Overview of U.S. Domestic Response to Coronavirus Disease 2019 (COVID-19)
This report discusses selected actions taken by the federal government to quell the introduction and spread of Coronavirus Disease 2019 (COVID-19) in the United States. COVID-19 is causing the third serious outbreak of novel coronavirus in modern times, following severe acute respiratory syndrome (SARS) in 2002 and Middle East Respiratory Syndrome (MERS) in 2012. The global health community is closely monitoring COVID-19 because of the severity of symptoms (including death) among those infected, and the speed of its spread worldwide. At this time, U.S health officials say the general public should be prepared for this virus to gain a foothold throughout the world, including the United States. However, federal agencies have ongoing activities to control and prepare for the spread of COVID-19. Domestic response activities of federal agencies in collaboration with state and local governments include, among others: (1) investigation of COVID-19 cases and infection control measures in the community; (2) travel restrictions and/or quarantine requirements on certain travelers who have recently visited China; (3) medical countermeasure development; and (4) health system preparedness.
Overview of U.S. Domestic Response to Coronavirus Disease 2019 (COVID-19)
Contents
- Background
- Epidemiology of COVID-19
- Domestic Response
- Investigation and Control of COVID-19 Cases in the Community
- The Role of Laboratories in Testing
- Travel-Related Policies and Restrictions
- COVID-19 Travel Restrictions and Quarantine Requirements: Legal Basis
- COVID-19 Travel Restrictions and Quarantine Requirements: Implementation
- Potential Health Effects of Travel Restrictions and Quarantines
- Medical Countermeasures
- Potential Products for Use in the COVID-19 Response
- Status of MCM Development
- FDA Emergency Use Authorization (EUA)
- Health System Preparedness
- Health Care Capability and Capacity
- Supply Chain Management
- Response Funding
Background
On December 31, 2019, the World Health Organization (WHO) was informed of a cluster of pneumonia cases in Wuhan City, Hubei Province of China. Illnesses have since been linked to a disease caused by a previously unidentified strain of coronavirus, designated Coronavirus Disease 2019, or COVID-19. The disease has spread to several other countries, including the United States. As of March 2, 2020, tens of thousands of people have been infected and over 2,500 have died. Both WHO and the U.S. Centers for Disease Control and Prevention (CDC) post frequent updates on the outbreak.1
On January 30, 2020, the Emergency Committee convened by the WHO Director-General declared the COVID-19 outbreak to be a Public Health Emergency of International Concern (PHEIC).2 The next day, on January 31, 2020, U.S. Department of Health and Human Services (HHS) Secretary Alex Azar declared the outbreak to be a Public Health Emergency pursuant to Public Health Service Act (PHSA) Section 319, retroactively dated to January 27, 2020.3
Despite containment efforts in China, the United States, and elsewhere, by late February there were indications that the COVID-19 outbreak may have entered a new phase, with community spread occurring or suspected in several countries other than China, and in at least two U.S. states. According to federal health officials, the COVID-19 outbreak currently meets two of three criteria needed to be considered a pandemic, namely that the disease has caused illness, including illness resulting in death, and that there is sustained person-to-person spread. They note that as community spread is detected in more and more countries, "the world moves closer toward meeting the third criteria, worldwide spread of the new virus."4 In addition, they say
…we should be prepared for Covid-19 to gain a foothold throughout the world, including in the United States. Community spread in the United States could require a shift from containment to mitigation strategies such as social distancing in order to reduce transmission. Such strategies could include isolating ill persons (including voluntary isolation at home), school closures, and telecommuting where possible.5
This report discusses selected actions taken by the U.S. federal government to quell the introduction and spread of COVID-19 in the United States. The President, the HHS Secretary, and other federal officials have taken several specific actions to address this threat. While some of these actions are based in generally applicable authorities, others may be contingent upon the Secretary or another federal official making a determination or declaration, specific to that action, regarding the existence of a public health emergency or threat. Key actions and their legal basis are discussed in this report.
Additional CRS products about this outbreak include
- CRS Report R46209, 2019 Novel Coronavirus (2019-nCoV) Outbreak: CRS Experts;
- CRS In Focus IF11421, COVID-2019: Global Implications and Responses;
- CRS In Focus IF11434, The Coronavirus: U.S.-China Economic Considerations;
- CRS Insight IN11228, COVID-19: Federal Economic Development Tools and Potential Responses.
|
A Snapshot of the Domestic Response to COVID-19, as of March 3, 2020 Note: All dates below are in 2020. International
United States
|
Epidemiology of COVID-19
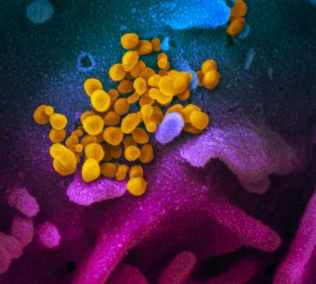
Coronaviruses (see Figure 1) are common respiratory pathogens, usually causing mild illnesses such as the common cold; however, several strains that cause serious illness have emerged in recent years. COVID-19 is the third serious outbreak caused by a novel coronavirus in modern times, following severe acute respiratory syndrome (SARS) in 2002 and Middle East Respiratory Syndrome (MERS) in 2012.6 The global health community is closely monitoring COVID-19 because of the severity of symptoms (including death) among those infected and the speed of its spread worldwide. Experts do not know the origin of COVID-19, though genetic analysis and other features suggest an animal source.7
Health officials and researchers are still learning about COVID-19 (see text box on "What We Know About COVID-19"). COVID-19 is a respiratory infection characterized by a fever, cough, and sometimes breathing difficulty—a suite of symptoms that is common during influenza season.8 Although initial COVID-19 cases likely resulted from animal contact, Chinese officials confirmed person-to-person transmission on January 21, 2020.9 While health officials and researchers are still learning about the disease, CDC has concluded the following about COVID-19:
- Routes of transmission. Based on how similar viruses spread, the virus is thought to spread via respiratory droplets and between people who are in close contact with one another (within about six feet). The virus may also spread via infected surfaces or objects, but according to CDC, this is not thought to be a primary means of transmission.10
- Incubation period. Health officials and researchers are still determining the virus's incubation period, or time between infection and onset of symptoms.11 CDC is using 14 days as the outer bound for the incubation period, meaning that the agency expects someone who has been infected to show symptoms at some point during those 14 days.12
- Transmission from asymptomatic patients. CDC has confirmed that some transmission may occur before people show symptoms, based on a few reports and general characteristics of respiratory viruses.13 However, the agency, WHO, and other health experts agree that asymptomatic spread is unlikely to be a main driver of the outbreak.14
At this time, no specific treatment or preventive vaccine exists for COVID-19. Care for patients is supportive: maintaining hydration, preventing secondary infections, and providing respiratory support, such as use of a ventilator, if needed.15
|
What We Know About COVID-19 As the outbreak has progressed, researchers and health officials have been learning about the disease and its epidemiology. Initially, data and reporting from China, the epicenter from the outbreak, was limited and uncertain. With the recent WHO mission to China and more data coming from other countries, experts have a better understanding of the clinical features of the disease and how it spreads. Some of the key findings include:
Experts are still understanding the exact fatality rate and attack rate (how easily the virus transmits), among other epidemiological characteristics. There is still uncertainty if the full spectrum of disease (including all mild cases) has been captured in the data from other countries, which affects our understanding of severity and transmission. Regardless, estimates suggest that the disease has a higher case fatality rate than the annual flu. Given the uncertainty, CRS presents conclusions that have been made by CDC and/or WHO. See WHO, "Report of the WHO-China Joint Mission on Coronavirus Disease (COVID-19)," February 16-24, 2020, https://www.who.int/docs/default-source/coronaviruse/who-china-joint-mission-on-covid-19-final-report.pdf. |
Domestic Response
The nation has both planning and real-world experience with pandemic infectious diseases, most notably the influenza pandemic of 2009.16 Although COVID-19 is from a different family of viruses, its similarity to influenza—the route of spread, respiratory system effects, and the possible role of antiviral drugs and vaccines, for example—allow the body of influenza experience and plans across government and the private sector to be applied to the COVID-19 response, with modest adjustments.17
Domestic communicable disease control involves collaboration among federal agencies, state health departments, and international partners. Many public health authorities are based in state law, such as authority to compel isolation (for sick patients), quarantine (for healthy exposed persons), and disease reporting.18 The HHS Secretary and, by delegation, CDC have broad authority to assist in the control of communicable diseases through international cooperation, federal-state cooperation, and public health emergency response activities.19 CDC (by delegation) also has explicit authority to detain, examine, and release persons arriving into the United States, and traveling between states, who are suspected of having a communicable disease.20 Other authorities, such as those in the Immigration and Nationality Act of 1952 (INA, P.L. 82-414), allow for other actions relevant to communicable disease control, such as travel restrictions.21
The use of federal and state disease control authorities and other key actions taken in response to the COVID-19 outbreak are discussed below. These activities of federal agencies in collaboration with state and local governments include, among others (1) investigation of COVID-19 cases and infection control measures in the community, (2) travel restrictions and/or quarantine requirements on certain travelers who have recently visited China, (3) medical countermeasure development, and (4) health system preparedness. Federal agencies involved include several HHS agencies, such as CDC, the Assistant Secretary for Preparedness and Response (ASPR), the National Institutes of Health (NIH), and the U.S. Food and Drug Administration (FDA), in collaboration with other agencies such as the U.S. Department of State and the Department of Homeland Security (DHS).
Investigation and Control of COVID-19 Cases in the Community
To curb the spread of COVID-19 cases in the community, state, tribal, local, and territorial health departments, with support from CDC, work to identify cases, investigate the possible spread of disease, and take infection control measures.
Case identification begins with diagnostic testing for COVID-19. As of February 27, CDC guidance urges clinicians to consider a patient's travel and/or contact history, as well as symptoms when deciding to test for COVID-19. CDC recommends COVID-19 testing for patients without known travel and/or contact history if clinical features include, "fever with severe acute lower respiratory illness ... requiring hospitalization and without alternative explanatory diagnosis (e.g., influenza)."22 (See the next section, "The Role of Laboratories in Testing" for more information about the CDC-developed test.) Health care providers are urged to report possible cases to jurisdictional health departments, which then report to CDC.23
Once a patient is reported and in the process of having specimens tested, he or she is considered a patient under investigation (PUI) for COVID-19. CDC has developed guidelines for isolation and other precautions for PUIs (including potential PUIs) or those receiving supportive care for COVID-19 infection in health care settings.24 A key goal of the guidelines is the prevention of disease transmission to health care workers, who may be exposed through high-risk procedures, such as maintaining an ill patient on a ventilator.25
Disease investigation for confirmed cases involves contact tracing—identifying and evaluating individuals who had contact with the patient to determine if transmission has occurred. These investigations are generally conducted by jurisdictional health officials, often with support and technical assistance from CDC.26 CDC has reported community spread in three states during the week of February 23, including a potential outbreak in a long-term care facility.27
Jurisdictional health departments may take actions at a local level to control the spread of COVID-19. For example, the government of Washington State declared a state of emergency on February 29.28 In addition, schools in the states of Washington and Oregon have had temporary closures due to presumptive positive COVID-19 cases.29 If and when outbreaks continue, jurisdictions may consider actions such as cancellation of events and encouraging telecommuting for workers. Such actions would be based in state and local level authorities.
As of February 29, 2020, CDC reported that it had "deployed multidisciplinary teams to support health departments with clinical management, contact tracing, and communications."30 In addition, the Public Health Emergency declaration by Secretary Azar, pursuant to PHSA Section 319, gives jurisdictional health departments more flexibility to reassign personnel to respond to COVID-19.
The Role of Laboratories in Testing
Every state, territory, and the District of Columbia has a central public health laboratory. These laboratories play many roles, including specialized testing for the detection and identification of infectious disease.31 Depending on the structure of their respective public health systems, states may also operate local public health laboratories.32 Health care facilities and businesses also separately operate laboratories outside of the public health laboratory system and are regulated by the FDA.
Typically, in emergency situations involving novel pathogens, diagnostic testing is initially centralized under CDC because CDC has the equipment, trained personnel, and facilities to provide the containment necessary to safely carry out the testing. Once a CDC-developed test is ready and meets any related regulatory requirements, the test may be distributed to state and local public health laboratories to expand testing capacity.
Initially, CDC performed all domestic COVID-19 testing, using a diagnostic test it developed, and continues to confirm presumptive positive cases.33 The CDC test, 2019-nCoV Real-Time RT-PCR Diagnostic Panel, is a molecular diagnostic test that requires specialized equipment and laboratory expertise.34 It is intended for use only by laboratories designated by CDC as qualified and certified to perform high-complexity testing under the CLIA (Clinical Laboratory Improvement Amendments of 1988) program, administered by the HHS Centers for Medicare & Medicaid Services (CMS).35 In the national Laboratory Response Network (LRN) supported by CDC, approximately 130 laboratories, mostly governmental, have the capability to perform specialized testing for high-risk clinical samples, such as those for COVID-2019.36
On February 5, 2020, CDC announced that it would begin distributing test kits to jurisdictional laboratories, following an Emergency Use Authorization from FDA (see the "Medical Countermeasures" section for more details).37 After distribution began, problems with one of the reagents (i.e., test chemicals), later reported to be linked to manufacturing, led to inconclusive test results in many laboratories.38 Performance problems with the CDC test persisted throughout the month of February.
On February 27, 2020, CDC and FDA reported that the problem of inconclusive test results was resolved and that newly manufactured tests were again being distributed to state and local public health laboratories.39 CDC reported that 40 laboratories in 32 states and the District of Columbia had received test kits, with additional kits to be made available to public health laboratories through the International Reagent Resource (IRR), a repository established by CDC.40 Domestic laboratories are not charged for reagents or shipping from the IRR.
For more information on U.S. diagnostic testing, see CRS Report R46261, Development and Regulation of Domestic Diagnostic Testing for Novel Coronavirus (COVID-19): Frequently Asked Questions, by Amanda K. Sarata.
Travel-Related Policies and Restrictions
Given that initially the spread of COVID-19 cases was linked to travel, particularly to mainland China, several policies have been implemented to curb travel-related cases. These have included CDC and State Department advisories to avoid travel to certain countries, and specific restrictions and quarantine requirements on travelers returning from mainland China or Iran pursuant to presidential proclamations (further explained below). In addition, screening programs have been implemented at U.S. airports and other ports of entry to evaluate the health of returning travelers. As COVID-19 continues to spread globally, screening and entry policies may continue to evolve.
COVID-19 Travel Restrictions and Quarantine Requirements: Legal Basis
The Trump Administration has imposed two types of movement restrictions to prevent the entry and/or spread of COVID-19 in the United States. First, an immigration restriction generally suspends the entry of foreign nationals who have been in mainland China or in the Islamic Republic of Iran (Iran) within the prior 14 days.41 Second, quarantine requirements have been imposed on persons entering the United States if they have been in mainland China within the prior 14 days.42 Persons entering the United States who have been in Iran within the prior 14 days are subject to health monitoring. 43
Entry Restriction
President Trump issued a Proclamation on January 31, 2020, that suspends the entry of any foreign national who has been in mainland China within the prior 14 days, subject to some exceptions.44 Hong Kong and Macau, both Special Administrative Regions of the People's Republic of China, are explicitly exempted. The China Proclamation directs the U.S. Department of State and the Department of Homeland Security (DHS) to establish procedures for implementing and enforcing the entry restrictions, which by the Proclamation's terms took effect on February 2, 2020. On February 29, 2020, President Trump issued another Proclamation with similar restrictions and exceptions for foreign nationals who had been in Iran within the prior 14 days.45 In similar fashion, the Iran Proclamation's terms took effect on March 2, 2020. Both proclamations excepted lawful permanent residents (LPRs), most immediate relatives of U.S. citizens and LPRs, and some other groups such as some airplane and ship crew members.46
For statutory authority, the Proclamations rely principally upon Section 212(f) of the Immigration and Nationality Act (INA).47 That statute authorizes the President to "suspend the entry of all aliens or any class of aliens" whose entry he "finds ... would be detrimental to the interests of the United States."48 The Supreme Court has held that Section 212(f) "exudes deference to the President in every clause" and gives him mostly unfettered discretion to decide "when to suspend entry," "whose entry to suspend," "for how long," and "on what conditions."49 The Proclamations are in effect until terminated by the President.50 The Proclamations also direct the Secretary of Health and Human Services (HHS) to "recommend that the President continue, modify, or terminate this proclamation and any other proclamation suspending or limiting the entry of foreign nationals into the United States as immigrants or nonimmigrants because of the threat posed by the virus."51 Such recommendation is required "no more than 15 days after the date of this order and every 15 days thereafter."52
Although the Supreme Court has affirmed broad presidential discretion in the application of Section 212(f), the travel restriction applied in response to COVID-19 is the first such use of this authority to control the spread of a communicable disease.
Quarantine Requirements
DHS announced quarantine requirements, for arrivals on and after February 2, 2020 from China, and for arrivals from Iran, as of March 2, 2020.53 Travelers who arrive in the United States within 14 days after having been in mainland China, are to be screened at one of 11 designated airports (see text box). Such persons may also be subject to mandatory quarantine, pursuant to the standing quarantine authorities of the HHS Secretary under Section 361 of the Public Health Service Act (PHSA).54 These authorities are generally implemented by the CDC through its Division of Global Migration and Quarantine.55 Persons showing symptoms of illness are to be evaluated by CDC staff to determine if they should be taken to a hospital for medical evaluation and to get care as needed.56 Asymptomatic persons are generally to be held under federal quarantine for 14 days from the time they left China if they have recently visited China's Hubei Province. However, asymptomatic persons whose recent travels have not included Hubei Province, are asked to self-quarantine for 14 days.57 Persons entering the United States who have been in Iran within the prior 14 days are subject to health monitoring.58
Prior to the COVID-19 response, the HHS/CDC federal quarantine authority had not been used to restrict the movement of people since the early 1960s.59 The CDC, however, regularly applies its quarantine authorities to assure that imports of animals, animal products, and other goods are free from diseases that could be transmitted to humans.60 Authority to compel isolation (for sick human patients) and quarantine (for healthy exposed persons) has generally been exercised under state law.61
(Of note, in addition to announcing the United States' use of entry restrictions and quarantine authority on January 31, 2020, HHS Secretary Azar declared the COVID-19 outbreak to be a Public Health Emergency, pursuant to PHSA Section 319.62 This declaration was not statutorily required for the abovementioned entry restrictions and quarantine requirements to go into effect, as each of these legal authorities is independent of the others. However, this declaration allows other actions, such as permitting states to reassign personnel on federal grants in order to respond to the emergency.)
COVID-19 Travel Restrictions and Quarantine Requirements: Implementation
In large part, the exclusion of foreign nationals who have been in mainland China within the past 14 days has been carried out by commercial airlines, who are working with DHS to comply with new requirements, and many carriers have cancelled flights from mainland China.63 Expanded exit screening of travelers in South Korea, Italy, and other countries, in addition to those traveling from China, are being put in place.64
In addition, personnel from DHS components—namely Customs and Border Protection (CBP) and the Transportation Security Administration (TSA)—are involved in excluding foreign nationals from entry once travelers arrive at a port of entry in the United States, whether due to the January 31 and February 29 Presidential Proclamations or for unrelated reasons under immigration law. These flights are arriving in one of 11 U.S. airports (see text box).65
Entry Restriction
In large part, the exclusion of foreign nationals who have been in mainland China within the past 14 days has been carried out by commercial airlines, who are working with DHS to comply with new requirements, and many carriers have cancelled flights from mainland China.66 Expanded exit screening of travelers in South Korea, Italy, and other countries, in addition to those traveling from China, are being put in place.67
In addition, personnel from DHS components—namely Customs and Border Protection (CBP) and the Transportation Security Administration (TSA)—are involved in excluding foreign nationals from entry once travelers arrive at a port of entry in the United States, whether due to the January 31 and February 29 Presidential Proclamations or for unrelated reasons under immigration law. These flights are arriving in one of 11 U.S. airports (see text box).68
|
U.S. Airports Accepting Passengers Who Have Been in Mainland China Within 14 Days John F. Kennedy International Airport (JFK), New York Chicago O'Hare International Airport (ORD), Illinois San Francisco International Airport (SFO), California Seattle-Tacoma International Airport (SEA), Washington Daniel K. Inouye International Airport (HNL), Hawaii Los Angeles International Airport, (LAX), California Hartsfield-Jackson Atlanta International Airport (ATL), Georgia Washington-Dulles International Airport (IAD), Virginia Newark Liberty International Airport (EWR), New Jersey Dallas/Fort Worth International Airport (DFW), Texas Detroit Metropolitan Airport (DTW), Michigan |
Quarantine Requirements for Travelers Arriving from China
Upon arrival at one of the designated U.S. airports, the health status and travel history of individuals who have been in mainland China within the prior 14 days are evaluated to determine the need for mandatory quarantine (if they have been in Hubei Province within the prior 14 days); isolation (if they are symptomatic and/or test positive for coronavirus infection); or education and self-quarantine (if they have been elsewhere in mainland China within the prior 14 days). These passenger screenings have been conducted by personnel from CDC with assistance from CBP. The Department of State has also assisted American citizens, LPRs, and other persons who are permitted to return to the United States, by providing a number of repatriation airline flights, among other assistance.69 According to CDC, as of February 23, "A total of 46,016 air travelers had been screened at the 11 U.S. airports to which all flights from China are being directed."70
Travelers designated for mandatory quarantine have generally been housed on military bases for a 14-day period. While in quarantine, the individuals are monitored and their care and basic needs attended to by personnel from CDC, the office of the HHS Assistant Secretary for Preparedness and Response (ASPR), officers of the U.S. Public Health Service Commissioned Corps, and deployed teams from the National Disaster Medical System (see Figure 2).71
Individuals who self-quarantine are directed to monitor their health and remain away from public places where close contact may occur (e.g., workplaces) for 14 days from the time the person was possibly exposed. State or local health departments are to provide oversight for individuals who self-quarantine.72
|
Figure 2. HHS Responders at Travis Air Force Base Taken February 5, 2020 |
 |
|
Source: HHS Assistant Secretary for Preparedness and Response (ASPR), Flickr photostream, https://www.flickr.com/photos/phegov/with/49531565831/. Notes: "When evacuees from Wuhan arrived at Travis Air Force Base on February 5, responders from the National Disaster Medical System (NDMS) and the U.S. Public Health Service Commissioned Corps were there to evaluate evacuees for symptoms of COVID19 and stood ready to help. The U.S. Department of Health and Human Services (HHS) is continuing to take steps to fight COVID-19 and keep Americans healthy." Wuhan is the capital of Hubei Province in mainland China. |
Potential Health Effects of Travel Restrictions and Quarantines
Proposals to restrict the movement of people from affected regions or countries are part of early discussions when novel communicable diseases arise. The World Health Organization (WHO) generally advises against nations imposing travel restrictions on other nations, citing limited evidence of the effectiveness of such measures in controlling outbreaks and the harmful economic effects they have on nations struggling with outbreaks.73 On January 27, 2020, WHO stated, with respect to COVID-19, that it "advises against the application of any restrictions of international traffic based on the information currently available on this event."74 However, on February 11, WHO issued more nuanced guidance, saying
Evidence on travel measures that significantly interfere with international traffic for more than 24 hours shows that such measures may have a public health rationale at the beginning of the containment phase of an outbreak, as they may allow affected countries to implement sustained response measures, and non-affected countries to gain time to initiate and implement effective preparedness measures. Such restrictions, however, need to be short in duration, proportionate to the public health risks, and be reconsidered regularly as the situation evolves.75
WHO's guidance then discusses the measures it recommends be taken in managing travelers before embarkation, en route, upon arrival and, if indicated, while in quarantine.
The effect of movement restrictions on the spread of communicable diseases is generally considered poorly understood for several reasons, including (1) limited contemporary examples for study; (2) the inherent variability in the natural progression of global disease outbreaks, even those caused by the same pathogen; (3) variation in actions taken by affected countries and restrictions imposed by other countries; and (4) difficulty in accounting for the effects of nongovernmental actions such as event cancellations and airline flight adjustments. In response to the emergence of COVID-19, China imposed sweeping internal movement restrictions,76 a measure that is likely, in later analyses, to obscure or confound any additional transmission-damping effects that the U.S.-imposed travel restrictions may achieve.
Several studies have examined the potential effects of travel restrictions on disease spread, particularly looking at the global spread of influenza and at the outbreak of Severe Acute Respiratory Syndrome (SARS) in 2002-2003. Of note, these analyses sometimes indicated delays in the speed of spread of an outbreak. However, the effect of travel restrictions on the ultimate geographic spread of the outbreak—or on the reduction of overall morbidity or mortality—is unclear, and the evidence base is limited. Some studies have found no effect of travel restrictions on overall morbidity and mortality of infectious disease.77 Others have found that very strict travel restrictions may effectively prevent the spread of disease (i.e., complete border closure) or that travel restrictions might be more effective when combined with other infection control measures, such as quarantine and isolation.78 In particular, compulsory movement restrictions may rely on public support in order to be effective, as well as to avoid discrimination and loss of public trust. Many suggest that if public support and trust are essential in any case, enlisting movement restriction through voluntary measures may be just as effective, with less societal disruption.79
Quarantine has a long history as a disease control measure, substantially predating the "germ theory" of infectious disease embraced in the late 19th century. According to CDC,
The practice of quarantine, as we know it, began during the 14th century in an effort to protect coastal cities from plague epidemics. Ships arriving in Venice from infected ports were required to sit at anchor for 40 days before landing. This practice, called quarantine, was derived from the Italian words quaranta giorni which mean 40 days.80
Quarantine is considered a social distancing measure in public health, along with isolation, contact tracing, and measures to avoid crowding (i.e., school closures). Similar to the studies on movement restrictions, the precise effect of social distancing measures on the spread of infectious disease can be difficult to measure and the evidence base is limited.81 Yet, social distancing measures were some of the primary means by which the 2003 SARS outbreak in China was contained and are generally considered fundamental tools of infection control in public health.
Medical Countermeasures
Potential Products for Use in the COVID-19 Response
Medical countermeasures (MCMs) are medical products that may be used to treat, prevent, or diagnose conditions associated with emerging infectious diseases or chemical, biological, radiological, or nuclear (CBRN) threats. Examples of MCMs include biologics (e.g., vaccines, monoclonal antibodies), drugs (e.g., antimicrobials, antivirals), and devices (e.g., diagnostic tests and general personal protective equipment such as gloves, respirators/masks, and gowns).82 FDA regulates MCMs domestically. Currently, there are no FDA-approved MCMs specifically for COVID-19, although FDA has authorized the use of unapproved diagnostic tests, including via Emergency Use Authorization (EUA).83 Federal agencies, pharmaceutical and biotech companies, nongovernmental organizations, and global regulators have been working to expedite the development and availability of MCMs for 2019-nCoV. Examples of such efforts include the following:
Diagnostics
As summarized earlier, CDC developed the 2019-nCoV Real-Time RT-PCR Diagnostic Panel for which FDA issued an EUA on February 4, 2020 (EUAs are described in more detail below).84 The CDC test is a "test kit," meaning it is manufactured, assembled, and then may be shipped for use by multiple laboratories. In contrast, many diagnostic tests are "laboratory-developed tests," meaning that they are developed, validated, and used in a single laboratory. Generally, the FDA waives most regulatory requirements (e.g., premarket review) for LDTs, but nevertheless, LDTs may only be used with authorization (an EUA) during an emergency declaration pursuant to FFDCA Section 564.
On February 29, 2020, as problems with the roll-out of the CDC-developed diagnostic test continued, FDA announced a new policy to immediately leverage LDTs developed in high-complexity commercial, reference, and clinical laboratories nationwide to expand testing capacity. Specifically, the new guidance from the agency allows the nation's CLIA-certified high-complexity laboratories that have developed and validated their own COVID-19 diagnostics to begin to use the tests while the laboratory is preparing, and FDA is reviewing, their EUA submissions.85 The FDA guidance recommends that laboratories have 15 days after validating their test to submit their EUA application to the FDA, and recommends confirming the test's first five negative and positive results against an EUA-authorized diagnostic. According to FDA, it "does not intend to object to the use of these tests for clinical testing while the laboratories are pursuing an EUA with the FDA. Importantly, this policy only applies to laboratories that are certified to perform high-complexity testing consistent with requirements under Clinical Laboratory Improvement Amendments."86
Several federal agencies are working with industry partners to develop rapid diagnostic point-of-care tests for COVID-19, including NIH, particularly through the National Institute of Allergy and Infectious Diseases (NIAID); ASPR, through the Biomedical Advanced Research and Development Authority (BARDA); and the Department of Defense (DOD).87 On February 5, 2020, BARDA announced an Easy Broad Agency Announcement (EZ-BAA) to solicit applications for development funding of COVID-19 molecular diagnostics. The submissions must have a viable plan to meet requirements for the FDA to consider EUA within 12 weeks of an award.88
Therapeutics
Research and development into several treatment strategies for COVID-19 are underway by federal agencies, international partners, and industry. Drawing from research on the SARS and MERS coronaviruses, NIAID is assessing potential treatment strategies such as antiviral drugs and animal models that can be used to test potential MCMs. In addition, NIAID is developing assays and other research tools to study COVID-19.89 In February 2020, BARDA announced that it would expand existing collaborations with Regeneron Pharmaceuticals Inc. and Janssen Research and Development to develop COVID-19 therapeutics.90
Scientists in China are testing drugs currently approved for treatment of HIV, influenza (flu), and malaria for potential effectiveness against COVID-19.91 For example, Chinese authorities have reportedly recommended AbbVie's HIV drug Kaletra to treat patients, while the drug undergoes clinical testing.92 Johnson & Johnson has reportedly provided its HIV drug Prezcobix to China to test as a potential treatment as well.93 Scientists are also testing many experimental treatments in the research pipeline.94 For example, Gilead is working with health authorities in China to determine whether its experimental antiviral drug Remdesivir can safely and effectively treat COVID-19.95 In the United States, a clinical trial evaluating the safety and effectiveness of Remdesivir has begun at the University of Nebraska Medical Center (UNMC) in Omaha. The trial is sponsored by NIAID.96
Vaccines
At least eight different COVID-19 vaccine development initiatives among federal agencies, industry, research institutions, and philanthropies have been announced.97 Of note, the NIAID Vaccine Research Center (VRC) is collaborating with the drug company Moderna and the Coalition for Epidemic Preparedness Innovations (CEPI) to advance a vaccine candidate. Moderna expects this vaccine to enter phase 1 clinical testing in the spring of 2020.98 CEPI is also supporting vaccine development by the University of Queensland (Australia) and the drug companies GlaxoSmithKline and Inovio.99 BARDA has announced vaccine development partnerships with Sanofi and Johnson & Johnson.100
Status of MCM Development
MCM development for COVID-19 has exceeded the pace of MCM development for previous infectious disease outbreaks; however, it is still uncertain if the products will be available in time to curb spread of the virus. Diagnostic tests for COVID-19 were developed by CDC and other global public health laboratories in a few weeks after COVID-19 was first reported, compared to almost six months for the 2002-2003 SARS outbreak.101 The NIAID supported Moderna vaccine is expected to begin phase 1 clinical trials in late April. In comparison, it took 20 months for NIAID to get a SARS vaccine into phase 1 clinical trials.102 However, vaccine development is difficult and only a handful of new vaccines have been licensed in recent decades, despite ongoing efforts to develop vaccines for infectious diseases such as MERS and HIV.103 Additionally, the NIAID and Moderna vaccine relies on a new technology that no FDA-approved vaccine has ever used.104 An FDA official has reportedly asserted that therapeutics for COVID-2019 are likely to be available more quickly than a vaccine.105
FDA Emergency Use Authorization (EUA)
Clinical testing and the FDA review process typically take several years, so it will take time for MCMs in development to reach the commercial market. However, experimental products may become available in the United States prior to FDA approval pursuant to an EUA. FDA encourages industry and government sponsors (e.g., CDC) to engage with FDA prior to submitting a formal request for an EUA, if possible.
Under most circumstances, drugs, medical devices, and biologics may be introduced into interstate commerce only if they have been approved, cleared, or licensed by FDA. Under certain circumstances, however, FDA may permit a medical product to be provided to patients outside the standard regulatory framework, including through issuance of an EUA. In the absence of an approved MCM for COVID-19, FDA may enable access to investigational MCMs by issuing an EUA, if the HHS Secretary declares that circumstances exist to justify the emergency use of an unapproved product or an unapproved use of an approved medical product.106 The HHS Secretary's declaration must be based on one of four determinations; for example, a determination that there is an actual or significant potential for a public health emergency that affects or has significant potential to affect national security or the health and security of U.S. citizens living abroad.107 Following the HHS Secretary's declaration, FDA, in consultation with ASPR, NIH, and CDC, may issue an EUA authorizing the emergency use of a specific drug, device, or biologic, provided that certain criteria are met (e.g., that there is no adequate, approved, and available alternative to the product).108
On February 4, 2020, the HHS Secretary determined that there is a public health emergency that has a significant potential to affect national security or the health and security of U.S. citizens living abroad, and that involves the COVID-2019.109 This emergency determination by the HHS Secretary is distinct from the Public Health Emergency declaration made pursuant to PHSA Section 319. On the basis of this determination, on February 4, 2020, the HHS Secretary declared that circumstances exist justifying the authorization of emergency use of in vitro diagnostics for the detection and/or diagnosis of COVID-2019. This declaration allowed FDA to issue an EUA authorizing the emergency use of the CDC-developed diagnostic test for COVID-2019. Pursuant to the same February 4, 2020 determination, on March 2, 2020, the HHS Secretary declared that circumstance exist justifying the emergency use of personal respiratory protective devices during the COVID-19 outbreak. This declaration allowed FDA to issue a second EUA—this one authorizing the emergency use of certain respirators in health care settings by health care personnel "to prevent wearer exposure to pathogenic biological airborne particulates during FFR [filtering facepiece respirator] shortages resulting from the COVID-19 outbreak."110
Health System Preparedness
Health Care Capability and Capacity
There is concern that if COVID-19 spreads widely in the community, it will overwhelm the health care system's ability to care for patients and prevent further spread of the disease. Given that it is currently flu season, many health care facilities are already at or near patient capacity.
The ASPR is the principal advisor to the HHS Secretary on the public health and medical preparedness and response for public health emergencies.111 CDC is the nation's leading public health agency. Since 2002, the ASPR and CDC have funded grants to states for health system and public health preparedness, respectively.112 These grants have fostered nationwide development of several response capabilities that would be called upon for a successful response to the COVID-19 threat, including the folloiwng:
- Medical surge: "…the ability to provide adequate medical evaluation and care during events that exceed the limits of the normal medical infrastructure of an affected community. It encompasses the ability of the health care system to endure a hazard impact, maintain or rapidly recover operations that were compromised, and support the delivery of medical care and associated public health services, including disease surveillance, epidemiological inquiry, laboratory diagnostic services, and environmental health assessments."113 ASPR and CDC are projecting the potential long-term impact of COVID-19 and assessing the capacity of the health care system to respond to a larger outbreak. A sustained response could engage the Regional Treatment Network for Ebola and Other Special Pathogens, a tiered health system response network developed with funding provided by Congress for response to the Ebola outbreak in 2015.114
- Nonpharmaceutical interventions (NPI): "…actions that people and communities can take to help slow the spread of illness or reduce the adverse impact of public health emergencies. This capability focuses on communities, community partners, and stakeholders recommending and implementing [NPI] in response to the needs of an incident, event, or threat."115 Interventions may include isolation, quarantine, restrictions on movement and travel advisories or warnings, social distancing, external decontamination, hygiene, and precautionary protective behaviors.
- Medical countermeasure dispensing and administration: "…the ability to provide medical countermeasures to targeted population(s) to prevent, mitigate, or treat the adverse health effects of a public health incident. This capability focuses on dispensing and administering medical countermeasures, such as vaccines, antiviral drugs, antibiotics…."116 The Strategic National Stockpile (SNS), managed by ASPR, provides select medicines and medical supplies during public health emergencies when local supply chains are disrupted.117
The National Health Security Preparedness Index (NHSPI, or the Index), a public-private partnership begun in 2013, currently assesses preparedness, using 140 measures, across all 50 states and the District of Columbia.118 In its latest comprehensive report, for 2017, NHSPI found overall incremental improvements over earlier years in capabilities such as disease surveillance and medical countermeasures management. However, the report highlighted differing preparedness levels among states, stating
Large geographic areas in the Deep South and Mountain West trail the rest of the nation in health security, leaving many low-income populations and rural residents at elevated risk.119
In addition, measures of health care delivery—for example, the number of certain types of health care providers (including mental health providers) per unit of population, access to trauma centers, the extent of preparedness planning in long-term care facilities, and uptake of electronic health record systems—and of community planning and engagement—for example, the degree of coordination between public health authorities and the health care system—continued to yield the lowest scores among the indicators across the United States.
Supply Chain Management
ASPR, CDC, and FDA play roles in protecting against and preparing for the potential impact of the COVID-19 virus on the medical product supply chain, including shortages of critical drugs and medical devices such as personal protective equipment (PPE). ASPR, FDA, and CDC have indicated that they are working with health care and/or industry partners to ensure an adequate supply of medical products needed to contain the outbreak and to identify potential disruptions or shortages.120 A chief concern in supply chain management is that many medical products or drugs are manufactured, at least in part, in China, the epicenter of the current outbreak.121
By law, drug manufacturers are required to notify FDA of a permanent discontinuance of or interruption in the manufacture of a drug that is likely to lead to a disruption in its supply.122 Based on the reported information, FDA may take various actions to mitigate or prevent a drug shortage from occurring, such as expediting applications for approval from other manufacturers and allowing for the temporary importation of unapproved drugs.123 Currently, there are no parallel reporting requirements for medical devices.
Some have concerns with respect to FDA's ability to inspect and monitor compliance of FDA-regulated products manufactured overseas and particularly in China. As of February 24, 2020, FDA is not conducting inspections in China due to the State Department travel advisory. Inspections in China scheduled for February 2020 have been either postponed, or the agency is using different means to obtain information to inform regulatory decisions about FDA-regulated products manufactured in these facilities.124 While there are no FDA-licensed vaccines, gene therapies, or blood derivatives manufactured in China, the raw materials used to produce these biologics are manufactured in China and other countries in Southeast Asia.125 In addition, according to FDA data, 72% of facilities that manufacture active pharmaceutical ingredients (APIs) for drugs are located outside of the United States, with 13% of facilities in China; 53% of facilities manufacturing finished drugs are located outside of the United States, with 7% of facilities in China.126 These numbers are not reflective of product volume. FDA is not able to determine what volume of APIs being used for the U.S. market is from China, as manufacturers are not required to report this information to the agency.
Response Funding
CDC and other federal agencies may have the authority needed to respond to the COVID-19 epidemic, but their ability to act may be affected by the availability of appropriations. Annual appropriations and standing transfer authority provide the HHS Secretary with some flexibility.127 Upon a declaration of a Public Health Emergency pursuant to PHSA Section 319—which HHS Secretary Azar made on January 31, 2020—HHS may access a Public Health Emergency Fund,128 but the fund does not have an available balance at this time. Separately, funding has generally not been available under the Robert T. Stafford Disaster Relief and Emergency Assistance Act (the Stafford Act) for the response to infectious disease outbreaks. As a result, Congress and the President provided supplemental appropriations for the response to the recent Ebola and Zika virus outbreaks in FY2015 and FY2016.129
In 2018, Congress established an Infectious Diseases Rapid Response Reserve Fund (IDRRRF) for CDC, providing appropriations of $50 million for FY2019 (P.L. 115-245) and $85 million for FY2020 (P.L. 116-94), available until expended.130 These funds may be made available for an infectious disease emergency if the HHS Secretary either (1) declares a Public Health Emergency pursuant PHSA Section 319, or (2) determines that the infectious disease outbreak has significant potential to occur and, if it occurs, the potential to affect national security or the health and security of U.S. citizens, both domestically and abroad.
Before HHS Secretary Azar declared the COVID-19 outbreak to be a Public Health Emergency under PHSA Section 319, he issued a determination on January 25, 2020, allowing the allotment of $105 million from the IDRRRF for the COVID-19 response.131 Secretary Azar had previously determined that the U.S. response to the Ebola outbreak in the Democratic Republic of Congo allowed the use of up to $30 million from the IDRRRF. If both the Ebola and COVID-19 amounts are fully used, all funds currently in the IDRRRF would be exhausted.132 On February 2, 2020, HHS reportedly notified Congress of its intention to use the Secretary's standing authority to transfer up to $136 million for COVID-19 response efforts, of which $75 million would be made available to CDC, $52 million for ASPR, and $8 million for the HHS Office of Global Affairs.133 Since then, Secretary Azar has reportedly "told lawmakers that the administration has now spent or obligated the entirety of $105 million [from the IDRRRF] and is now moving into previously announced transfers of $136 million from other programs."134
CDC has an additional source of emergency support through the CDC Foundation, a 501(c)(3) public charity established by Congress "to support and carry out activities for the prevention and control of diseases, disorders, injuries, and disabilities, and for promotion of public health."135 The CDC Foundation activated its Emergency Response Fund (ERF) to support COVID-19 response on January 27, 2020, as requested by CDC.136 Funds have been donated to the ERF for this response by the Robert Wood Johnson Foundation, among others. Although the support provided by the foundation for outbreak response has been modest compared with supplemental appropriations, the foundation has greater spending flexibility and can sometimes procure response supplies and services more quickly than CDC through federal procurement processes.137
On February 24, 2020, the Administration asked Congress for an emergency supplemental appropriation of $1.25 billion for COVID-19 response efforts. The Administration also asked Congress to allow re-purposing of another $1.25 billion in existing funds from across the government, including HHS funds for current Ebola response activities.138 It is reported that "House and Senate appropriators are discussing a package in the range of $6 billion to $8 billion … [for] the departments of Health and Human Services, State, Homeland Security, Defense and possibly other agencies…."139
Author Contact Information
Acknowledgments
Edward C. Liu, Legislative Attorney, and Ben Harrington, Legislative Attorney, contributed to this report.
Footnotes
| 1. |
WHO, "Novel Coronavirus (COVID-19) Situation Reports," https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports; and U.S. Centers for Disease Control and Prevention (CDC), "Coronavirus Disease 2019 (COVID-19) Situation Summary," https://www.cdc.gov/coronavirus/COVID-19/summary.html. |
| 2. |
WHO, "Statement on the second meeting of the International Health Regulations (2005) Emergency Committee regarding the outbreak of novel coronavirus (COVID-19)," January 30, 2020, https://www.who.int/news-room/statements. The definition of and procedures for a PHEIC are at https://www.who.int/ihr/procedures/pheic/en/. See also CRS In Focus IF10022, The Global Health Security Agenda and International Health Regulations. |
| 3. |
U.S. Department of Health and Human Services (HHS), "Secretary Azar Declares Public Health Emergency for United States for Coronavirus Disease 2019," press release, January 31, 2020, https://www.hhs.gov/about/news/2020/01/31/secretary-azar-declares-public-health-emergency-us-2019-novel-coronavirus.html. |
| 4. |
CDC, "Coronavirus Disease 2019 (COVID-19) Situation Summary," updated February 25, 2020, https://www.cdc.gov/coronavirus/2019-ncov/summary.html#risk-assessment. |
| 5. |
Anthony S. Fauci, H. Clifford Lane, and Robert R. Redfield, "Covid-19–Navigating the Uncharted," New England Journal of Medicine, online editorial, February 28, 2020, https://www.nejm.org/doi/full/10.1056/NEJMe2002387. |
| 6. |
CDC, "Human Coronavirus Types," accessed February 4, 2020, https://www.cdc.gov/coronavirus/types.html. |
| 7. |
Kristian G. Andersen, Andrew Rambaut, and W. Ian Lipkin, "The Proximal Origin of SARS-CoV-2," Virological, pre-print, February 2020, virological.org/t/the-proximal-origin-of-sars-cov-2/398; and CDC, "Coronavirus Disease 2019 (COVID-19) Situation Summary," updated February 16, 2020, https://www.cdc.gov/coronavirus/COVID-19/summary.html. |
| 8. |
CDC, "Symptoms—Coronavirus Disease 2019," accessed February 18, 2020, https://www.cdc.gov/coronavirus/COVID-19/about/symptoms.html. |
| 9. |
Matthew Walsh and Han Wei, "Wuhan Virus Update: China Confirms Human-to-Human Transmission," Caixin Global, January 21, 2020, https://www.caixinglobal.com/2020-01-21/wuhan-virus-update-china-confirms-human-to-human-transmission-101506555.html. |
| 10. |
CDC, "How COVID-19 Spreads," accessed February 18, 2020, https://www.cdc.gov/coronavirus/2019-ncov/about/transmission.html. |
| 11. |
WHO states that "Current estimates of the incubation period range from 1-12.5 days with median estimates of 5-6 days. These estimates will be refined as more data become available. Based on information from other coronavirus diseases, such as MERS and SARS, the incubation period of 2019-nCoV could be up to 14 days. WHO recommends that the follow-up of contacts of confirmed cases is 14 days." from WHO, "Q&A on Coronaviruses," February 11, 2020, https://www.who.int/news-room/q-a-detail/q-a-coronaviruses. |
| 12. |
CDC, "Transcript for CDC Media Telebriefing: Update on COVID-19," February 14, 2020, https://www.cdc.gov/media/releases/2020/t0214-covid-19-update.html.html. |
| 13. |
Ibid. |
| 14. |
Ibid, and WHO, "Q&A on Coronaviruses," February 11, 2020, https://www.who.int/news-room/q-a-detail/q-a-coronaviruses. |
| 15. |
CDC, "Coronavirus Disease 2019: Information for Healthcare Professionals," https://www.cdc.gov/coronavirus/COVID-19/hcp/index.html. |
| 16. |
CRS Report R40554, The 2009 Influenza Pandemic: An Overview. |
| 17. |
CDC, "Pandemic Preparedness Resources," February 15, 2020, https://www.cdc.gov/coronavirus/2019-ncov/php/pandemic-preparedness-resources.html. |
| 18. |
CDC, "Legal Authorities for Isolation and Quarantine," https://www.cdc.gov/quarantine/aboutlawsregulationsquarantineisolation.html. |
| 19. |
CDC, "Selected Federal Legal Authorities Pertinent to Public Health Emergencies," August 2017, https://www.cdc.gov/phlp/docs/ph-emergencies.pdf. |
| 20. |
Interstate Quarantine regulations: 42 C.F.R. Part 70, and Foreign Quarantine regulations: 42 C.F.R. Part 71. |
| 21. |
8 U.S.C. Chapter 12. |
| 22. |
CDC, "Evaluating and Reporting Persons Under Investigation (PUI)," updated February 27, 2020, |
| 23. |
Anita Patel, Daniel B. Jernigan, and 2019 n-CoV CDC Response Team, "Initial Public Health Response and Interim Clinical Guidance for the Coronavirus Disease 2019 Outbreak—United States, December 31, 2019–February 4, 2020," Morbidity and Mortality Weekly Report (MMWR), vol. 69 (February 5, 2020). |
| 24. |
Current guidance is compiled at CDC, "Information for Healthcare Professionals," https://www.cdc.gov/coronavirus/2019-ncov/hcp/index.html; and "Resources for State, Local, Territorial and Tribal Health Departments," https://www.cdc.gov/coronavirus/2019-ncov/php/index.html. |
| 25. |
Chaolin Huang, Yeming Wang, Xingwang Li, et al., "Clinical Features of Patients Infected with Coronavirus Disease 2019 in Wuhan, China," The Lancet, January 24, 2020. |
| 26. |
CDC, "Transcript of Coronavirus Disease 2019 (COVID-19) Update," January 27, 2020, https://www.cdc.gov/media/releases/2020/t0127-coronavirus-update.html. |
| 27. |
CDC, "Coronavirus Disease 2019 (COVID-19) Situation Summary," updated February 29, 2020, https://www.cdc.gov/coronavirus/COVID-19/summary.html. |
| 28. |
Andrew Selsky, "Washington Governor Declares State of Emergency Over Virus," February 29, 2020, https://abcnews.go.com/US/wireStory/coronavirus-cases-unknown-origin-found-west-coast-69301250. |
| 29. |
Alex Horton and William Wan, "Coronavirus Shuts Down Two Public Schools as Districts Race to Contain the Spread," Washington Post, February 29, 2020. |
| 30. |
CDC, "Coronavirus Disease 2019 (COVID-19) Situation Summary," updated February 20, 2020, https://www.cdc.gov/coronavirus/COVID-19/summary.html. |
| 31. |
Stanley L. Inhorn, J. Rex Astiles, and Vanessa A. White, "The State Public Health Laboratory System," Public Health Reports, vol. 125, no. Suppl 2 (2010), pp. 4-17. |
| 32. |
Association of Public Health Laboratories, "About Public Health Laboratories," https://www.aphl.org/aboutAPHL/Pages/aboutphls.aspx. |
| 33. |
CDC, "Coronavirus Disease 2019 (COVID-2019) Situation Summary," updated February 3, 2020, https://www.cdc.gov/coronavirus/COVID-2019/summary.html. |
| 34. |
Reverse transcriptase-polymerase chain reaction (RT-PCR) is a very sensitive technique that, in this use, allows the detection of otherwise undetectably low amounts of biological components specific to coronavirus. |
| 35. |
CDC, "CDC Tests for COVID-19," accessed February 18, 2020, https://www.cdc.gov/coronavirus/2019-ncov/about/testing.html; and Centers for Medicare & Medicaid Services (CMS), Clinical Laboratory Improvement Amendments (CLIA), https://www.cms.gov/Regulations-and-Guidance/Legislation/CLIA. |
| 36. |
CDC, "Laboratory Response Network for Biological Threats (LRN-B)," accessed February 18, 2020, https://emergency.cdc.gov/lrn/biological.asp. |
| 37. |
CDC "Media Telebriefing: Update on Coronavirus Disease 2019 (COVID-2019)," February 5, 2020, https://www.cdc.gov/media/releases/2020/a0205-cdc-telebriefing-coronavirus-update.html. |
| 38. |
CDC, "CDC Tests for COVID-19," accessed February 18, 2020, https://www.cdc.gov/coronavirus/2019-ncov/about/testing.html; and CDC, "Transcript for CDC Telebriefing: CDC Update on Novel Coronavirus," February 12, 2020, https://www.cdc.gov/media/releases/2020/t0212-cdc-telebriefing-transcript.html. |
| 39. |
CDC, "COVID-19 Situation Summary," February 29, 2020, https://www.cdc.gov/coronavirus/2019-ncov/summary.html; and Rob Stein, "CDC Has Fixed Issue Delaying Coronavirus Testing In U.S., Health Officials Say," National Public Radio, February 27, 2020, https://www.npr.org/sections/health-shots/2020/02/27/809936132/cdc-fixes-issue-delaying-coronavirus-testing-in-u-s. |
| 40. |
International Reagent Resource, https://www.internationalreagentresource.org/. |
| 41. |
The travel restrictions for China became effective on February 2, 2020, and for Iran, March 2, 2020. The White House, Remarks by President Trump, Vice President Pence, and Members of the Coronavirus Task Force in Press Conference, February 29, 2020, https://www.whitehouse.gov/briefings-statements/remarks-president-trump-vice-president-pence-members-coronavirus-task-force-press-conference-2/. |
| 42. |
Although the incubation period for COVID-19 has not yet been established, the U.S. Centers for Disease Control and Prevention (CDC) advises that "[f]or COVID-19, the period of quarantine is 14 days from the last date of exposure because 14 days is the longest incubation period seen for similar coronaviruses." Centers for Disease Control and Prevention, "Coronavirus Disease 2019 (COVID-19)," updated February 15, 2020, https://www.cdc.gov/coronavirus/2019-ncov/faq.html. |
| 43. |
Centers for Disease Control and Prevention, Travelers from Countries with Widespread Sustained (Ongoing) Transmission Arriving in the United States, accessed March 4, 2020, https://www.cdc.gov/coronavirus/2019-ncov/travelers/after-travel-precautions.html. |
| 44. |
The White House, "Proclamation on Suspension of Entry as Immigrants and Nonimmigrants of Persons Who Pose a Risk of Transmitting 2019 Novel Coronavirus," January 31, 2020, https://www.whitehouse.gov/presidential-actions/proclamation-suspension-entry-immigrants-nonimmigrants-persons-pose-risk-transmitting-2019-novel-coronavirus/ [hereinafter China Proclamation]. |
| 45. |
The White House, "Proclamation on Suspension of Entry as Immigrants and Nonimmigrants of Persons Who Pose a Risk of Transmitting 2019 Novel Coronavirus," February 29, 2020, https://www.whitehouse.gov/presidential-actions/proclamation-suspension-entry-immigrants-nonimmigrants-certain-additional-persons-pose-risk-transmitting-coronavirus/ [hereinafter Iran Proclamation]. |
| 46. |
Id. |
| 47. |
8 U.S.C. §1182(f). |
| 48. |
Id. |
| 49. |
Trump v. Hawaii, 138 S. Ct. 2392, 2408 (2018). |
| 50. |
China Proclamation, supra note 43, §5; Iran Proclamation, supra note 44, §5. |
| 51. |
China Proclamation, supra note 43, §5, as amended by Iran Proclamation, supra note 44, §4(c). |
| 52. |
Id. |
| 53. |
U.S. Department of Homeland Security (DHS), "DHS Issues Supplemental Instructions for Inbound Flights with Individuals Who Have Been in China," press release, February 2, 2020, https://www.dhs.gov/news/2020/02/02/dhs-issues-supplemental-instructions-inbound-flights-individuals-who-have-been-china, and U.S. Customs and Border Protection, "Notification of Arrival Restrictions Applicable to Flights Carrying Persons Who Have Recently Traveled From or Were Otherwise Present Within the People's Republic of China or the Islamic Republic of Iran," 85 Federal Register 12731-12733, March 4, 2020. |
| 54. |
42 U.S.C. §264. See "Domestic Quarantine and Isolation: Legal Authority and Policies," in CRS Report R43809, Preventing the Introduction and Spread of Ebola in the United States: Frequently Asked Questions; and CDC, "Legal Authorities for Isolation and Quarantine," updated February 20, 2020, https://www.cdc.gov/quarantine/aboutlawsregulationsquarantineisolation.html. |
| 55. |
CDC, Division of Global Migration and Quarantine (DGMQ), https://www.cdc.gov/ncezid/dgmq/index.html. |
| 56. |
CDC, "2019 Novel Coronavirus: Travelers from China Arriving in the United States," https://www.cdc.gov/coronavirus/2019ncov/travelers/from-china.html. |
| 57. |
DHS, "DHS Issues Supplemental Instructions for Inbound Flights with Individuals Who Have Been in China," press release, February 2, 2020, https://www.dhs.gov/news/2020/02/02/dhs-issues-supplemental-instructions-inbound-flights-individuals-who-have-been-china. |
| 58. |
Centers for Disease Control and Prevention, Travelers from Countries with Widespread Sustained (Ongoing) Transmission Arriving in the United States, accessed March 4, 2020, https://www.cdc.gov/coronavirus/2019-ncov/travelers/after-travel-precautions.html. |
| 59. |
Stephanie Soucheray, "CDC Quarantines 195 Passengers; U.S. Declares nCoV Public Health Emergency," CIDRAP News, January 31, 2020, http://www.cidrap.umn.edu/news-perspective/2020/01/cdc-quarantines-195-passengers-us-declares-ncov-public-health-emergency. |
| 60. |
CDC, "Importation," https://www.cdc.gov/importation/index.html. |
| 61. |
For a discussion, see "Domestic Quarantine and Isolation: Legal Authority and Policies" in CRS Report R43809, Preventing the Introduction and Spread of Ebola in the United States: Frequently Asked Questions. |
| 62. |
HHS, "Secretary Azar Declares Public Health Emergency for United States for 2019 Novel Coronavirus," press release, January 31, 2020. |
| 63. |
Department of Homeland Security, "Notification of Arrival Restrictions Applicable to Flights Carrying Persons Who Have Recently Traveled From or Were Otherwise Present within the People's Republic of China," 85 Federal Register 7214-7215, February 7, 2020. [hereinafter Notification of Arrival Restrictions]. |
| 64. |
Hollie Silverman, "Travelers Will Face New Restrictions and Cancellations as Coronavirus Cases Grow in the US," CNN, March 2, 2020. |
| 65. |
Notification of Arrival Restrictions, February 7, 2020. |
| 66. |
Department of Homeland Security, "Notification of Arrival Restrictions Applicable to Flights Carrying Persons Who Have Recently Traveled From or Were Otherwise Present within the People's Republic of China," 85 Federal Register 7214-7215, February 7, 2020. [hereinafter Notification of Arrival Restrictions]. |
| 67. |
Hollie Silverman, "Travelers Will Face New Restrictions and Cancellations as Coronavirus Cases Grow in the US," CNN, March 2, 2020. |
| 68. |
Id. |
| 69. |
U.S. Department of State, "Evacuation of Americans from Wuhan, China," Press Statement, February 8, 2020, https://www.state.gov/evacuation-of-americans-from-wuhan-china-2/. See also Department of State, "On the Repatriation of U.S. Citizens from the Princess Diamond Cruise Ship," Special Briefing, February 17, 2020, https://www.state.gov/on-the-repatriation-of-u-s-citizens-from-the-princess-diamond-cruise-ship/. |
| 70. |
Daniel B. Jernigan, MD and CDC COVID-19 Response Team, "Update: Public Health Response to Coronavirus Disease 2019 Outbreak—United States, February 24, 2020," Morbidity and Mortality Weekly Report, vol. 69, no. 8 (February 25, 2020), https://www.cdc.gov/mmwr/volumes/69/wr/mm6908e1.htm. |
| 71. |
The U.S. Public Health Service Commissioned Corps and the National Disaster Medical System are described in CRS Report R43560, Deployable Federal Assets Supporting Domestic Disaster Response Operations: Summary and Considerations for Congress. |
| 72. |
CDC, "Coronavirus Disease 2019 (COVID-19), Travel: Frequently Asked Questions and Answers," accessed February 21, 2020, https://www.cdc.gov/coronavirus/2019-ncov/travelers/faqs.html. |
| 73. |
See, for example, World Health Organization (WHO), "No Rationale for Travel Restrictions," May 1, 2009, in the context of the 2009 H1N1 influenza pandemic, https://www.who.int/csr/disease/swineflu/guidance/public_health/travel_advice/en/. |
| 74. |
WHO, "Updated WHO Advice for International Traffic in Relation to the Outbreak of the Novel Coronavirus 2019-nCoV," January 27, 2020, https://www.who.int/ith/2019-nCoV_advice_for_international_traffic/en/. |
| 75. |
WHO, "Key Considerations for Repatriation and Quarantine of Travellers in Relation to the Outbreak of Novel Coronavirus 2019-nCoV," February 11, 2020, https://www.who.int/emergencies/diseases/novel-coronavirus-2019/travel-advice. |
| 76. |
Michael Levenson, "Scale of China's Wuhan Shutdown Is Believed to Be without Precedent," The New York Times, January 22, 2020. Wuhan is the capital of Hubei Province in mainland China. |
| 77. |
Several such studies are discussed in Julia Belluz and Steven Hoffman, "The evidence on travel bans for diseases like coronavirus is clear: They don't work," Vox, January 23, 2020, https://www.vox.com/2020/1/23/21078325/wuhan-china-coronavirus-travel-ban. |
| 78. |
Sukhyun Ryu, Huizhi Gao, Jessica Y. Wong, et al., "Nonpharmaceutical Measures for Pandemic Influenza in Nonhealthcare Settings—International Travel-Related Measures," Emerging Infectious Diseases, vol. 26, no. 5 (May 2020). |
| 79. |
Francesca Matthews Pillemer et al., "Predicting Support for Non-pharmaceutical Interventions during Infectious Outbreaks: A Four Region Analysis," Disasters, vol. 39, no. 1, pp. 125-145, January 2015, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4355939/. |
| 80. |
CDC. "History of Quarantine," https://www.cdc.gov/quarantine/historyquarantine.html. |
| 81. |
Min W. Fong, Huizhi Gao, and Jessica Y. Wong, "Nonpharmaceutical Measures for Pandemic Influenza in Nonhealthcare Settings—Social Distancing Measures," Emerging Infectious Diseases, pre-print, vol. 26, no. 5 (May 2020). |
| 82. |
FDA, "What Are Medical Countermeasures?" accessed February 4, 2020, https://www.fda.gov/emergency-preparedness-and-response/about-mcmi/what-are-medical-countermeasures. |
| 83. |
FDA, "Novel coronavirus (2019-nCoV)," accessed February 4, 2020, https://www.fda.gov/emergency-preparedness-and-response/mcm-issues/novel-coronavirus-2019-ncov; and FDA, "Coronavirus (COVID-19) Update: FDA Issues New Policy to Help Expedite Availability of Diagnostics," press release with link to guidance, February 29, 2020, https://www.fda.gov/news-events/press-announcements/coronavirus-covid-19-update-fda-issues-new-policy-help-expedite-availability-diagnostics. |
| 84. |
FDA, "FDA Takes Significant Step in Coronavirus Response Efforts, Issues Emergency Use Authorization for the First 2019 Novel Coronavirus Diagnostic," February 4, 2020, https://www.fda.gov/news-events/press-announcements/fda-takes-significant-step-coronavirus-response-efforts-issues-emergency-use-authorization-first. |
| 85. |
GenomeWeb, "FDA Provides SARS-CoV-2 Test Validation Guidance for High-Complexity Labs Seeking EUA," March 3, 2020, https://www.genomeweb.com/pcr/fda-provides-sars-cov-2-test-validation-guidance-high-complexity-labs-seeking-eua#.Xl7JFqhKiUk; and FDA, "Policy for Diagnostics Testing in Laboratories Certified to Perform High Complexity Testing under CLIA prior to Emergency Use Authorization for Coronavirus Disease-2019 during the Public Health Emergency," February 29, 2020, https://www.fda.gov/media/135659/download. |
| 86. |
FDA, "Coronavirus (COVID-19) Update: FDA Issues New Policy to Help Expedite Availability of Diagnostics," press release with link to guidance, February 29, 2020, https://www.fda.gov/news-events/press-announcements/coronavirus-covid-19-update-fda-issues-new-policy-help-expedite-availability-diagnostics. See also CRS In Focus IF11389, FDA Regulation of Laboratory-Developed Tests (LDTs). |
| 87. |
HHS Representative, White House Coronavirus Task Force news conference, January 31, 2020, https://plus.cq.com/doc/newsmakertranscripts-5826415. |
| 88. |
HHS, "HHS Seeks Abstract Submissions for 2019-nCoV Diagnostics Development," press release, February 5, 2020, https://www.hhs.gov/about/news/2020/02/05/hhs-seeks-abstract-submissions-for-2019-ncov-diagnostics-development.html. |
| 89. |
Hilary Marston, NIAID, "2019 Novel Coronavirus Stakeholder Listening Session Transcript," January 30, 2020, https://www.phe.gov/Preparedness/nCoV/Documents/2019nCoV-Listening-Session-Transcript.pdf. |
| 90. |
HHS, "HHS, Regeneron Collaborate to Develop 2019-nCoV Treatment," February 4, 2020, https://www.hhs.gov/about/news/2020/02/04/hhs-regeneron-collaborate-to-develop-2019-ncov-treatment.html; and HHS, "HHS, Janssen Collaborate to Develop Coronavirus Therapeutics," February, 18, 2020, https://www.hhs.gov/about/news/2020/02/18/hhs-janssen-collaborate-to-develop-coronavirus-therapeutics.html. |
| 91. |
Guangdi Li and Erik De Clercq, "Therapeutic options for the 2019 novel coronavirus (2019-nCoV)," Nature Reviews: Drug Discovery, February 10, 2020, https://www.nature.com/articles/d41573-020-00016-0. |
| 92. |
Jared Hopkins, "U.S. Drugmakers Ship Therapies to China, Seeking to Treat Coronavirus," Wall Street Journal, January 27, 2020. |
| 93. |
Ibid. |
| 94. |
Guangdi Li and Erik De Clercq, "Therapeutic options for the 2019 novel coronavirus (2019-nCoV)," Nature Reviews: Drug Discovery, February 10, 2020, https://www.nature.com/articles/d41573-020-00016-0. |
| 95. |
Gilead, "Gilead Sciences Statement on the Company's Ongoing Response to the 2019 Novel Coronavirus (2019-nCoV)," January 31, 2020, https://www.gilead.com/news-and-press/company-statements/gilead-sciences-statement-on-the-company-ongoing-response-to-the-2019-new-coronavirus. |
| 96. |
NIH, "NIH clinical trial of remdesivir to treat COVID-19 begins," February 25, 2020, https://www.nih.gov/news-events/news-releases/nih-clinical-trial-remdesivir-treat-covid-19-begins. |
| 97. |
Steve Usdin and Karen Tkach Tuzman, "The Race Is on to Develop Therapies and Vaccines for the Coronavirus Outbreak," Biocentury, January 24, 2020, https://www.biocentury.com/article/304290/the-coronavirus-outbreak-is-creating-a-testbed-for-new-vaccine-and-therapeutic-technologies. |
| 98. |
Moderna, "Moderna Announces Funding Award from CEPI to Accelerate Development of Messenger RNA (mRNA) Vaccine Against Novel Coronavirus," January 23, 2020, https://investors.modernatx.com/news-releases/news-release-details/moderna-announces-funding-award-cepi-accelerate-development. |
| 99. |
Coalition for Epidemic Preparedness Innovations, "CEPI and GSK announce collaboration to strengthen the global effort to develop a vaccine for the 2019-nCoV virus," February 3, 2020, https://cepi.net/news_cepi/cepi-and-gsk-announce-collaboration-to-strengthen-the-global-effort-to-develop-a-vaccine-for-the-2019-ncov-virus/. |
| 100. |
HHS, "HHS Engages Sanofi's Recombinant Technology for 2019 Novel Coronavirus Vaccine," February 18, 2020, https://www.hhs.gov/about/news/2020/02/18/hhs-engages-sanofis-recombinant-technology-for-2019-novel-coronavirus-vaccine.html; and HHS, "HHS, Janssen Join Forces On Coronavirus Vaccine," February, 11, 2020, https://www.hhs.gov/about/news/2020/02/11/hhs-janssen-join-forces-on-coronavirus-vaccine.html. |
| 101. |
Cormac Sheridan, "Coronavirus and the Race to Distribute Reliable Diagnostics," Nature Biotechnology, February 21, 2020. |
| 102. |
Peter Loftus, "Drugmaker Moderna Delivers First Experimental Coronavirus Vaccine for Human Testing," Wall Street Journal, February 24, 2007. |
| 103. |
HHS, Encouraging Vaccine Innovation: Promoting the Development of Vaccines that Minimize the Burden of Infectious Diseases in the 21st Century, Report to Congress, December 2017, https://www.hhs.gov/sites/default/files/encouraging_vaccine_innovation_2018_final_report.pdf. |
| 104. |
Hanna Ziady, "Biotech Company Moderna Says its Coronavirus Vaccine is Ready for First Tests," CNN Business, February 26, 2020, https://www.cnn.com/2020/02/25/business/moderna-coronavirus-vaccine/index.html. |
| 105. |
Matthew Herper and Damien Garde, "Coronavirus Vaccines Are Far Off, FDA Official Says, But Drugs to Treat Patients Could Come Sooner," STAT, February 26, 2020, https://www.statnews.com/2020/02/26/coronavirus-vaccines-are-far-off-fda-official-says-but-drugs-to-treat-patients-could-come-sooner/. |
| 106. |
21 U.S.C. §360bbb-3. For additional information, see CRS In Focus IF10745, Emergency Use Authorization and FDA's Related Authorities. |
| 107. |
21 U.S.C. §360bbb-3(b)(1). |
| 108. |
21 U.S.C. §360bbb-3(c). |
| 109. |
This determination, made pursuant to Section 564(b)(1)(C) of the Federal Food, Drug, and Cosmetic Act (21 U.S.C. §360bbb-3(b)(1)(C)), is noted on page 1 of the letter of authorization from FDA to CDC, advising of the authorization for emergency use of the CDC-developed diagnostic test. This letter is available at "Novel coronavirus (COVID-2019) EUA Information" on the FDA web page "Emergency Use Authorization," https://www.fda.gov/emergency-preparedness-and-response/mcm-legal-regulatory-and-policy-framework/emergency-use-authorization. See also footnote 84. |
| 110. |
FDA, "Coronavirus (COVID-19) Update: FDA and CDC take action to increase access to respirators, including N95s, for health care personnel," March 2, 2020, https://www.fda.gov/news-events/press-announcements/coronavirus-covid-19-update-fda-and-cdc-take-action-increase-access-respirators-including-n95s. The letter of authorization from FDA to CDC, advising of the authorization for emergency use of certain eligible respirators is available at "Novel coronavirus (COVID-2019) EUA Information" on the FDA web page "Emergency Use Authorization," https://www.fda.gov/emergency-preparedness-and-response/mcm-legal-regulatory-and-policy-framework/emergency-use-authorization. |
| 111. |
HHS, "Coronavirus Disease 2019," https://www.phe.gov/Preparedness/nCoV/Pages/default.aspx. See also CRS Insight IN11038, U.S. National Health Security: Homeland Security Issues in the 116th Congress. |
| 112. |
CDC, Public Health Emergency Preparedness (PHEP) Cooperative Agreement, https://www.cdc.gov/cpr/readiness/phep.htm; and HHS, Assistant Secretary for Preparedness and Response (ASPR), Hospital Preparedness Program (HPP), https://www.phe.gov/Preparedness/planning/hpp/Pages/default.aspx. |
| 113. |
CDC, "Public Health Emergency Preparedness and Response Capabilities," p. 103, October 2018, Updated January 2019, https://www.cdc.gov/cpr/readiness/capabilities.htm, hereinafter "CDC Capabilities 2019." |
| 114. |
HHS, "HPP Funds Regional Treatment Network for Ebola and Other Special Pathogens," https://www.phe.gov/Preparedness/planning/hpp/Pages/hpp-pathogens.aspx. |
| 115. |
CDC Capabilities 2019, p. 112. |
| 116. |
Ibid, p. 80. |
| 117. |
HHS, "Strategic National Stockpile, https://www.phe.gov/about/sns/Pages/default.aspx." |
| 118. |
National Health Security Preparedness Index (NHSPI), https://nhspi.org/. |
| 119. |
NHSPI Frequently Asked Questions, 2019, https://nhspi.org/?s=FAQs. |
| 120. |
Robert Kadlec, HHS Assistant Secretary for Preparedness and Response (ASPR), "Coronavirus Disease 2019 Stakeholder Listening Session Transcript," January 30, 2020, https://www.phe.gov/Preparedness/nCoV/Documents/2019nCoV-Listening-Session-Transcript.pdf; CDC, "CDC Update on Novel Coronavirus," February 5, 2020, https://www.cdc.gov/media/releases/2020/t0205-coronavirus-update.html; and FDA, "FDA's Actions in Response to 2019 Novel Coronavirus at Home and Abroad," February 14, 2020, https://www.fda.gov/news-events/press-announcements/fdas-actions-response-2019-novel-coronavirus-home-and-abroad. |
| 121. |
Robert Kadlec, HHS Assistant Secretary for Preparedness and Response (ASPR), "Coronavirus Disease 2019 Stakeholder Listening Session Transcript," January 30, 2020, https://www.phe.gov/Preparedness/nCoV/Documents/2019nCoV-Listening-Session-Transcript.pdf; and CDC, "CDC Update on Novel Coronavirus," February 5, 2020, https://www.cdc.gov/media/releases/2020/t0205-coronavirus-update.html. |
| 122. |
21 U.S.C. §356c(a). |
| 123. |
21 U.S.C. §356c(g), 21 U.S.C. §381(d). |
| 124. |
FDA, "Coronavirus Update: FDA steps to ensure quality of foreign products," February 24, 2020, https://www.fda.gov/news-events/press-announcements/coronavirus-update-fda-steps-ensure-quality-foreign-products. |
| 125. |
FDA, "FDA's Actions in Response to 2019 Novel Coronavirus at Home and Abroad," February 14, 2020, https://www.fda.gov/news-events/press-announcements/fdas-actions-response-2019-novel-coronavirus-home-and-abroad. |
| 126. |
FDA, Testimony of Dr. Janet Woodcock, Director the Center for Drug Evaluation and Research, "Securing the U.S. Drug Supply Chain: Oversight of FDA's Foreign Inspection Program," December 10, 2019, https://www.fda.gov/news-events/congressional-testimony/securing-us-drug-supply-chain-oversight-fdas-foreign-inspection-program-12102019. |
| 127. |
Annual appropriations acts give the HHS Secretary limited authority to transfer funds from one budget account to another within the department. For instance, a provision in the FY2020 HHS appropriations act (P.L. 116-94, Division A, Title II, §205) generally allows the Secretary to transfer up to 1% of the funds from any given account. However, in general, a recipient account may not be increased by more than 3%. Congressional appropriators must be notified in advance of any transfer. Another FY2020 appropriations provision (P.L. 116-94, Division A, Title V, §514) addresses the Secretary's authority to reprogram funds from one program, project, or activity in a given budget account to a different program, project, or activity within the same budget account. This provision places certain limits on such actions and clarifies the circumstances in which appropriations committees must be consulted in advance. (See P.L. 115-245.) |
| 128. |
See HHS, "Legal Authority with Declaration of Public Health Emergency," https://www.phe.gov/Preparedness/support/secauthority/Pages/default.aspx#phe. |
| 129. |
Rebecca Katz, Aurelia Attal-Juncqua, and Julie E. Fischer, "Funding Public Health Emergency Preparedness in the United States," American Journal of Public Health, vol. 107, suppl. 2, pp. S148-S152, September, 2017, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5594396/. |
| 130. |
The IDRRRF authority is codified at 42 U.S.C. §247d-4a. |
| 131. |
CQ Newsmaker Transcripts, "Health and Human Services Secretary Azar Holds News Conference on Coronavirus," January 28, 2020, https://plus.cq.com/doc/newsmakertranscripts-5822133?8&searchId=XGVQS7c5. |
| 132. |
Communication with CDC, January 28, 2020. |
| 133. |
Yasmeen Abutaleb and Erica Werner, "HHS Notifies Congress that it May Tap Millions of Additional Dollars for Coronavirus Response," Washington Post, February 3, 2020. Likely the authority described in footnote 127. |
| 134. |
Erica Werner and Yasmeen Abutaleb, "Congressional Leaders Launch Emergency Spending Talks for Coronavirus Response," Washington Post, February 26, 2020. |
| 135. |
Public Health Service Act Section 399G, 42 U.S.C. §280e–11. See "National Foundation for the Centers for Disease Control and Prevention" in CRS Report R46109, Agency-Related Nonprofit Research Foundations and Corporations. |
| 136. |
CDC Foundation, "Responding to Coronavirus," https://www.cdcfoundation.org/coronavirus. |
| 137. |
See, for example, CDC Foundation, "2018 Ebola Outbreak," https://www.cdcfoundation.org/2018-ebola-outbreak. |
| 138. |
Russell T. Vought, Acting Director, White House Office of Management and Budget, letter to the Honorable Michael R. Pence, President of the Senate, February 24, 2020. |
| 139. |
Paul M. Krawzak, "Lawmakers Zeroing in on $6B to $8B Coronavirus Aid Package," CQ News, February 27, 2020. |