apps10/poms.nsf/lnx/0500830099. |
| 107. |
SSA no longer includes clothing in the definition of in-kind support and maintenance (ISM). |
| 108. |
20 C.F.R. §416.1130(b). |
| 109. |
Section 1612(a)(2)(A) of the Social Security Act; 42 U.S.C. §1382a(a)(2)(A). See also 20 C.F.R. §416.1131. |
| 110. |
SSA, POMS, "SI 00835.901 Values for In-Kind Support and Maintenance for 2006 and Later," January 24, 2018, http://policy.ssa.gov/poms.nsf/lnx/0500835901. |
| 111. |
20 C.F.R. §416.1140. |
| 112. |
See CRS Report RL34591, Overview of Federal Housing Assistance Programs and Policy. |
| 113. |
Ken Brown, In-kind Support & Maintenance in the Supplemental Security Income Program, July 12, 2016, slide 4, http://www.ssab.gov/Portals/0/2016%20SSI%20Forum/Presentations/Ken%20Brown%20-%20ISM%20Presentation.pdf?ver=2016-07-09-131547-763. |
| 114. |
Section 1611(a)(3) of the Social Security Act; 42 U.S.C. §1382(a)(3). See also 20 C.F.R. §416.1205. |
| 115. |
Under certain circumstances, individuals who have excess countable resources but who meet all other eligibility requirements may receive SSI benefits for a limited period, provided they dispose of their excess resources at current market value (CMV). See Section 1613(b) of the Social Security Act; 42 U.S.C. §1382b(b). See also 20 C.F.R. §§416.1240-416.1245. |
| 116. |
Section 1613(c) of the Social Security Act; 42 U.S.C. §1382b(c). |
| 117. |
Section 1613(e) of the Social Security Act; 42 U.S.C. §1382b(e). |
| 118. |
Section 1613(a) of the Social Security Act; 42 U.S.C. §1382b(a). See also 20 C.F.R. §§416.1210-416.1266. Not all resource exclusions are specified in Title XVI or in SSA regulations. |
| 119. |
Section 1613(a)(1) of the Social Security Act; 42 U.S.C. §1382b(a)(1). See also 20 C.F.R. §§416.1210(a) and 416.1212. |
| 120. |
Section 1613(a)(2)(A) of the Social Security Act; 42 U.S.C. §1382b(a)(2)(A). See also 20 C.F.R. §§416.1210(b) and 416.1216. |
| 121. |
Section 1613(a)(2)(A) of the Social Security Act; 42 U.S.C. §1382b(a)(2)(A). See also 20 C.F.R. §§416.1210(c) and 416.1218. |
| 122. |
Section 1613(a)(3) of the Social Security Act; 42 U.S.C. §1382b(a)(3). See also 20 C.F.R. §§416.1210(e) and 416.1224. |
| 123. |
SSA, POMS, "SI 01120.230 Health Flexible Spending Arrangements (FSAs)," November 13, 2013, https://secure.ssa.gov/poms.nsf/lnx/0501120230. |
| 124. |
Section 1613(a)(4) of the Social Security Act; 42 U.S.C. §1382b(a)(4). See also 20 C.F.R. §§416.1210(f) and 416.1226. |
| 125. |
26 U.S.C. §§24 note and 6409. See also 20 C.F.R. §§416.1210(o) and 416.1235. Moreover, see SSA, POMS, "SI 01130.676 Federal Tax Refunds and Advanced Tax Credits for SSI Resources," August 11, 2014, https://secure.ssa.gov/poms.nsf/lnx/0501130676. |
| 126. |
Section 1613(a)(16) of the Social Security Act; 42 U.S.C. §1382b(a)(16). See also 20 C.F.R. §§416.1210(h) and 416.1230 |
| 127. |
Section 1613(d) of the Social Security Act; 42 U.S.C. §1382b(d). See also 20 C.F.R. §§416.1210(l) and 416.1231. |
| 128. |
Sections 1613(c)(1)(C)(ii), 1613(e)(5), 1917(d)(4)(A), and 1917(d)(4)(C) of the Social Security Act; 42 U.S.C. §§1382b(c)(1)(C)(ii), 1382b(e)(5), 1396p(d)(4)(A), and 1396p(d)(4)(C). |
| 129. |
26 U.S.C. §529A note. CRS In Focus IF10363, Achieving a Better Life Experience (ABLE) Programs. |
| 130. |
SSA, POMS, "SI 01130.050 Guide to Resources Exclusions," August 16, 2017, https://secure.ssa.gov/apps10/poms.nsf/lnx/0501130050. |
| 131. |
Section 1614(f) of the Social Security Act; 42 U.S.C. §1382c(f). See also 20 C.F.R. §§416.1160-416.1169 and 416.1202-416.1204a. |
| 132. |
The allocation for an ineligible spouse is the difference between the federal benefit rate (FBR) for a couple and the FBR for an individual (20 C.F.R. §416.1163[d]). (Although SSA effectively deducts an allocation equal to this amount from the ineligible spouse's income, the agency does not call it an allocation because the calculation process used for ineligible spouses is different from the process used for other ineligible family members.) The allocation for each ineligible child is the difference between the FBR for a couple and the FBR for an individual (20 C.F.R. §§416.1163[b][1] and 416.1165[b]). In the case of an eligible child, the parental allocation is equal to the FBR for an individual for one ineligible parent or the FBR for a couple for two ineligible parents (20 C.F.R. §416.1165[d][3]). |
| 133. |
The countable resource limit for an eligible individual with an ineligible spouse is the amount applicable to an eligible couple. The countable resource limit for an ineligible child is equal to his or her own $2,000 limit plus the amount applicable to an eligible individual in the case of one ineligible parent or the amount application to an eligible couple in the case of two ineligible parents (20 C.F.R. §416.1202[b]). The countable resource limit for an alien subject to deeming is the amount applicable to an eligible individual in the case of a sponsor without a spouse or the amount applicable to an eligible couple in the case of a sponsor who lives with a spouse (20 C.F.R. §416.1204[a]). |
| 134. |
Virginia Commonwealth University (VCU) National Training and Data Center (NTDC), "Understanding the Supplemental Security Income (SSI) Program," https://vcu-ntdc.org/resources/resourceDetail.cfm?id=1. |
| 135. |
Section 1614(a)(1)(B)(i) and 1614(e) of the Social Security Act; 42 U.S.C. §1382c(a)(1)(B)(i) and 1382c(e). See also 20 C.F.R. §§416.202(b) and 416.1603(c). Although 1614(e) of the Social Security Act specifies that the term "United States" includes only the 50 states and the District of Columbia, the Northern Mariana Islands territorial covenant specifies that "[t]he following laws of the United States in existence on the effective date of this Section and subsequent amendments to such laws will apply to the Northern Mariana Islands ... Title XVI of the Social Security Act as it applies to the several States." See Section 503(a) of P.L. 94-241; 48 U.S.C. §1801 note. |
| 136. |
42 U.S.C. §§301-306, 1201-1206, and 1351-1355, respectively. |
| 137. |
42 U.S.C. §§1381 note-1385 note. |
| 138. |
Section 1611(f) of the Social Security Act; 42 U.S.C. §1382(f). See also 20 C.F.R. §§416.215 and 416.1327. |
| 139. |
Sections 1611(f)(1) and 1614(a)(1)(B)(ii) of the Social Security Act; 42 U.S.C. §§1382(f)(1) and 1382c(a)(1)(B)(ii). See also 20 C.F.R. §416.216. |
| 140. |
Section 1611(f)(2) of the Social Security Act; 42 U.S.C. §1382(f)(2). See also SSA, POMS, "SI 00501.411 SSI Eligibility for Students Temporarily Abroad—Overview," September 13, 2012, https://secure.ssa.gov/poms.nsf/lnx/0500501411. |
| 141. |
Section 1614(a)(1)(B)(i) of the Social Security Act; 42 U.S.C. §1382c(a)(1)(B)(i). See also 20 C.F.R. §416.202(b) and 416.1610-416.1619. |
| 142. |
For a discussion of qualified and non-qualified aliens, see Appendix C of CRS Report RL33809, Noncitizen Eligibility for Federal Public Assistance: Policy Overview. |
| 143. |
Title V of the Illegal Immigration Reform and Immigrant Responsibility Act of 1996 (Division C of the Omnibus Consolidated Appropriations Act, 1997 [P.L. 104-208]), Title V of the Balanced Budget Act of 1997 (P.L. 105-33), and the Noncitizen Benefit Clarification and Other Technical Amendments Act of 1998 (P.L. 105-306). |
| 144. |
CRS Report RL33809, Noncitizen Eligibility for Federal Public Assistance: Policy Overview. |
| 145. |
CRS Report R45020, A Primer on U.S. Immigration Policy. |
| 146. |
8 U.S.C. §§1612(a)(2), 1613, and 1641(b). |
| 147. |
CRS Report R44714, U.S. Policy on Cuban Migrants: In Brief. |
| 148. |
CRS Report R43725, Iraqi and Afghan Special Immigrant Visa Programs. |
| 149. |
8 U.S.C. §§1612(a)(2), 1613, and 1641(b). |
| 150. |
SSA, ORES, SSI Annual Statistical Report, 2016, Table 29, https://www.ssa.gov/policy/docs/statcomps/ssi_asr/ (hereinafter "2016 SSI Annual Statistical Report"). |
| 151. |
SSA, OCACT, Annual Report of the Supplemental Security Income Program, 2017, September 1, 2017, p. 21, https://www.ssa.gov/oact/ssir/SSI17/ssi2017.pdf (hereinafter "2017 Annual Report of the SSI Program"). |
| 152. |
2016 SSI Annual Statistical Report, Table 6. |
| 153. |
Ibid., Tables 30 and 33. |
| 154. |
Section 1611(e)(1)(A) of the Social Security Act; 42 U.S.C. §1382(e)(1)(A). See also 20 C.F.R. §416.211. |
| 155. |
Section 1611(e)(1)(C) of the Social Security Act; 42 U.S.C. §1382(e)(1)(C). See also 20 C.F.R. §416.211(c). |
| 156. |
Section 1611(e)(1)(B) of the Social Security Act; 42 U.S.C. §1382(e)(1)(B). See also 20 C.F.R. §§416.212 and 416.414. |
| 157. |
Section 1611(e)(2) of the Social Security Act; 42 U.S.C. §1382(e)(2). See also 20 C.F.R. §416.210. |
| 158. |
Section 1611(e)(4)(A) of the Social Security Act; 42 U.S.C. §1382(e)(4)(A). See also 20 C.F.R. §§416.202(f) and 416.1339. |
| 159. |
Section 1631(e)(1)(B)(ii) of the Social Security Act; 42 U.S.C. §1383(e)(1)(B)(ii). See also 20 C.F.R. §416.207. |
| 160. |
Section 1631(j)(1) of the Social Security Act; 42 U.S.C. §1383(j)(1). Blind or disabled children of military personnel stationed overseas and military-related individuals who become ineligible for SSI because their spouse or parent(s) is called to active duty have 24-consecutive months after the suspension to have eligibility reinstated without having to file a new application. See 20 C.F.R. §416.216. |
| 161. |
Section 1611(b) of the Social Security Act; 42 U.S.C. §1382(b). See also 20 C.F.R. §§416.410-416.415. |
| 162. |
Pursuant to the Department of the Treasury's 2010 rule (75 Federal Register 80315), all federal benefit payments must be made via EFT, unless the individual can demonstrate hardship due to age, mental impairment, or geographic location. SSI recipients receive their payments by direct deposit, either to a bank account or to a Direct Express® card account. |
| 163. |
The term federal poverty level (FPL) used in this report refers to the Department of Health and Human Services' (HHS) 2018 federal poverty guidelines for the 48 contiguous states and the District of Columbia. See HHS, Office of the Assistant Secretary for Planning and Evaluation (ASPE), "Poverty Guidelines," https://aspe.hhs.gov/poverty-guidelines. See also 42 U.S.C. §9902(2). |
| 164. |
Section 1617 of the Social Security Act; 42 U.S.C. §1382f. See also 20 C.F.R. §416.405. |
| 165. |
SSA, OCACT, "SSI Federal Payment Amounts," https://www.ssa.gov/oact/cola/SSIamts.html. |
| 166. |
Section 1616(a) of the Social Security Act; 42 U.S.C. §1382e(a). See also 20 C.F.R. §§416.2001-416.2075. |
| 167. |
2017 Annual Report of the SSI Program, Table III.H1, p. 25. The 2017 Annual Report of the SSI program states "[c]urrently, 44 States and the District of Columbia have optional State supplementation programs" (p. 21). Although Table III.H1 counts 44 states (including Kansas) and D.C. as having optional state supplementation programs, a footnote to Kansas states "[m]andatory minimum State supplementation program is federally administered. No optional program." Based on the documentation in the footnotes to Table III.H1, the following areas do not operate optional state supplementation programs: Arizona, Arkansas, Kansas, Mississippi, North Dakota, the Northern Mariana Islands, Tennessee, and West Virginia. |
| 168. |
Section 212(a) of P.L. 93-66. See also 20 C.F.R. §§416.2050-416.2075. Texas never operated a mandatory minimum supplementation program because it has a state constitutional barrier against such a requirement. The Commonwealth of the Northern Mariana Islands was not required to operate a mandatory minimum supplementation program because the former federal-state programs of cash assistance for the aged, blind, and disabled were never available in the territory. In addition, SSI was not extended to the Northern Mariana Islands until 1978. |
| 169. |
North Dakota and West Virginia are required to operate mandatory minimum supplementation programs; however, they currently have no recipients. |
| 170. |
Section 1616(b) of the Social Security Act; 42 U.S.C. §1382e(b). See also 20 C.F.R. §416.2005. |
| 171. |
Section 1616(d) of the Social Security Act; 42 U.S.C. §1382e(d). See also 20 C.F.R. §416.2010. |
| 172. |
The user fee per state supplementary payment (SSP) for FY2018 is $11.87. See SSA, OCACT, "Fee for Administration of State Supplementary Payments," https://www.ssa.gov/oact/cola/statesuppfee.html. |
| 173. |
See SSA, A Guide to Supplemental Security Income (SSI) for Groups and Organizations, January 2018, Publication No. 05-11015, p. 5, https://www.ssa.gov/pubs/EN-05-11015.pdf. |
| 174. |
SSA, ORES "SSI Monthly Statistics, 2017," https://www.ssa.gov/policy/docs/statcomps/ssi_monthly/2017/index.html; and SSA, ORES, Congressional Statistics, 2017, April 2018, Table 2 for California, https://www.ssa.gov/policy/docs/factsheets/cong_stats/index.html (hereinafter "2017 Congressional Statistics"). |
| 175. |
SSA, ORES, State Assistance Programs for SSI Recipients, January 2011, November 2011, https://www.ssa.gov/policy/docs/progdesc/ssi_st_asst/. |
| 176. |
See SSA, POMS, "SI 02302.200 Charted Threshold Amounts," January 25, 2017, https://secure.ssa.gov/poms.nsf/lnx/0502302200. |
| 177. |
Section 1612(b)(2) and 1612(b)(4) of the Social Security Act; 42 U.S.C. §1382a(b)(2) and 1382a(b)(4). See also 20 C.F.R. §§416.1112(c)(5) and 416.1124(c)(12). |
| 178. |
Any portion of the $20 general income exclusion that has not been used to disregard unearned income in a given month can be applied to earned income for that month. See 20 C.F.R. §416.1112(c)(4). |
| 179. |
A person is eligible for the SSI program if his or her monthly countable income is (1) equal to or less than the FBR or (2) less than the FBR plus the amount of applicable federally administered SSP. See SSA, POMS, "SI 02301.215 Summary of Posteligibility (PE) Suspension, Stop Payment and Termination Events by Payment Status Code (PSC)," February 18, 2016, http://policy.ssa.gov/poms.nsf/lnx/0502301215. |
| 180. |
SSA, POMS, "SI 00810.350 Income Break-Even Points General Information," November 6, 2017. http://policy.ssa.gov/poms.nsf/lnx/0500810350. The combined $85 earned income exclusion is the sum of the $20 general income exclusion and the $65 earned income exclusion. |
| 181. |
The example assumes the individual or couple does not receive a SSP. |
| 182. |
2017 Annual Statistical Supplement, Table 7.D1. |
| 183. |
Section 1611(e)(1)(B) of the Social Security Act; 42 U.S.C. §1382(e)(1)(B). See also 20 C.F.R. §§416.212 and 416.414. Some states supplement the reduced SSI payment. |
| 184. |
2017 Annual Statistical Supplement, Table 7.E5. |
| 185. |
Section 1611(c)(7) of the Social Security Act; 42 U.S.C. §1382(c)(7). See also 20 C.F.R. §416.501. |
| 186. |
See SSA, "Medicaid Information," https://www.ssa.gov/disabilityresearch/wi/medicaid.htm. |
| 187. |
42 U.S.C. §§1396 et seq. See CRS Report R43357, Medicaid: An Overview. |
| 188. |
HHS, Centers for Medicare & Medicaid Services (CMS), Office of the Actuary, 2016 Actuarial Report on the Financial Outlook for Medicaid, Table 2, https://www.cms.gov/Research-Statistics-Data-and-Systems/Research/ActuarialStudies/Downloads/MedicaidReport2016.pdf. Estimate includes spending on disabled Medicaid enrollees under 65 years old who are eligible for Medicaid through non-SSI pathways. |
| 189. |
CRS analysis of the 2017 CPS ASEC. A 2015 study that matched SSA administrative records to data from the Survey of Income and Program Participation (SIPP) found that 96.3% of SSI recipients under 18 years old and 96.0% of SSI recipients aged 18-64 reported Medicaid coverage in 2013. See Michelle Stegman Bailey and Jeffrey Hemmeter, Characteristics of Noninstitutionalized DI and SSI Program Participants, 2013 Update, Research and Statistics Note no. 2015-02, September 2015, Table 8, https://www.ssa.gov/policy/docs/rsnotes/rsn2015-02.html (hereinafter "Bailey and Hemmeter 2015"). |
| 190. |
Section 1902(a)(10)(A)(i)(II) of the Social Security Act; 42 U.S.C. §1396a(a)(10)(A)(i)(II). |
| 191. |
42 U.S.C. §1383c. See also 20 C.F.R. §§416.2101-416.2176. |
| 192. |
2017 Congressional Statistics, Table 2 for the applicable states. |
| 193. |
Ibid. |
| 194. |
Section 1902(f) of the Social Security Act; 42 U.S.C. §1396a(f). |
| 195. |
Medicaid and CHIP Payment and Access Commission (MACPAC), MACStats: Medicaid and CHIP Data Book, December 2017, Exhibit 37, p. 109, https://www.macpac.gov/publication/macstats-medicaid-and-chip-data-book-2/. |
| 196. |
2017 Congressional Statistics, Table 2 for the applicable states. |
| 197. |
New Hampshire Revised Statutes §167:3-j. |
| 198. |
Virginia Administrative Code 12VAC30-40-240. |
| 199. |
42 C.F.R. §435.121. 209(b) states must also deduct the value of SSI and any optional SSP from an individual's income in determining Medicaid eligibility. |
| 200. |
State of Oklahoma, Department of Human Services, "Library: Policy: 317:35-5-41.2. Miscellaneous Personal property," March 10, 2017, http://www.okdhs.org/library/policy/Pages/oac317035050041002.aspx. |
| 201. |
State of Indiana, Family and Social Services Administration, "2014 Disability Eligibility Changes FAQ," https://www.in.gov/fssa/ddrs/4861.htm. |
| 202. |
Letter from John B. McCarthy, director, Department of Medicaid, State of Ohio, to All Medicaid Eligibility Manual Holders, Medicaid Eligibility Manual Transmittal Letter No. 116, 2016, http://medicaid.ohio.gov/Portals/0/Resources/Publications/Guidance/MedicaidPolicy/Elig-Chip/MEMTL-116.pdf. |
| 203. |
See CRS Report R42505, Supplemental Nutrition Assistance Program (SNAP): A Primer on Eligibility and Benefits, and CRS Report R42054, The Supplemental Nutrition Assistance Program (SNAP): Categorical Eligibility. |
| 204. |
7 U.S.C. §2014(a) and 7 C.F.R. §273.2(j)(2)(D). |
| 205. |
Under Supplemental Nutrition Assistance Program (SNAP) law, the resources of SSI recipients in the household are deemed to meet the program's resource limitations for purposes of traditional eligibility (i.e., their resources are excluded). See 7 U.S.C. §2014(j) and 7 C.F.R. §273.8(e)(17). However, the SSI payments of household members are considered unearned income under SNAP's traditional eligibility rules and thus are included in the household income calculation. See 7 C.F.R. §273.9(b)(2)(i). |
| 206. |
CRS analysis of the 2017 CPS ASEC. A 2015 study that matched SSA administrative records to data from the SIPP found that 64.9% of SSI recipients under 18 years old and 64.6% of SSI recipients aged 18-64 lived in households that received SNAP benefits in 2013. See Bailey and Hemmeter 2015, Table 9. |
| 207. |
Under SNAP law, SSI recipients living in states that cash out the bonus value of the SNAP allotment are not considered to be a member of the household and thus are ineligible for SNAP benefits. See 7 U.S.C. §2015(g) and 7 C.F.R. §273.20. SSI recipients living in California receive an extra $10 in their monthly SSP in lieu of SNAP benefits. For more information on California's cash-out policy, see State of California, Legislative Analyst's Office (LAO), The Potential Effects of Ending the SSI Cash-Out, January 8, 2018, http://www.lao.ca.gov/Publications/Report/3729. |
| 208. |
SSA, Justifications of Estimates for Appropriations Committees, Fiscal Year 2019, February 12, 2018, Table i.7, https://www.ssa.gov/budget/. |
| 209. |
Ibid. |
| 210. |
2017 Annual Statistical Supplement, Table 7.B7. |
| 211. |
2017 Annual Report of the SSI Program, Table IV.C3. |
| 212. |
Ibid., Table IV.D1. |
| 213. |
CBO, Supplemental Security Income—CBO's April 2018 Baseline, April 10, 2018, https://www.cbo.gov/sites/default/files/recurringdata/51313-2018-04-ssi.pdf. |
| 214. |
The definition of blindness under the SSI program does not require an individual to be unable to perform substantial gainful activity (SGA). |
| 215. |
Sections 223(d)(1)(A) and 1614(a)(3)(A) of the Social Security Act; 42 U.S.C. §§423(d)(1)(A) and 1382c(a)(3)(A). Section 223(d)(1)(B) of the Social Security Act provides an alternative definition of disability for blind individuals who are aged 55 or older. |
| 216. |
Section 1614(a)(3)(C) of the Social Security Act; 42 U.S.C. §1382c(a)(3)(C). |
| 217. |
20 C.F.R. §§404.1572 and 416.972. |
| 218. |
Ibid. |
| 219. |
SSA, OCACT, "Substantial Gainful Activity," https://www.ssa.gov/oact/cola/sga.html. |
| 220. |
Section 1619(a) of the Social Security Act (42 U.S.C. §1382h[a]) provides for the continuation of cash payments for SSI recipients (but not for claimants) with substantial earnings that otherwise would disqualify them from the program. Under this provision, recipients who have earnings at or above the SGA threshold but whose countable income is less than the applicable FBR are eligible to receive special SSI payments in lieu of regular SSI payments. These special 1619(a) payments are calculated in the same manner as regular SSI payments and are payable for as long as an individual performs SGA and meets all other SSI eligibility criteria. 1619(a) effectively eliminates the SGA threshold for non-blind SSI recipients. |
| 221. |
42 U.S.C. §423(d)(4)(A). |
| 222. |
20 C.F.R. §§404.1574 and 416.974. |
| 223. |
Sections 223(d)(2)(C) and 1614(a)(3)(J) of the Social Security Act; 42 U.S.C. §423(d)(2)(C) and 1382c(a)(3)(J). See also 20 C.F.R. §§404.1513(a)(5)(vi), 404.1535, 416.913(a)(5)(vii), and 416.935. |
| 224. |
SSA, "SSR 13-2p: Titles II and XVI: Evaluating Cases Involving of Drug Addiction and Alcoholism (DAA), February 20, 2013 (effective date March 22, 2013), https://www.ssa.gov/OP_Home/rulings/di/01/SSR2013-02-di-01.html. |
| 225. |
20 C.F.R. §§404.1535(b) and 416.935(b). |
| 226. |
See statement of Sarah-Schultz Lackey, spokesperson, SSA, in KTHV-TV, "Patients fear medical marijuana card could cost them their social security benefits," July 3, 2017, http://www.thv11.com/article/news/local/patients-fear-medical-marijuana-card-could-cost-them-their-social-security-benefits-11-listens/453909122. |
| 227. |
SSA, Office of Retirement and Disability Policy, Office of Research, Demonstration, and Employment Support, National Beneficiary Survey: Disability Statistics, 2015, March 2018, Table 8, p. 4, https://www.ssa.gov/policy/docs/statcomps/nbs/2015/index.html. |
| 228. |
Sections 223(f) and 1614(a)(4) of the Social Security Act; 42 U.S.C. §§423(f) and 1382c(a)(4). See also 20 C.F.R. §§404.1513(a)(5)(vi), 404.1530, 404.1579(e)(4), 404.1586(c), 416.913(a)(5)(vii), 404.1594(e)(4), 416.930, 416.986(a)(3), and 416.994(b)(4)(iv). |
| 229. |
SSA, Office of the Inspector General (OIG), Failure to Follow Prescribed Treatment, A-01-15-50024, August 21, 2015, p. 8, https://oig.ssa.gov/audits-and-investigations/audit-reports/A-01-15-50024. |
| 230. |
CRS Report R41289, Disability Benefits Available Under the Social Security Disability Insurance (SSDI) and Veterans Disability Compensation (VDC) Programs. |
| 231. |
CRS Report R44580, Workers' Compensation: Overview and Issues. |
| 232. |
SSA, "Revisions to Rules Regarding the Evaluation of Medical Evidence," 82 Federal Register 5848, January 18, 2017, https://www.gpo.gov/fdsys/pkg/FR-2017-01-18/pdf/2017-00455.pdf. |
| 233. |
This report describes the initial disability determination process for claims with a filing date on or after March 27, 2017. Claims with an earlier filing date are evaluated under somewhat different rules. See 20 C.F.R. §§404.1527 and 416.927. |
| 234. |
20 C.F.R. §§404.1512 and 416.912. |
| 235. |
See SSA, POMS, "DI 22501.002 Responsibilities for Case Development of Disability Claims," March 23, 2016, http://policy.ssa.gov/poms.nsf/lnx/0422501002. |
| 236. |
Sections 221(a) and 1633 of the Social Security Act; 42 U.S.C. §§421(a) and 1383b. |
| 237. |
See SSA, POMS, "DI 24501.001 The Disability Determination Services (DDS) Disability Examiner (DE), Medical Consultant (MC), and Psychological Consultant (PC) Team, and the Role of the Medical Advisor (MA)," December 8, 2017, http://policy.ssa.gov/poms.nsf/lnx/0424501001. |
| 238. |
SSA, "Consultative Examinations: A Guide for Health Professionals," https://www.ssa.gov/disability/professionals/greenbook/ce-guidelines.htm. |
| 239. |
Sections 221, 223(d), and 1614(a)(3) of the Social Security Act; 42 U.S.C. §§421, 423(d), and 1382c(a)(3). |
| 240. |
20 C.F.R. §§404.1520 and 416.920. See also Bernard Wixon and Alexander Strand, Identifying SSA's Sequential Disability Determination Steps Using Administrative Data, Research and Statistics Note no. 2013-01, June 2013, https://www.ssa.gov/policy/docs/rsnotes/rsn2013-01.html. Moreover, see Tom Johns, branch chief, Disability Quality Branch Office of Quality Performance, Dallas, SSA's Sequential Evaluation Process for Assessing Disability, https://www.ssa.gov/oidap/Documents/Social%20Security%20Administration.%20%20SSAs%20Sequential%20Evaluation.pdf. |
| 241. |
20 C.F.R. §§404.1571-404.1576 and 416.971-416.976. |
| 242. |
SSA applies special rules in evaluating the countable income of self-employed claimants and the countable earnings or income of statutorily blind Social Security claimants who are aged 55 or older. |
| 243. |
Certain compensation is not counted as earnings for SGA purposes, such as vacation or sick pay. |
| 244. |
20 C.F.R. §§404.1521 and 416.921. For more information on the terms used in this section, see 20 C.F.R. §§404.1502 and 416.902. |
| 245. |
20 C.F.R. §§404.1529 and 416.929. |
| 246. |
20 C.F.R. §§404.1522 and 416.922. |
| 247. |
Sections 223(d)(2)(B) and 1614(a)(3)(G) of the Social Security Act; 42 U.S.C. §§423(d)(2)(B) and 1382c(a)(3)(G). See also 20 C.F.R. §§404.1523(c) and 416.923(c). |
| 248. |
The Disability Determination Services (DDS) agency cannot combine two or more unrelated severe impairments to meet the 12-month duration requirement. The duration requirement does not apply to blind SSI claimants or to certain blind SSDI claimants aged 55 or older. |
| 249. |
Appendix 1 to Subpart P of 20 C.F.R. §404. |
| 250. |
20 C.F.R. §§404.1525 and 416.925. |
| 251. |
20 C.F.R. §§404.1526 and 416.926. |
| 252. |
Claimants at this stage of the disability determination process are evaluated at a greater level of severity compared with those evaluated at the latter stages, insofar as awards at Step 3 are based on medical factors alone, whereas awards at the later stages take into consideration a claimant's vocational factors, such as age, education, and work experience. In addition, claimants at Step 3 must be unable to perform any gainful activity, which is a stricter standard than any substantial gainful activity. |
| 253. |
20 C.F.R. §§404.1545 and 416.945. |
| 254. |
If there is insufficient evidence of a claimant's past relevant work, the DDS may expedite the claim to Step 5. See 20 C.F.R. §§404.1520(h) and 416.920(h). |
| 255. |
20 C.F.R. §§404.1560 and 416.960. |
| 256. |
See SSA, POMS, "DI 25005.010 Whether Past Relevant Work Must Exist in Significant Numbers in the National Economy (SSR 05-1c)—U.S. Supreme Court Decision in the Case of Jo Anne B. Barnhart, Commissioner of Social Security v. Pauline Thomas," January 27, 2009, http://policy.ssa.gov/poms.nsf/lnx/0425005010. |
| 257. |
The DDS agency may find a claimant disabled if he or she meets the criteria outlined in SSA's special medical-vocational profiles, which describe specific combinations of vocational factors that are considered so unfavorable to a claimant that he or she is deemed unable to adjust to any other work. See 20 C.F.R. §§404.1562 and 416.962. |
| 258. |
Sections 223(d)(2)(A) and 1614(a)(3)(B) of the Social Security Act; 42 U.S.C. §§423(d)(2)(A) and 1382c(a)(3)(B). |
| 259. |
20 C.F.R. §§404.1566 and 416.966. |
| 260. |
Appendix 2 to Subpart P of 20 C.F.R. §404. See also 20 C.F.R. §§404.1563-1565 and 416.963-416.965. |
| 261. |
The medical-vocational rules (i.e., the grids) were established in 1978. See 43 Federal Register 55349. |
| 262. |
The Dictionary of Occupational Titles (DOT) was last updated in 1991. SSA is working with the Bureau of Labor Statistics (BLS) to develop its own occupational information system. See SSA, "Occupational Information System Project," https://www.ssa.gov/disabilityresearch/occupational_info_systems.html. |
| 263. |
20 C.F.R. §416.924. |
| 264. |
20 C.F.R. §416.926a. |
| 265. |
Sections 205(b)(1) and 1631(c)(1)(A) of the Social Security Act; 42 U.S.C. §§405(b)(1) and 1383(c)(1)(A). |
| 266. |
20 C.F.R. §§404.1705 and 416.1505. |
| 267. |
A representative payee is an individual appointed by SSA to receive the benefit payments of a Social Security beneficiary or SSI recipient who is unable to manage or direct the management of his or her benefit payments. |
| 268. |
SSA presumes the date that the individual receives the notice is five days after the date on the notice, unless the individual can demonstrate that he or she did not receive the notice within the five days. |
| 269. |
Sections 205(b) and 1631(c)(1)(A) of the Social Security Act require SSA "to make findings of fact, and decisions as to the rights of any individual applying for a payment" and to give denied claimants "reasonable notice and opportunity for a hearing." Since 1940, SSA's appeals process has consisted of an evidentiary hearing, as well as two additional levels of administrative review—reconsideration prior to the evidentiary hearing (certain exceptions apply) and review by the Appeals Council (AC) after the evidentiary hearing has been conducted. See Social Security Board (SSB), 5 Federal Register 4169, October 22, 1940, https://cdn.loc.gov/service/ll/fedreg/fr005/fr005206/fr005206.pdf. |
| 270. |
SSDI beneficiaries and SSI disability recipients may continue to receive benefit payments pending appeal of a medical cessation determination at the reconsideration and hearing levels of the appeals process, provided they request an appeal and continuation of benefit payments no later than 10 days after the date they receive the notice of the prior determination or decision. However, if SSA later affirms the determination that the individual is not entitled to benefit payments, the individual must pay back any continued benefit payments that he or she received, subject to SSA's overpayment rules. See 20 C.F.R. §§404.1597a and 416.996. |
| 271. |
Sections 205(g) and 1631(c)(3) of the Social Security Act; 42 U.S.C. §§405(g) and 1383(c)(3). |
| 272. |
20 C.F.R. §§404.907-404.922 and 416.1407-416.1422. |
| 273. |
In general, state DDS agencies review medical and vocational issues, while SSA processing centers review all other issues. |
| 274. |
An individual who contests an initial determination of a SSI non-medical issue may request case review, informal conference, or formal conference. A conference is a face-to-face meeting between the individual and the official making the decision, during which the individual is given the opportunity to present his or her case. An informal conference allows an individual to present witnesses. A formal conference allows an individual who contests a non-medical adverse action (i.e., a non-medical determination that the individual is no longer eligible for payments) to request that SSA subpoena adverse witnesses and documents and to cross-examine adverse witnesses. See 20 C.F.R. §§416.1413 and 416.1413c. |
| 275. |
20 C.F.R. §§404.914-404.918 and 416.1414-416.1418. |
| 276. |
SSA, POMS, "DI 12015.100 Disability Redesign Prototype Model," January 16, 2014, http://policy.ssa.gov/poms.nsf/lnx/0412015100. |
| 277. |
SSA, Justifications of Estimates for Appropriations Committees, Fiscal Year 2019, February 12, 2018, p. 25, https://www.ssa.gov/budget/. |
| 278. |
Information presented to CRS by SSA on February 15, 2018. |
| 279. |
20 C.F.R. §§404.929-404.965 and 416.1429-416.1465. See SSA, "Information About Social Security's Hearings and Appeals Process," https://www.ssa.gov/appeals/. |
| 280. |
Administrative law judges (ALJs) are authorized under the Administrative Procedure Act of 1946 (APA; 5 U.S.C. §511 et seq.). ALJs must meet certain minimum standards and pass a test administered by the Office of Personnel Management (OPM). Although the Social Security Act predates the APA and does not explicitly require SSA to use ALJs, the agency has used them (with few exceptions) to adjudicate SSDI and SSI hearings. SSA notes that ALJs "decide matters of fact and law in accordance with the Social Security Act, Administrative Procedure Act (APA), Social Security Administration (SSA) Regulations, Social Security Rulings, and other SSA policy pronouncements." See SSA, POMS, "DI 23020.020 Administrative Law Judge (ALJ) Hearing Cases," January 28, 2008, http://policy.ssa.gov/poms.nsf/lnx/0423020020. According to SSA, "[t]he Commissioner of Social Security has delegated the authority to hold hearings and issue decisions to administrative law judges (ALJ)." See SSA, Hearings, Appeals, and Litigation Law Manual (HALLEX), "I-2-0-2. Hearing Operation—In General," May 1, 2017, https://www.ssa.gov/OP_Home/hallex/I-02/I-2-0-2.html. |
| 281. |
20 C.F.R. §§404.935(a) and 416.1435(a). |
| 282. |
20 C.F.R. §§404.966-404.982 and 416.1466-416.1482. |
| 283. |
The AC reviews cases only under the following conditions: (1) there appears to be an abuse of discretion by the ALJ; (2) there is an error of law; (3) the action, findings or conclusions of the ALJ are not supported by substantial evidence; (4) there is a broad policy or procedural issue that may affect the general public interest; or (5) the AC receives additional evidence that is new, material, and relates to the period on or before the date of the hearing decision, and there is a reasonable probability that the additional evidence would change the outcome of the decision. See 20 C.F.R. §§404.970 and 416.1470. |
| 284. |
20 C.F.R. §§404.969 and 416.1469. |
| 285. |
Sections 205(g) and 1631(c)(3) of the Social Security Act; 42 U.S.C. §§405(g) and 1383(c)(3). See also 20 C.F.R. §§404.983-404.985 and 416.1483-416.1485. |
| 286. |
Sections 223(i) and 1614(a)(4) of the Social Security Act; 42 U.S.C. §§423(i) and 1382c(a)(4). See also 20 C.F.R. §§404.1589, 416.989, and 416.989a. |
| 287. |
20 C.F.R. §§404.1590 and 416.990. |
| 288. |
Applies to centrally processed cases. |
| 289. |
SSA, POMS, "DI 13004.005 An Overview of Processing Continuing Disability Review (CDR) Mailer Forms SSA-455 and SSA-455-OCR-SM," September 23, 2016, http://policy.ssa.gov/poms.nsf/lnx/0413004005. |
| 290. |
Sections 223(f) and 1614(a)(4) of the Social Security Act; 42 U.S.C. §§423(f) and 1382c(a)(4). |
| 291. |
Section 1614(a)(3)(H)(iii) of the Social Security Act; 42 U.S.C. §1382c(a)(3)(H)(iii). See also 20 C.F.R. §416.987. |
| 292. |
SSA, POMS, "DI 33025.075 Age 18 Redetermination Cases Under P.L. 104-193," December 13, 2017, http://policy.ssa.gov/poms.nsf/lnx/0433025075. |
| 293. |
Section 1614(c) of the Social Security Act; 42 U.S.C. §1382c(c). See also 20 C.F.R. §416.204. |
| 294. |
26 U.S.C. §529A. For more information, see CRS In Focus IF10363, Achieving a Better Life Experience (ABLE) Programs, and U.S. Congress, Senate Committee on the Budget, Tax Expenditures: Compendium of Background Material on Individual Provisions, committee print, prepared by the Congressional Research Service, 114th Cong., 2nd sess., December 2016, S.Prt. 114-31 (Washington: GPO, 2017), pp. 1011-1018, at https://www.gpo.gov/fdsys/pkg/CPRT-114SPRT24030/pdf/CPRT-114SPRT24030.pdf. |
| 295. |
SSA, POMS, "SI 01130.740 Achieving a Better Life Experience (ABLE) Accounts," April 2, 2018, https://secure.ssa.gov/poms.nsf/lnx/0501130740. |
| 296. |
Letter from Brian Neale, Director, Center for Medicaid and CHIP Services, to State Medicaid Directors, Implications of the ABLE Act for State Medicaid Programs, September 7, 2017, https://www.medicaid.gov/federal-policy-guidance/downloads/smd17002.pdf. |
| 297. |
7 C.F.R. §273.8(e)(2)(ii). |
| 298. |
Sections 437(a), 455(a)(1), and 464(c)(1)(F) of the Higher Education Act of 1965 (HEA); 20 U.S.C. §§1087(a), 1087e(a)(1), and 1087dd(c)(1)(F). See also 34 C.F.R. §§674.51(aa), 674.61(b), 682.200(b), 682.402(c), 685.102(b), 685.213, and 686.42(b). |
| 299. |
The HEA provides that a qualifying loan may be discharged if the borrower is determined by the Department of Veterans Affairs (VA) to be unemployable due to a service-connected disability or condition. The Department of Education (ED) consulted with the VA and determined that there are two types of VA determinations that meet the requirements of the HEA for the Total and Permanent Disability (TPD) discharge. The first type of determination is that the veteran has one or more service-connected disabilities rated as totally disabling under the VA's rating schedule (i.e., a 100% rating). The second type of determination is that the veteran has one or more service-connected disabilities rated as less than totally disabling (i.e., a rating of less than 100%), but which, in the judgment of the VA, prevent the individual from securing or following a substantially gainful occupation. See ED, Financial Student Aid, "Procedures for discharging Title IV loans based on a determination by the Department of Veterans Affairs that a veteran is unemployable due to a service-connected condition or disability," May 15, 2009, https://ifap.ed.gov/dpcletters/GEN0907.html. For more information on the requirements for the aforementioned VA determinations, see 38 C.F.R. §§3.340, 3.4(b), 4.16, and 4.18. |
| 300. |
ED issued final regulations establishing the SSA method for the TPD discharge in November 2012 (effective July 2013). See ED, "Federal Perkins Loan Program, Federal Family Education Loan Program, and William D. Ford Federal Direct Loan Program," 77 Federal Register 66087, November 1, 2012, https://www.gpo.gov/fdsys/pkg/FR-2012-11-01/pdf/2012-26348.pdf. |
| 301. |
SSA, Benefits Planning Query Handbook (BPQY), July 2012, https://www.ssa.gov/disabilityresearch/documents/BPQY_Handbook_Version%205.2_7.19.2012.pdf. |
| 302. |
34 C.F.R. §§674.61(b)(6)-(7), 682.402(c)(6)-(7), and 685.213(b)(7)-(8). |
| 303. |
See, for example, Sen. Tammy Baldwin, in U.S. Congress, Senate Committee on Health, Education, Labor, and Pensions, Strengthening the Federal Student Loan Program for Borrowers, 113th Cong., 2nd sess., March 27, 2014, S.Hrg. 113-829 (Washington: GPO, 2016), p. 23. |
| 304. |
Executive Office of the President, "Student Aid Bill of Rights To Help Ensure Affordable Loan Repayment," 80 Federal Register 13473, March 4, 2015. See also 20 U.S.C. §1092 note. |
| 305. |
ED, Strengthening the Student Loan System to Better Protect All Borrowers, October 1, 2015, p. 12, https://www2.ed.gov/documents/press-releases/strengthening-student-loan-system.pdf. |
| 306. |
ED, Financial Student Aid, "Total and Permanent Disability (TPD) Match Process with Social Security Administration Begins (Updated May 9, 2016)," https://ifap.ed.gov/eannouncements/041216TPDMatchProcessSSABegins.html. See also ED, "U.S. Department of Education Acts to Protect Social Security Benefits for Borrowers with Disabilities," April 12, 2016, https://www.ed.gov/news/press-releases/us-department-education-acts-protect-social-security-benefits-borrowers-disabilities. Moreover, see ED, Computer Matching Agreement between the Social Security Administration (SSA) and the U.S. Department of Education (ED) Federal Student Aid (FSA): Match #1100, https://www2.ed.gov/about/offices/list/om/docs/pirms/ssa-mine-cma.pdf. |
| 307. |
U.S. Government Accountability Office (GAO), Social Security Offsets: Improvements to Program Design Could Better Assist Older Student Loan Borrowers with Obtaining Permitted Relief, GAO-17-45, December 19, 2016, p. 31, https://www.gao.gov/products/GAO-17-45. According to GAO, as of October 2016, an additional 7,000 borrowers were identified as being eligible for the TPD discharge via the SSA method. |
| 308. |
ED, "U.S. Department of Education and U.S. Department of Veterans Affairs Team Up to Simplify Student Loan Discharge Process for Disabled Veterans," April 16, 2018, https://www.ed.gov/news/press-releases/us-department-education-and-us-department-veterans-affairs-team-simplify-student-loan-discharge-process-disabled-veterans. See also ED, Computer Matching Agreement between the Veterans Administration (VA) and the U.S. Department of Education (ED) Federal Student Aid (FSA), https://www2.ed.gov/about/offices/list/om/docs/pirms/va-tpd-cma.pdf. |
| 309. |
See CRS Report R45092, The 2017 Tax Revision (P.L. 115-97): Comparison to 2017 Tax Law. |
| 310. |
26 U.S.C. §108(f)(5). |