Ebola Outbreaks in the Democratic Republic of Congo: Emergencies or Enduring Threat?
Changes from September 27, 2019 to September 10, 2020
This page shows textual changes in the document between the two versions indicated in the dates above. Textual matter removed in the later version is indicated with red strikethrough and textual matter added in the later version is indicated with blue.
Contents
- Introduction
- The International Response
- DRC Government Role
- U.N. and Other Multilateral Organizations
- The U.S. Government Response
- Challenges
- Security Threats and Political Tensions
- Health System Constraints
- Reported Progress
- Issues for Congress
- U.S. Funding for DRC Ebola Response
- U.S. Aid Restrictions Related to Trafficking in Persons
- Global Health Security
Figures
Summary
The Ebola outbreak in the Democratic Republic of Congo (DRC) that began in August 2018 has eluded international containment efforts and posed significant challenges to local and international policymakers. The current outbreak is the 10th and largest on record in DRC, and the world's second largest ever (after the 2014-2016 West Africa outbreak). On July 17, 2019, the World Health Organization (WHO) declared the current DRC outbreak to be a Public Health Emergency of International Concern (PHEIC) and called for increased donor funding. To date, the U.S. Agency for International Development (USAID) has announced nearly $158 million to support the response to the outbreak in DRC and neighboring countries, most of which has been funded through USAID-administered International Disaster Assistance (IDA) funds appropriated by Congress in FY2015.
Challenges
Broad challenges in DRC—including unresolved armed conflicts, shortfalls in the local health care system, political tensions, community grievances, and criminal activities—have hindered outbreak control. The main outbreak zone is an area of eastern DRC where long-running conflicts had already caused a protracted humanitarian crisis. In addition, the outbreak has coincided with a fraught political transition process in DRC, where a former opposition figure, Felix Tshisekedi, was inaugurated president in January 2019. The electoral process and tense negotiations over a coalition government have complicated Ebola response efforts, as well as coordination between national and provincial officials. Ebola and related response efforts have also diverted or interrupted already limited local health resources in affected areas. This phenomenon, in turn, has been linked to interruptions in routine immunization campaigns. Inadequate measles vaccine supplies have limited capacity to control a measles outbreak in DRC that began in January 2019 and has claimed more than 3,000 lives.
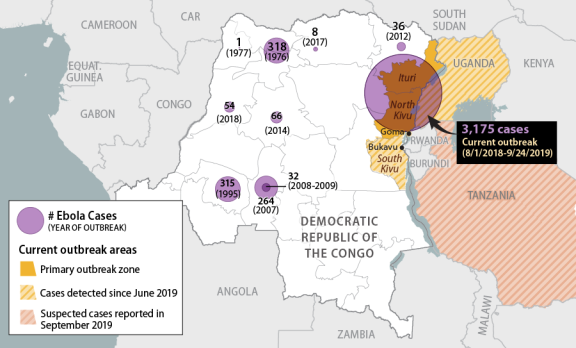
Since June 2019, a handful of Ebola-infected individuals have been identified in the large city of Goma in eastern DRC (a staging area for humanitarian operations and U.N. peacekeeping activities in the country), in the city of Bukavu (south of the main outbreak zone), and in Uganda. Suspected cases were reported, but not confirmed, in Tanzania in mid-September 2019. Transmission outside the outbreak zone has been limited to date, which may be attributable to internationally supported surveillance and prevention efforts, as well as the use of an investigational vaccine. Concerns nevertheless persist that cases could spread to new areas and/or countries. Uganda (which borders the most affected areas in DRC) has prior experience in Ebola control, but Rwanda, Tanzania, and Burundi do not. Minimal state capacity and protracted conflict in South Sudan and the Central African Republic suggest that a coordinated disease control response in either setting could be highly challenging.
Issues for Congress
A potential issue for Congress is the level of funding allocated for global health security and pandemic preparedness versus outbreak response, with funding for outbreak response to date outweighing support for global outbreak prevention. Separately, the State Department's designation of DRC as a "Tier III" (worst-performing) country under the Trafficking Victims Protection Act (TVPA, Division A of P.L. 106-386, as amended) triggers restrictions on certain types of U.S. aid (not including IDA-funded activities). Several bills would authorize U.S. funding for programs intended to lower community resistance and otherwise support Ebola control in DRC and neighboring states, "notwithstanding" the TVPA restrictions. These include S. 1340, the Ebola Eradication Act of 2019, which passed the Senate in September 2019; H.R. 3085, a House companion bill; and a Senate committee draft of the FY2020 Department of State, Foreign Operations, and Related Programs appropriations bill circulated on September 18, 2019. Some Members of Congress have also monitored State Department security policies that have restricted U.S. government experts' travel to and within the outbreak zone.
Introduction
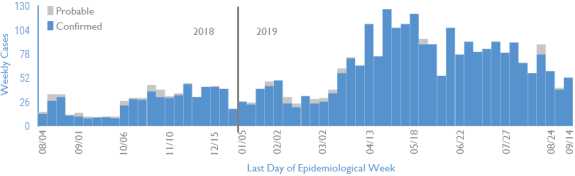
On August 1, 2018, the World Health Organization (WHO) reported a new Ebola outbreak in eastern DRC, about a week after having declared the end of a separate outbreak in the west of the country. As of September 24, 2019, the WHO had reported 3,175 cases in the current outbreak, including 2,119 deaths. About 58% of all cases have been women and 28% children.1 The current outbreak is the 10th on record in DRC, the largest to have occurred in the country, and the second largest ever, after the 2014-2016 Ebola outbreak in West Africa.2 Cases have been concentrated in North Kivu and Ituri provinces (Figure 1), where long-running conflicts had already caused a protracted humanitarian crisis and are complicating Ebola control efforts.3 The number of new Ebola cases identified per week has fluctuated since the start of the outbreak (Figure 2), but has generally trended downward slowly since peaking in April 2019.
|
 |
|
Sources: CRS graphic. Base map drawn from Esri (2016); data from the WHO, as of September 24, 2019. |
The current outbreak has coincided with a fraught political transition process in DRC. A new president, parliament, provincial-level assemblies, and governors were elected between late 2018 and mid-2019, after years of delays, gridlock, political violence, and repression of opposition voices. Election delays in the Ebola-affected areas, an opposition stronghold, heightened tensions and spurred conspiracy theories, arguably hindering Ebola response. President Felix Tshisekedi, inaugurated in January 2019, was previously an opposition figure, but the coalition of his predecessor Joseph Kabila won supermajorities in parliament and at the provincial level. Observers questioned the legitimacy of the election results, and tense negotiations between the two political blocs (Tshisekedi's and Kabila's) delayed the naming of a new cabinet until late August 2019, while complicating relations between the national and provincial/local officials.4
Several factors have foiled outbreak control efforts, including low Ebola awareness (early symptoms are similar to other common ailments like malaria), community distrust of health interventions, belated visits to health facilities (at which point survival prospects decline rapidly), and infection prevention control lapses in health facilities. Attacks by militia and criminal groups, political protests, health worker strikes, and security force abuses have also disrupted and impeded the response. In mid-September, for example, violent attacks in a new hotspot (Lwemba, Ituri Province) after the death of a local healthcare worker from Ebola prompted the indefinite suspension of Ebola control activities in the area.5 As a result, new cases continue to stem from unknown chains of transmission, and deaths continue to occur outside Ebola treatment centers.
As of September 14, 2019 |
 |
|
Source: Adapted by CRS from WHO, RD Congo-Ituri et Nord-Kivu: Tableau de bord de l'état de la riposte de la MVE (Semaine 37: du 09 au 15 Septembre 2019), September 20, 2019. Note: Figures in later weeks are subject to delays in case confirmation and reporting, as well as data cleaning. |
U.S. officials and other health experts have repeatedly raised concerns about broader challenges in DRC related to its health care system, political tensions, local grievances, and instability.6 USAID Administrator Mark Green testified to Congress in April 2019 that in DRC, "You have a failed democracy in many, many ways…. It will take more than simply a medical approach. It will take a development approach to try to tackle this terrible disease and to contain its outbreak."7 After traveling to DRC in August 2019, Administrator Green wrote, "Decades of corrupt, authoritarian rule during which communities were denied any meaningful voice in their government have undermined the Congolese people's trust in institutions."8
Health experts have been troubled by reports of Ebola cases in major DRC cities (including the capital of North Kivu, Goma) and outside of DRC. Between June and August 2019, a total of four cross-border cases were detected in Uganda. Observers expressed optimism about the rapid detection and containment of these cases, but new concerns have arisen about subsequent suspected cases in Tanzania. In mid-September, WHO was informed by unofficial sources of a number of suspected Ebola cases in that country, including in the capital city of Dar es Salaam, while Tanzanian authorities asserted that there were no confirmed or suspected Ebola cases in the country.9 WHO has reportedly since sent personal protective equipment (PPE) and vaccination supplies to Tanzania, and recommended that the sickened patients (one of whom reportedly died) receive secondary confirmation testing at a WHO facility. As of September 21, none of the cases had received secondary confirmation. Ebola control in other neighboring countries such as South Sudan, Burundi, or Central Africa Republic, which have minimal state capacity and are affected by protracted conflicts and political crises, could be highly challenging if required.
The International Response
Outbreak control, treatment, and disease surveillance activities are being carried out primarily by DRC government employees (including health workers and frontline workers, who provide routine and essential services), as well as by international nongovernmental organizations, with U.N. agencies (including the WHO), other multilateral entities (including the World Bank), and foreign governments providing funding, expertise, coordination, and logistical assistance.
10, 2020 Congo: Emergencies or Enduring Threat? Tiaji Salaam-Blyther On June 25, 2020, the World Health Organization (WHO) announced the end to an Specialist in Global Health Ebola outbreak that began nearly two years earlier in eastern Democratic Republic of Congo (DRC). The outbreak—DRC’s 10th on record—was concentrated in a conflict Alexis Arieff zone, complicating containment efforts, and became the world’s second-largest Ebola Specialist in African Affairs outbreak ever. Attacks on health workers repeatedly impeded containment efforts, as did political tensions, local community suspicion of government officials and international actors, and local frustrations at perceived profiteering by responders. Eventual success in containing the outbreak was attributable, in part, to the deployment of new vaccines first pioneered during the West Africa outbreak, advances in experimental therapeutics, and changes in the coordination of response efforts on the ground. Relief over ending the 2018-2020 eastern DRC Ebola outbreak was muted, however, by the detection of a new outbreak, DRC’s 11th to date, in the western part of the country in the same month—and by the global Coronavirus Disease 2019 (COVID-19) pandemic, which has posed new health challenges in DRC and severely affected the country’s economy. The DRC government and international partners also face other health challenges, including intermittent outbreaks of measles, cholera, and malaria, and relatively high preventable death rates (particularly in the areas of maternal and child health) resulting from inadequate access to clean water, sanitation, and hygiene (WASH) and primary health care. Poor conditions at health facilities continue to frustrate efforts to convince individuals with Ebola symptoms to seek diagnosis and treatment. According to the U.N. Office for the Coordination of Humanitarian Affairs (UNOCHA), fewer than 30% of health facilities in the country are equipped to provide basic medical care, including vaccines, antidiarrheal treatment, undernutrition, or prenatal and postnatal care. The prolonged battle to contain the Ebola outbreak in eastern DRC, coupled with what appear to be more frequent outbreaks in the country, raise questions about the allocation of U.S. global health resources and bilateral aid for DRC. New vaccines and therapeutics are potential game-changers in responding to new Ebola outbreaks, yet local health system weaknesses, community mistrust, and barriers to humanitarian access have continued to present obstacles. Among the issues that Congress might consider include the relative ranking of U.S. global health priorities in the context of COVID-19, the implications of frequent Ebola outbreaks for the global health security agenda, and lessons that may be gleaned from DRC about pandemic response in other complex conflict settings. The United States was the largest country donor to the international Ebola response effort in eastern DRC, with the U.S. Agency for International Development (USAID) and U.S. Centers for Disease Control and Prevention (CDC) playing a lead role. If responding to and preventing Ebola outbreaks remain congressional priorities in the future, Congress may consider how such efforts may be funded. Notably, USAID drew on unobligated International Disaster Assistance (IDA) funds that Congress had provided in FY2015—in the context of the 2014-2016 West Africa Ebola outbreak—as its core source of funding for Ebola response in eastern DRC. Since June, USAID has allocated resources for countering the new outbreak in the west, but since March 2020, the agency also has drawn on remaining unobligated FY2015 emergency Ebola appropriations to fund COVID-19 response efforts in developing countries worldwide. The CDC, for its part, also drew on 2015 Emergency Ebola supplemental appropriations, along with more recent appropriations for global disease detection and infectious disease response that, likewise, may be focused elsewhere in the current context. Total USAID funding for emergency response to the eastern DRC Ebola outbreak, at $342 million, also exceeded the U.S. annual bilateral health assistance budget for DRC ($217 million allocated in FY2019). Much of the U.S. bilateral health aid budget for DRC is focused on other disease-specific initiatives, namely HIV/AIDS, malaria, and tuberculosis, although DRC also receives U.S. health system strengthening aid through global programs. Congressional Research Service link to page 4 link to page 5 link to page 7 link to page 9 link to page 10 link to page 11 link to page 11 link to page 13 link to page 13 link to page 4 link to page 12 link to page 8 link to page 14 Ebola Outbreaks in the Democratic Republic of Congo: Emergencies or Enduring Threat? Contents Introduction ..................................................................................................................................... 1 Successes in Ebola Control ....................................................................................................... 2 Challenges in Ebola Control ..................................................................................................... 4 The International Response to the 2018-2020 Eastern DRC Outbreak ........................................... 6 U.S. Role and Funding: The 2018-2020 Outbreak in Eastern DRC ......................................... 7 Issues for Congress .......................................................................................................................... 8 Implications for U.S.-DRC Policy and Aid ............................................................................... 8 Lessons Learned for Pandemic Response in Conflict Settings? ............................................. 10 Global Health Security ............................................................................................................ 10 Figures Figure 1. Documented Ebola Outbreaks in DRC to Date ................................................................ 1 Figure 2. U.S. Bilateral Health Aid for DRC, by Program Objective ............................................. 9 Tables Table 1. Key Health Statistics: DRC, Africa, and the World ........................................................... 5 Contacts Author Information ......................................................................................................................... 11 Congressional Research Service link to page 4 Ebola Outbreaks in the Democratic Republic of Congo: Emergencies or Enduring Threat? Introduction On June 25, 2020, a nearly two-year Ebola virus outbreak in eastern Democratic Republic of Congo (DRC) was declared over, after claiming the lives of nearly 2,300 people.1 A new outbreak emerged the same month in the west of the country, marking the 11th documented Ebola outbreak in the country since the virus was first identified in DRC in 1976 (Figure 1).2 The eastern DRC outbreak (the country’s 10th) unfolded in an area without recent experience with the disease, and which was already experiencing complex armed conflicts and a protracted humanitarian crisis.3 The multilateral Ebola response effort confronted stark obstacles and frequent setbacks, including attacks on health workers, political tensions, local disinformation campaigns, intense community mistrust, and resource constraints, particularly in public health facilities.4 The outbreak, which peaked in mid-2019, became DRC’s largest ever, and the world’s second-largest after the 2014-2016 West Africa outbreak (which infected over 28,000 people and killed more than 11,000). Figure 1. Documented Ebola Outbreaks in DRC to Date Source: CRS graphic. Base map drawn from Esri (2016); case data from the WHO, as of August 2020. 1 Per World Health Organization (WHO) guidance, Ebola outbreaks are declared over when 42 days (twice the known incubation period) pass, with no new cases, after the discharge of all known Ebola patients. 2 See U.S. Centers for Disease Control and Prevention (CDC), “Years of Ebola Virus Disease Outbreaks,” at https://www.cdc.gov/vhf/ebola/history/chronology.html. Ebola is named after a river in DRC, and a Congolese scientist, Dr. Jean-Jacques Muyembe, played a key role in the virus’s discovery in 1976. Dr. Muyembe currently heads DRC’s National Institute for Biomedical Research and was appointed DRC’s national Ebola coordinator in mid-2019. 3 As of October 2018 (before the outbreak had substantially spread), 4.3 million people were in need of humanitarian aid in the two provinces, according to U.N. Office for the Coordination of Humanitarian Affairs (UNOCHA) data. 4 See National Public Radio (NPR), “‘It was unmistakably a directed attack’: 4 Ebola workers killed in Congo,” November 28, 2019. Congressional Research Service 1 Ebola Outbreaks in the Democratic Republic of Congo: Emergencies or Enduring Threat? The deployment of new vaccines and therapeutics, improved coordination of response efforts on the ground, and community-level engagement appear to have been key factors supporting containment of the eastern DRC outbreak. Yet, flagging donor commitment and competing needs—including the novel Coronavirus Disease 2019 (COVID-19) pandemic—have complicated and arguably diverted national and global resources from controlling the new outbreak in western Equateur province and ensuring adequate disease surveillance elsewhere the country.5 In early August 2020, the WHO issued a donor appeal requesting $18.4 million to control the new (11th) outbreak, which, at that point, was reportedly growing steadily with new health zones affected in hard-to-reach, remote villages.6 As in the 10th outbreak, Ebola responders have faced local resistance, particularly in reporting of cases, referring suspected cases to health facilities, and following safe and dignified burial practices. The prolonged battle to contain the Ebola outbreak in eastern DRC, coupled with what appear to be more frequent outbreaks in the country, raise questions about the allocation of U.S. global health resources and bilateral aid for DRC. Vaccines and therapeutics are potential game-changers, yet health system weaknesses, community mistrust, and barriers to humanitarian access remain obstacles. Among the issues that Congress might consider include the relative ranking of U.S. global health priorities in the context of COVID-19, the implications of frequent Ebola outbreaks for the global health security agenda, and lessons learned from DRC about pandemic response in complex conflict settings. If responding to and preventing Ebola outbreaks remain congressional priorities, Congress might also consider how such efforts may be funded. Successes in Ebola Control The extraordinary conditions in eastern DRC, particularly significant infrastructure constraints and security threats, limited the implementation of conventional infection control and prevention measures and required ever-evolving strategies for containment. Classic Ebola outbreak control protocol entails
- infection prevention control (IPC) in health care facilities;
- management and isolation of patients
in, ideally in specialized Ebola Treatment Centers (ETCs); -
fever surveillance with rapid diagnosis;
- tracing of Ebola cases and their contacts; and
- community awareness and adherence to IPC protocols, safe patient
and body transport, safecare, safe body transport and burials, and household and environmental decontamination. To overcome barriers caused by insecurity, inaccessibility, and poor IPC compliance in some health settings, Ebola responders adopted modified approaches, including expanded application of Ebola vaccines, deployment of innovative Ebola therapeutics, and local outreach to secure access and protection of health workers. Vaccines. During the 2014-2016 West Africa Ebola outbreak, health workers deployed a “ring vaccination” strategy for the first time, using an experimental vaccine (unlicensed at the time) under a “compassionate use” protocol. Ring vaccination entails vaccinating those who have come in contact with a known Ebola case, as well as their contacts. The same strategy was employed 5 In March, the WHO appealed for donors to fill “an immediate US$20 million funding gap,” or risk running out of money, and possibly missing new cases, before the outbreak was fully over. WHO, Remarks by Dr Ibrahima Socé Fall, “End in sight, but flare-ups likely in the Ebola outbreak in the Democratic Republic of the Congo,” March 6, 2020. 6 UNOCHA, “Republique Demoratique Du Congo,” Note d’information, rapport #56, 18 août 2020. Congressional Research Service 2 Ebola Outbreaks in the Democratic Republic of Congo: Emergencies or Enduring Threat? during the 2018-2020 outbreak in eastern DRC, although population mobility, suboptimal IPC practices in local health clinics, gaps in rapid diagnosis and isolation of infected individuals, and resistance by some communities limited its effectiveness. In February 2019, the World Health Organization (WHO) Strategic Advisory Group of Experts (SAGE) noted the “exceptional circumstances” of the eastern DRC outbreak (summarized above) and recommended adding geographic-targeted vaccination, entailing vaccinating residents in the area immediately surrounding an Ebola case, such as a village or neighborhood. In May 2019, the WHO SAGE recommended additional adjustments to the vaccine strategy, including “pop-up” vaccination to make the process faster, more secure, and more responsive to local feedback; streamlining implementation of the vaccination protocol; modifying follow-up for safety monitoring; and adjusting the dose of the vaccine to ensure vaccine availability (i.e., primary and secondary contacts would receive one-half the previously used dose and tertiary contacts would receive one-fifth of the previous dose). By the end of the outbreak, over 300,000 people had been vaccinated in the main outbreak zone (Ituri and North Kivu provinces) with the aforementioned experimental vaccine, rVSV-ZEBOV (brand name Ervebo, produced by Merck). In December 2019, Ervebo became the first Ebola vaccine to be approved by the U.S. Food and Drug Administration (FDA).7 In September 2019, Congolese officials approved use of a second vaccine candidate, Ad26.ZEBOV/MVA-BN, developed by Janssen Pharmaceuticals (a subsidiary of Johnson & Johnson) and Bavarian Nordic. As of August 18, 2020, more than 22,000 people had been vaccinated against Ebola in the new outbreak zone, Equateur province.8 Therapeutics. The FDA has not approved any antiviral drugs to treat Ebola, though experimental treatments (known as REGN-EB3 and mAb114) were used to care for Ebola patients during the 2018-2020 outbreak.9 Caretakers had otherwise primarily focused on addressing Ebola-related symptoms (e.g., through the provision of fluids intravenously, oxygen therapy, fever suppressants, and pain relievers). In August 2019, a study by the U.S. National Institutes of Health (NIH), the WHO, and the DRC National Institute of Biomedical Research reported that REGN-EB3 and mAb114 had proven effective in improving survival outcomes for Ebola patients during an investigational trial. While several other candidate therapies are also being evaluated, the WHO announced in August 2019 that it would follow the recommendations of an independent Data and Safety Monitoring Board to use only the two aforementioned therapies when treating Ebola patients.10 Over 2,100 people were treated with these therapies during the eastern DRC outbreak.11 7 WHO, “Ebola Virus Disease—Democratic Republic of the Congo, Weekly Epidemiological Record, Volume 27, Issue 95, pp. 301-324, July 3, 2020; U.S. FDA, Ebola Preparedness and Response Updates from FDA, at https://www.fda.gov. FDA approval followed a determination by the European Medicines Agency to grant conditional marketing authorization for the Ervebo vaccine. 8 UNOCHA, “Republique Demoratique Du Congo,” Note d’information, rapport #56, August 18, 2020. 9 CDC, Ebola Virus Disease, “Treatment,” at https://www.cdc.gov/vhf/ebola/treatment/index.html; and NIH, Independent Monitoring Board Recommends Early Termination of Ebola Therapeutics Trial in DRC Because of Favorable Results with Two of Four Candidates, August 12, 2019. 10 WHO, Update on Ebola Drug Trial: Two Strong Performers Identified, August 12, 2019. 11 WHO, “Ebola Virus Disease—Democratic Republic of the Congo, Weekly Epidemiological Record, Volume 27, Issue 95, pp. 301-324, July 3, 2020. Congressional Research Service 3 link to page 7 link to page 9 link to page 9 Ebola Outbreaks in the Democratic Republic of Congo: Emergencies or Enduring Threat? Local Engagement and Coordination of Response Efforts. Local resistance to Ebola response activities was a persistent feature of the eastern DRC outbreak—at times amounting to armed attacks and seemingly organized sabotage. While the extent of armed group involvement may have been unique to the geographic location of the outbreak, community resistance remains an obstacle in the new outbreak and likely in the future (see “Challenges in Ebola Control” below). Because willing local participation in efforts to prevent, identify, and rapidly isolate Ebola cases is crucial to containment, strong engagement with local communities has been a top priority among organizations responding to Ebola outbreaks in DRC, and in Ebola response generally.12 Steps by the DRC government in 2019 to address internal coordination and accountability problems may have helped improve coordination and local perceptions of responders. Notably, after former opposition figure Felix Tshisekedi was inaugurated president in early 2019, he centralized and elevated the coordination of response efforts to the office of the presidency, appointed an expert virologist to lead these efforts, and pursued investigations into health sector corruption under the previous DRC administration (see text box below). Donors, including the U.S. Agency for International Development (USAID), invested in efforts to improve and coordinate messaging around Ebola response efforts. In 2019, the U.N. peacekeeping operation in DRC took on a greater role in ensuring financial, logistical, and policy coordination among those involved in responding to the outbreak (see “The International Response to the 2018-2020 Eastern DRC Outbreak” below). Donors, including the United States, also expanded response efforts to include support for broader health and food security initiatives in Ebola-affected areas, both in response to local needs and as an effort to build local support for containment efforts. Challenges in Ebola Control Post-Outbreak Health Concerns. Scientists do not yet know whether Ebola infection confers lifelong immunity in all cases, as had been assumed prior to the 2014-2016 West Africa outbreak. Rare cases of relapse have been documented in West Africa and eastern DRC, while experts are continuing to investigate whether other cases were reinfected or relapsed.13 The persistence of the virus in the body has also raised questions about the risk for the reemergence of Ebola outbreaks after their containment, including in West Africa, which has over 17,000 Ebola survivors, and in eastern DRC, which has over 1,100 survivors.14 Noting that “survivor-linked transmission, undetected chains of transmission, and new introduction of Ebola virus into the human population from an animal reservoir” were possible, USAID reported in June 2020 that “response actors aim to continue supporting critical activities to detect and respond to additional cases that may emerge following the official end of the outbreak.”15 Health Infrastructure Constraints. DRC’s weak national health system posed a key challenge to Ebola response efforts during the tenth outbreak, notwithstanding the country’s prior experience and expertise in Ebola control. According to the U.N. Office for the Coordination of Humanitarian Affairs (UNOCHA), as of early 2020 fewer than 30% of health facilities had the 12 See WHO, “Ebola in the Democratic Republic of the Congo: North Kivu, Ituri 2018 – 2020,” at https://www.who.int/emergencies/diseases/ebola/drc-2019; and WHO et al, Risk Communication and Community Engagement Preparedness and Readiness Framework: Ebola Response in the Democratic Republic of Congo in North Kivu, September 2018. 13 WHO, Ebola Virus Disease-Democratic Republic of the Congo: External Situation Report 72, December 17, 2019. 14 C. Raina MacIntyre and Abrar Chughtai, “Recurrence and Reinfection-A new Paradigm for the Management of Ebola Virus Disease,” International Journal of Infectious Diseases, volume 43, (2016), pp. 58-61. 15 USAID, “Democratic Republic of the Congo – Ebola Outbreaks,” FY2020 Fact Sheet #7, June 29, 2020. Congressional Research Service 4 link to page 8 link to page 8 link to page 8 link to page 8 link to page 8 link to page 8 link to page 8 Ebola Outbreaks in the Democratic Republic of Congo: Emergencies or Enduring Threat? operational capacity to provide basic medical care, significantly limiting the ability to provide preventive care, including the provision of vaccines, maternal and child health care, and control of measles, cholera, and malaria.16 Deaths and illness from these causes in DRC have, for years, exceeded regional and global averages (Table 1). Faced with limited health resources, authorities redirected local health resources to Ebola control in some hotspots, including those for regular vaccination campaigns, deepening mistrust by some of government authorities. Between 2019 and mid-2020, DRC experienced the world’s worst measles epidemic at the time, which killed over 7,000 children. Health system capacity has likely been further weakened by Ebola deaths among health workers: the WHO reported in December 2019 that Ebola had killed at least 34 health workers in eastern DRC since the outbreak in that region began.17 Table 1. Key Health Statistics: DRC, Africa, and the World Maternal New Mortality Child Stunting New HIV Malaria New TB Ratioa Mortality Among Infectionsb Infectionsb Infectionsb Physician (per Rateb (per Children (per 1,000 (per 1,000 (per Densityc 100,00 live 1,000 live Under 5 uninfected pop. at 100,000 (per 10,000 births) births) (%) pop.) risk) pop.) pop.) DRC 473 88 42.7 0.21 319.8 321 0.7 Africa 525 76 32.5 1.07 229.3 231 3.0 World 211 39 21.3 0.24 57.4 132 15.6 Source: WHO, World Health Statistics 2020: Monitoring Health for the SDGs [Sustainable Development Goals], 2020. a. Data col ected in 2017. b. Data col ected in 2018. c. Data col ected in 2016. Security and Governance Challenges. At the height of the eastern DRC outbreak in mid-2019, U.S. officials and other health experts identified local tensions and political grievances, along with security threats, as key challenges.18 Attacks by local militias and criminal groups, political protests, health worker strikes, and security force abuses repeatedly disrupted and impeded response efforts. In 2019, then-USAID Administrator Mark Green urged a multifaceted “development approach” toward the outbreak, referring to DRC as a “failed democracy” that had undermined “the Congolese people’s trust in institutions.”19 From the start of the outbreak in August 2018 through March 2020, the WHO documented 420 attacks on health facilities in the main outbreak zone, resulting in 11 deaths and 86 injuries.20 In many cases, assailants were never conclusively identified. Local mistrust of government officials and perceived outsiders (including Congolese responders from other parts of the country) contributed to community resistance. The first year of the 16 UNOCHA, Democratic Republic of the Congo, Health Cluster Report, March 2020. 17 WHO, Disease Outbreak News Report on the DRC, December 12, 2019. 18 See, for example, House Foreign Affairs Subcommittee on Africa, Global Health, Global Human Rights and International Organizations (“HFAC Africa Subcommittee”), hearing, “Eradicating Ebola: Lessons Learned and Medical Achievements,” June 4, 2019; and WHO, “High-Level Event on Ebola Virus Disease in DRC,” July 15, 2019. 19 Mark Green, testimony before the Senate Appropriations Subcommittee on State, Foreign Operations, and Related Programs, hearing, “Review of the FY2020 Budget Request for USAID,” April 30, 2019; and “How to End the Ebola Crisis [Op-Ed],” CNN, August 22, 2019. 20 WHO, Remarks by Dr Ibrahima Socé Fall, March 6, 2020, op. cit. Congressional Research Service 5 Ebola Outbreaks in the Democratic Republic of Congo: Emergencies or Enduring Threat? outbreak also coincided with a fraught political transition process, during which the outgoing national government’s decision to delay and, in some cases, cancel elections in the outbreak zone (an opposition stronghold) heightened tensions and spurred conspiracy theories.21 Perceptions that outsiders were profiting financially from the response effort, or that international interventions were driven more by Westerners’ fear of contagion than by concern for locals’ wellbeing, also appear to have fueled local mistrust, as well as kidnappings of Ebola responders.22 Corruption Concerns in the Ebola Response From the start of the eastern DRC outbreak, the DRC government’s health responses were coordinated by the Ministry of Health (MoH), as in past Ebola outbreaks in the country. In July 2019, newly elected President Etienne Tshisekedi transferred coordination responsibilities to an expert committee headed by the director of DRC’s national biomedical research institute, Dr. Jean-Jacques Muyembe. Dr. Muyembe is a renowned expert on Ebola who helped investigate the first known outbreak of the disease in DRC in 1976. Health Minister Dr. Oly Ilunga resigned fol owing Dr. Muyembe’s appointment, complaining of a dilution of his authority, confusion about the lines of coordination, an insufficient focus on the health system, and opposition to introducing a second vaccine as part of the response. A DRC government investigative commission subsequently issued scathing criticism of Dr. Ilunga, indicating, among other things, that the minister and his team had displayed an “aggressive and ostentatious attitude” when visiting the outbreak area and had squandered Ebola response funds on fancy cars and hotel rooms.23 In March 2020, a DRC court sentenced Ilunga to prison for allegedly embezzling Ebola response funds.24 This was not the only case of apparent misappropriation of funds and other abuses by various actors involved in responding to the eastern DRC outbreak. As of mid-2020, investigative journalists, U.N. agencies, and NGOs had identified a range of problematic behavior that likely contributed to local mistrust of responders, including alleged sexual exploitation, petty corruption, and inflated fees and kickbacks paid to DRC state security forces (who have repeatedly been implicated in gross human rights violations).25 Overall, perceived profiteering and corruption among DRC officials and others came to be known as the “Ebola business.” The International Response to the 2018-2020 Eastern DRC Outbreak The Congolese government has led the response to successive Ebola outbreaks in DRC, with support from the World Health Organization, nongovernmental organizations, donors, and other partners. National and international nongovernmental organizations partnered with the Congolese government to provide direct support for activities such as IPC training, communication campaigns, and disease surveillance, while U.N. agencies (including the WHO), other multilateral entities (including the World Bank), and foreign governments provided funding, technical expertise, coordination, and/or logistical assistance. Most of the direct patient care was provided by Congolese nationals. As a WHO official noted at the height of the outbreak in June 2019, “If you go into the treatment facilities now it is Congolese doctors and nurses in the front line. There may be NGO or WHO badges on the tents but the doctors and nurses are Congolese; surveillance officers are Congolese; 80% of the vaccinators in this response are Congolese.”26 21 See CRS Report R43166, Democratic Republic of Congo: Background and U.S. Relations. 22 New York Times, “Ebola Outbreak Reaches Major City in Congo, Renewing Calls for Emergency Order,” July 15, 2019. 23 New York Times, “In Congo, a New Plan to Fight Ebola Follows a Government Power Struggle,” July 26, 2019. 24 Reuters, “Former DR Congo Health Minister Convicted of Embezzling Ebola Funds,” March 23, 2020. 25 The New Humanitarian, “How ‘Ebola business’ threatens aid operations in Congo,” June 18, 2020. 26 WHO, “Ebola Outbreak in the Democratic Republic of the Congo,” Press Briefing, June 6, 2019. Congressional Research Service 6 Ebola Outbreaks in the Democratic Republic of Congo: Emergencies or Enduring Threat? The African Union (AU) Africa Centers for Disease Control and Prevention (Africa CDC) also deployed members of its voluntary response corps to DRC and neighboring countries to provide technical assistance. The U.N. Stabilization Mission in Congo (MONUSCO) provided logistical and security support to Ebola response efforts while also seeking to fulfill its otherwise wide-ranging civilian-protection and stabilization mandate. Starting when the WHO declared the eastern DRC outbreak to be a Public Health Emergency of International Concern (PHEIC) in July 2019 (about 11 months after the first cases were identified), the WHO sought emergency donor funds, as well as international support for addressing local political and security challenges. Over a series of appeals to donors from August 2018 through mid-2020, the WHO sought a total of $570 million to support public health response and regional preparedness efforts, of which donors ultimately provided about $276 million.27 The WHO appeals aimed to support clinical care, disease surveillance, contact tracing, vaccinations, laboratory capacity, infection prevention and control, clean water and sanitation, safe and dignified burials, psychosocial care, operational preparedness, and coordination.28 In May 2019, in response to concerns (including among U.S. officials) that a lack of operational coordination and transparency were stymying efforts to improve humanitarian access and address security threats, the U.N. Secretary-General established a new position of U.N. Ebola Response Coordinator. David Gressly, a U.S. citizen serving as the Deputy Special Representative of the U.N. Secretary-General within MONUSCO, was appointed to the post. He sought to strengthen financial tracking, humanitarian coordination, political engagement, and “preparedness and readiness planning,” while the WHO continued to lead on health operations and technical support activities.29 Gressly returned to his regular position within MONUSCO in March 2020, at which time the U.N. response coordinator position was deemed no longer necessary. U.S. Role and Funding: The 2018-2020 Outbreak in Eastern DRC The United States was the largest country donor to the international Ebola response effort during the outbreak in eastern DRC. USAID and CDC were the primary federal entities involved. The Trump Administration largely restricted U.S. government personnel from traveling to and within the main outbreak zone for most of its duration due to security concerns, with some exceptions for high-level visits. (U.S. personnel were stationed in Kinshasa, in the eastern DRC city of Goma, and in neighboring countries, while U.S. implementing partners used U.S. resources to conduct activities within the outbreak zone.) The Trump Administration deployed a USAID-led Disaster Assistance Response Team (DART) to the region starting in September 2018 to coordinate the U.S. response in support of the DRC government, the WHO, and other partners, and established a Washington, D.C.-based Response Management Team to support the DART. CDC staff supported and participated in these effort, while NIH supported trials of Ebola vaccines and therapeutics in partnership with the WHO and DRC’s National Institute of Biomedical Research. Over the duration of the eastern DRC Ebola outbreak (August 2018-June 2020), USAID provided over $342 million in support of response and preparedness activities in DRC and neighboring countries. The bulk of these funds were drawn from unobligated FY2015 International Disaster Assistance (IDA) that Congress had appropriated on an emergency basis for Ebola response during the West Africa outbreak under P.L. 113-235. USAID also drew on foreign assistance 27 See WHO strategic response plans, at https://www.who.int/emergencies/diseases/ebola/drc-2019/funding. 28 See WHO and DRC Ministry of Health, Strategic Response Plan for the Ebola Virus Disease Outbreak in the Provinces of North Kivu and Itur, Democratic Republic of the Congo, July – December 2019. 29 Ibid. See also Ziemer testimony before the HFAC Africa Subcommittee, “Eradicating Ebola,” June 4, 2019, op. cit. Congressional Research Service 7 link to page 11 Ebola Outbreaks in the Democratic Republic of Congo: Emergencies or Enduring Threat? funds provided under the Global Health Programs (GHP) and Food for Peace (FFP) accounts. CDC, for its part, allocated approximately $36.7 million in support of Ebola control efforts in eastern DRC, drawing on the 2015 Emergency Ebola supplemental appropriations, 2018 and 2019 appropriations for global disease detection, and the Infectious Disease Rapid Response Reserve Fund.30 CDC provided technical assistance through its personnel in the field and at headquarters in the United States. According to the U.S. Embassy in DRC, total U.S. federal funding allocated in response to the eastern DRC Ebola outbreak reached $600 million, including CDC and NIH activities as well as other U.S. Department of Health and Human Services contributions.31 More broadly, the United States is the top country donor of emergency humanitarian assistance to DRC and the top financial contributor to MONUSCO (see “Issues for Congress” below). Issues for Congress In FY2015, at the height of the West Africa Ebola outbreak, Congress appropriated $5.1 billion for Ebola response and preparedness on an emergency basis, including $1.436 billion in multiyear International Disaster Assistance (IDA) funds (Title IX of Division J, P.L. 113-235). USAID primarily used the unobligated balance of these IDA funds to respond to the 2018-2020 eastern DRC Ebola outbreak. As of August 2020, it was unclear whether any of these funds were being used to support Ebola control efforts in Equateur (western DRC) after a new outbreak was detected there in June 2020. USAID’s heavy reliance on FY2015 emergency appropriations for Ebola response may raise questions about how the agency would provide additional support for Ebola control if the Equateur outbreak is not rapidly contained or if another outbreak occurs in the near term, in DRC or elsewhere. Looking ahead, and weighing the threat of Ebola against other global pandemic threats such as COVID-19, Congress may consider what funding mechanisms, if any, the United States might use to support Ebola prevention and preparedness in the future. Members may also examine the U.S. role, vis-à-vis other actors (including other countries, multilateral entities, and private sources), in financing Ebola prevention and preparedness activities, and may debate strategies for securing additional contributions from other sources. Additional issues Congress might consider are discussed below. Implications for U.S.-DRC Policy and Aid The prospect of potentially larger and/or more frequent Ebola outbreaks, alongside competing global pandemic response needs, may raise questions about where Ebola response fits into broader U.S. health and stabilization priorities and approaches toward DRC, and Africa more broadly. This includes the extent to which Ebola-related foreign assistance should continue to be funded via global emergency response mechanisms, as opposed to being integrated into annual bilateral aid budget planning. The U.S. Embassy in DRC reported in June 2020 that, the United States would be able “to build up the DRC’s longer-term preparedness capacity amidst the varied health-security threats the DRC faces,” as a U.S. Global Health Security Agenda (GHSA) 30 CDC response to CRS query, July 2020. 31 U.S. Ambassador Mike Hammer, “Together We Stopped Ebola in the East; Together We Can Advance a Better Future for the DRC,” U.S. Embassy Kinshasa, June 25, 2020. Congressional Research Service 8 link to page 12 Ebola Outbreaks in the Democratic Republic of Congo: Emergencies or Enduring Threat? intensive support country.32 U.S. GHSA aid programming is generally funded through globally allocated resources, as opposed to bilateral foreign assistance planned at the country level. DRC is a significant recipient of U.S. bilateral aid in sub-Saharan Africa, with $284 million allocated in FY2019 appropriations. Of that total, $217 million (76%) was for health assistance (see Figure 2), roughly the same proportion as for U.S. bilateral aid to sub-Saharan Africa generally.33 The United States is also by far the top country donor of emergency humanitarian assistance for DRC, with programs focusing on conflict-affected populations and those suffering from acute food insecurity. Excluding funds primarily targeted at Ebola response, U.S. emergency humanitarian aid obligations for DRC in FY2019 totaled $344 million.34 Figure 2. U.S. Bilateral Health Aid for DRC, by Program Objective State Department + USAID, Allocations of FY2019 Appropriations Source: Created by CRS using data provided to CRS by USAID, February 2020. Notes: Does not include funding administered on a global basis (including Global Health Security Agenda and pandemic preparedness funds) or U.S. contributions to multilateral initiatives. DA=Development Assistance; ESF=Economic Support Fund; GHP=Global Health Programs. Given that the lengthy and costly international response to DRC’s 10th outbreak was prolonged, in part, by armed conflicts and political instability, Members of Congress may weigh the scale and prioritization of aid and diplomatic resources devoted to addressing these challenges. DRC is a significant recipient of U.S. aid for peace and security and for democracy and governance activities: the State Department and USAID allocated $12 million in FY2019 bilateral aid appropriations to support the professionalization and capacity of DRC’s military, police, and internal security forces, and $17 million in support of democracy, governance, and human rights-related programs in the country.35 The United States is also the top provider of funds for MONUSCO (as with all U.N. peacekeeping operations), allocating $313 million in FY2019.36 Whether enduring problems illustrate that existing donor aid is insufficient, or, alternately, that existing aid programs are ineffective, may be debated. The Trump Administration has repeatedly proposed to decrease U.S. bilateral aid for DRC—although not as much as for many other African countries, and its bilateral health aid budget proposals have varied. In foreign aid appropriations measures between FY2018 and FY2020, Congress generally did not enact the Administration’s 32 U.S. Ambassador Mike Hammer, “Together We Stopped Ebola in the East; Together We Can Advance a Better Future for the DRC,” U.S. Embassy Kinshasa, June 25, 2020. 33 CRS Report R46368, U.S. Assistance to Sub-Saharan Africa: An Overview, coordinated by Tomas F. Husted. 34 USAID, “Democratic Republic of the Congo – Complex Emergency,” FY2019 Fact Sheet #2, September 30, 2019. 35 CRS calculation based on data provided by USAID (February 2020) and published in the State Department Budget Justification for FY2021. 36 State Department Congressional Budget Justification for FY2021; see also CRS In Focus IF10597, United Nations Issues: U.S. Funding of U.N. Peacekeeping, by Luisa Blanchfield. Congressional Research Service 9 Ebola Outbreaks in the Democratic Republic of Congo: Emergencies or Enduring Threat? global foreign aid budget proposals, including with regard to DRC. For example, Congress provided at least $80 million in Development Assistance (DA) budget authority for DRC in FY2020 appropriations, nearly twice the Administration’s budget proposal for bilateral economic aid to the country.37 Despite its regular criticisms of U.N. peacekeeping worldwide, the Administration also voted in the U.N. Security Council to extend MONUSCO’s mandate for at least one more year on December 19, 2019, via a Resolution that recognized the mission’s “positive role” in coordinating international Ebola response efforts.38 At the same time, the Administration secured a decrease in MONUSCO’s authorized troop level in the same Resolution, along with language calling on the mission to plan to draw down further in the coming years, with an eye toward full exit. Lessons Learned for Pandemic Response in Conflict Settings? With its many setbacks, the 2018-2020 Ebola response effort may contain lessons for pandemic preparedness and response efforts in other conflict-affected settings where central government authority is weak or contested. Many of the challenges that confronted Ebola responders in eastern DRC are not unique to the area, and are reminiscent of challenges facing efforts to contain COVID-19 in many parts of the world, including in some parts that are ostensibly peaceful.39 These include persistent misinformation and conspiracy theories about the disease, corruption in the allocation of public health resources, a lack of coordination among responders, community resistance to public health measures, and local mistrust of public authorities. Greater prioritization of local community engagement—including efforts to address perceived exclusion of local residents in hiring decisions—and improved transparency and coordination of international aid activities arguably led to a turning point toward Ebola containment in late 2019. (Whether local hiring initiatives specifically contributed, knowingly or not, to kickback schemes and other alleged corruption in the response effort is unclear.40) USAID’s decision to broaden its emergency Ebola response funding to include resources, for example, for broader health initiatives and food aid for affected communities within the outbreak zone, as well as stepped-up resources for communication and messaging, may also have helped alleviate local rejection of the Ebola response effort. Global Health Security The Ebola outbreak in eastern DRC prompted the resumption of discussions about strengthening health systems worldwide, particularly with regard to pandemic preparedness. During that outbreak, several Members introduced legislation aimed at bolstering U.S. engagement in the multilateral GHSA—through which the United States has prioritized pandemic preparedness and response in DRC—and for strengthening health systems worldwide. In 2014, during the Obama Administration, the United States and the WHO co-launched the GHSA to improve countries’ ability to prevent, detect, and respond to infectious disease threats.41 The United States, the largest 37 Explanatory statement accompanying Division G of H.R. 1865 (P.L. 116-94). For FY2020, as in prior years, the Administration proposed to replace the DA foreign assistance account and several others with a consolidated Economic Support and Development Fund (ESDF) account. 38 U.N. Security Council Resolution 2502 (2019). 39 See also CRS Insight IN11285, Fostering Behavior Change During Disease Outbreaks: Insights from Ebola Response in Africa, by Alexis Arieff, Tomas F. Husted, and Nicolas Cook. 40 The New Humanitarian, “How ‘Ebola business’ threatens aid operations in Congo,” op. cit. 41 For more information on the GHSA, see CRS In Focus IF10022, The Global Health Security Agenda (2014-2019) Congressional Research Service 10 Ebola Outbreaks in the Democratic Republic of Congo: Emergencies or Enduring Threat? donor to this multilateral effort, pledged to support it with $1 billion from FY2015 through FY2019. In 2019, the White House released the United States Government Global Health Security Strategy, which outlined the U.S. role in extending the GHSA and improving global health security worldwide.42 Although the Trump Administration, through the strategy and public statements, has signaled support for extending the GHSA through 2024, officials have not provided comprehensive information on what that support would entail. Congress might consider funding provided for global health security and pandemic preparedness through regular appropriations. Over time, appropriations for preventing and responding to pandemics have totaled far less than the billions spent on responding to pandemics and infectious disease outbreaks. Given U.S. endorsement of the GHSA across two Administrations and the emphasis the United States has placed on DRC through the initiative, Members of Congress may consider what role, if any, the United States should play in supporting the GHSA, including whether to codify U.S. engagement in the GHSA. President Obama issued an executive order in November 2016 that established an interagency Pandemic Preparedness and Response Directorate to bolster pandemic preparedness capacity at home and abroad.43 The executive order named the National Security Council as the chair, specified $1 billion for advancing the GHSA, and outlined the role of participating agencies and departments. The Trump Administration has provided verbal support for the GHSA but has dismantled some of the structure established through the executive order.44 A number of bills have been introduced in the 116th Congress to codify a coordinated approach to pandemic preparedness and support for the GHSA. The Global Health Security Act of 2020 (H.R. 2166 and S. 3302), for example, would call for establishing a Special Advisor for Global Health Security within the Executive Office of the President to coordinate U.S. federal government global health security activities, convene and chair a Global Health Security Interagency Review Council, and submit a biannual report to Congress on related activities, among other things. Author Information Tiaji Salaam-Blyther Alexis Arieff Specialist in Global Health Specialist in African Affairs and International Health Regulations (2005), by Tiaji Salaam-Blyther. 42 White House, United States Government Global Health Security Strategy, 2019. 43 White House, “Advancing the Global Health Security Agenda to Achieve a World Safe and Secure from Infectious Diseases Threats,” November 4, 2016. 44 Ronald Klain, Testimony before the Asia, Pacific and Non-Proliferation Subcommittee of the House Committee on Foreign Affairs, “Lessons from the West African Ebola Response: How to Save Lives and Protect Our Nation During the Novel Coronavirus Epidemic of 2020,” February 5, 2020. Congressional Research Service 11 Ebola Outbreaks in the Democratic Republic of Congo: Emergencies or Enduring Threat? Disclaimer This document was prepared by the Congressional Research Service (CRS). CRS serves as nonpartisan shared staff to congressional committees and Members of Congress. It operates solely at the behest of and under the direction of Congress. Information in a CRS Report should not be relied upon for purposes other than public understanding of information that has been provided by CRS to Members of Congress in connection with CRS’s institutional role. CRS Reports, as a work of the United States Government, are not subject to copyright protection in the United States. Any CRS Report may be reproduced and distributed in its entirety without permission from CRS. However, as a CRS Report may include copyrighted images or material from a third party, you may need to obtain the permission of the copyright holder if you wish to copy or otherwise use copyrighted material. Congressional Research Service R45933 · VERSION 5 · UPDATED 12burials, and household and environmental decontamination.
The extraordinary conditions on the ground in affected areas of eastern DRC have limited the effectiveness of conventional control measures, however, and are requiring ever-evolving strategies for containment, including aggressive vaccination campaigns (see text box below). Since the WHO declared the outbreak to be a Public Health Emergency of International Concern (PHEIC) in July 2019, it has sought to garner additional donor funds, as well as international support for addressing the political and security issues affecting Ebola control.
In July 2019, the WHO and the DRC Ministry of Health (MoH) released a fourth strategic response plan to "definitively defeat" the Ebola epidemic (Table 1). The strategic plan is expected to cost over $462 million, including about $288 million for the public health response portion (Table 1). In July 2019, the World Bank announced that it would provide $300 million toward the plan, about half of which would support the public health response, on top of prior funding commitments (discussed below).10
The public health portion of the strategic plan, covering July 1 through December 31, 2019, purportedly takes into account lessons learned from the third strategic response plan (February through July 2019). This portion of the plan is based on
- strengthening political commitment, security, and operational support to improve acceptance of the response and access to insecure areas;
- deepening support for addressing the varied needs of communities affected by Ebola (beyond a single-minded focus on containment efforts), as a means toward fostering community ownership and involvement in Ebola responses;
- improving financial planning, monitoring and reporting; and
- bolstering preparedness of neighboring provinces and countries.
|
Activity |
|
Lead |
Co-Lead |
|
Risk Communication and Community Engagement |
38.3 |
MOH |
UNICEF |
|
Surveillance, Contact Tracing and Vaccination |
42.7 |
MOH |
WHO |
|
Laboratory and Research |
3.2 |
MOH |
WHO |
|
Patient Care, Isolation and Survivors Follow-Up |
54.7 |
MOH |
WHO |
|
Infection, Prevention and Control |
41.6 |
MOH |
WHO & UNICEF |
|
Safe and Dignified Burials |
18.8 |
MOH |
IFRC |
|
Psychosocial Care |
10.4 |
MOH |
UNICEF |
|
Operational Preparedness |
6.1 |
MOH |
WHO |
|
Coordination + Support to Coordination |
71.9 |
MOH |
WB, UNOCHA, and WHO |
|
Public Health Response Total |
287.7 |
||
|
Security, Political Engagement, Operations Support |
11.5 |
||
|
Strengthened Support to Communities |
97.1 |
||
|
Strengthened Preparedness for Surrounding Countries |
66.0 |
||
|
Total Ebola Strategic Response Plan |
462.3 |
||
Sources: DRC Ministry of Health, Strategic Response Plan for the Ebola Virus Disease Outbreak in the Provinces of North Kivu and Ituri, Democratic Republic of Congo, July-December 2019, July 2019; and WHO Health Emergencies Program, Funding Requirements – SRP 4 – Jul to Dec 2019, September 3, 2019.
The World Bank has urged other countries to provide additional support, and the WHO Director-General has urged donors to address disbursement delays. As of September 11, 2019, the WHO had received less than $60 million of the $288 million it sought for the current phase of the public health response.11 The United States is the top country donor for the public health response and has provided almost $158 million for the Ebola humanitarian response, largely supporting activities by nongovernmental organizations (NGOs), as discussed below.
|
Vaccination Strategy During the 2014-2016 West Africa outbreak, Ebola responders deployed an experimental vaccine, rVSV-ZEBOV-GP (produced by Merck). Responders are now using that vaccine to control the DRC outbreak, and the WHO announced on September 23, 2019, that Congolese officials had approved deploying a second vaccine candidate (Ad26.ZEBOV/MVA-BN), developed by Janssen Pharmaceuticals (a subsidiary of Johnson & Johnson) and Bavarian Nordic. The announcement followed a period of controversy in which DRC's then-Minister of Health refused to authorize the Janssen candidate, citing concerns about safety and the potential to undermine community acceptance of Ebola control efforts.12 (The Janssen vaccine requires two doses, while the Merck vaccine requires a single dose.) The DRC Health Minister has since resigned. Both vaccine candidates have been submitted for approval to the U.S. Food and Drug Administration (FDA).13 Two other vaccine candidates are licensed solely in their respective countries of origin: Ad5-EBOV, in China, and GamEvac-Combi, in Russia. During the 2014-2016 West Africa Ebola outbreak, health workers deployed a "ring vaccination" strategy for the first time. This entails vaccinating those who have come in contact with a known Ebola case, as well as their contacts. Health workers have used this strategy in the current outbreak, with some success, but population mobility, suboptimal infection prevention and control practices in local health clinics, gaps in rapid diagnosis and isolation of infected individuals, and resistance by some communities have limited its effectiveness. In February 2019, the WHO Strategic Advisory Group of Experts (SAGE) noted the "exceptional circumstances" of the DRC outbreak and recommended adding geographic-targeted vaccination, entailing vaccinating residents in the area immediately surrounding an Ebola case, such as a village or neighborhood. The SAGE also recommended that "consideration is given to the use of any of [the three] new vaccines to vaccinate health care workers and frontline workers in the neighboring areas where there is a possibility of spread." If a confirmed Ebola case is observed, however, guidance indicates the rVSV-ZEBOV-GP vaccine must be used for a ring or geographic-targeted vaccination in preference to the new vaccine candidates. In May 2019, the WHO SAGE recommended additional adjustments to the vaccine strategy, including
On September 23, 2019—the same day the WHO asserted that "[t]here are enough vaccine doses on the ground to meet the current needs"—Doctors Without Borders called for an independent Ebola vaccination committee to oversee vaccination activities.14 Among other things, the organization asserted that the WHO was limiting the use of vaccines in the field and that at least twice as many people should have been vaccinated to date. As of that date, more than 220,000 people had been vaccinated, including almost 45,000 health workers (HWs) and frontline workers (FLWs).15 Thousands of HWs and FLWs in neighboring countries have also been vaccinated, including 580 in Burundi; 3,000 in Rwanda; 2,974 in South Sudan; and 4,915 in Uganda as of August 24, 2019. |
DRC Government Role
DRC government employees and other Congolese nationals are the primary responders to the Ebola epidemic on the ground. As WHO Executive Director for Health Emergencies Dr. Michael Ryan noted in June 2019, "If you go into the treatment facilities now it is Congolese doctors and nurses in the front line. There may be NGO or WHO badges on the tents but the doctors and nurses are Congolese; surveillance officers are Congolese; 80% of the vaccinators in this response are Congolese."16 The DRC government has provided health workers and administrative personnel, hired local frontline workers, organized volunteers, and conducted information awareness campaigns. The government has also offered certain health services free of charge in selected government health facilities, with donor support (discussed below).
From the start of the current outbreak, the DRC government's health responses were coordinated by the MoH, as in past Ebola outbreaks in DRC. In July 2019, however, President Tshisekedi transferred coordination responsibilities to an expert committee headed by the director of DRC's biomedical research institute, Dr. Jean-Jacques Muyembe, who reports directly to the president. Dr. Muyembe is a recognized expert on Ebola who helped investigate the first known outbreak of the disease, in DRC in 1976. Then-Health Minister Dr. Oly Ilunga resigned following Dr. Muyembe's appointment, citing a dilution of his authority as well as confusion about the coordination of DRC government Ebola responses, an insufficient focus on the health system, and opposition to utilizing the Johnson & Johnson experimental vaccine (see text box above). Ilunga was subsequently the target of scathing criticism in the leaked report of a DRC government investigative commission, which indicated, among other things, that Ilunga and his team had displayed an "aggressive and ostentatious attitude" when visiting the outbreak area and had squandered Ebola response funds on fancy cars and hotel rooms.17 These developments have suggested an internal power struggle over policy and control of funds for Ebola response.
U.N. and Other Multilateral Organizations
Humanitarian experts, including U.S. officials, have repeatedly asserted that broader humanitarian access and security issues have stymied outbreak control efforts, and that international response efforts require increased coordination and transparency.18 In response to such concerns, in May 2019 U.N. Secretary-General António Guterres appointed MONUSCO Deputy Special Representative David Gressly, a U.S. citizen, to serve as a new U.N. Emergency Ebola Response Coordinator charged with establishing a "strengthened coordination and support mechanism" for Ebola response.19 While the WHO is to continue to lead "all health operations and technical support activities to the government," Gressly is leading a broader U.N.-wide effort to strengthen political engagement, financial tracking, humanitarian coordination, and "preparedness and readiness planning" for Goma and surrounding countries.20 Gressly, who continues to report to the head of MONUSCO, portrayed his new role as a reflection of the need for "more than just a public health response."21
The WHO has deployed some 700 personnel to DRC since the current outbreak began. These personnel are coordinating the public health response and providing operational and technical support to DRC government personnel and other actors. Particular areas of focus include detection and rapid isolation of Ebola cases, intensification of rapid multidisciplinary public health actions for Ebola cases, community engagement, and health system strengthening. In addition, the WHO is coordinating regional readiness exercises and assessments in adjacent areas of DRC and neighboring countries. Vaccination and disease surveillance efforts have been bolstered in Uganda, Rwanda, and Burundi.
The World Bank has stepped up its role in supporting the Ebola response effort since mid-2019.22 On July 24, the World Bank Group announced it was mobilizing up to $300 million—to be financed through the Bank's International Development Association and its Crisis Response Window—on top of $100 million disbursed previously through the International Development Association and the Bank's Pandemic Emergency Financing Facility (PEF).23 The PEF announced a further $30 million disbursement for DRC on August 23, 2019.24 World Bank resources have financed free health care and essential medicines in clinics in all affected areas, hazard pay for frontline health workers, handwashing stations, mobile laboratories, decontamination teams, psychosocial support teams, community engagement campaigns, and vaccination efforts. The injection of new resources aims to build on existing World Bank support to strengthen the DRC health system.
The African Union (AU) Africa Centers for Disease Control and Prevention (Africa CDC) has supported international response efforts by deploying members of its voluntary response corps to DRC and neighboring countries. Africa CDC voluntary responders include epidemiologists and anthropologists, as well as communication, laboratory, and logistics experts from various African countries who are "on standby for emergency deployment."25 To date, these responders have trained local health workers and community volunteers, set up laboratories, supplied personal protective equipment, and trained people in port-of-entry screening.
The U.S. Government Response
USAID and the U.S. Centers for Disease Control and Prevention (CDC) deployed staff to DRC and the region when the outbreak was first detected in August 2018. The United States is also the top country donor to the Ebola response effort, as noted above. As of September 10, USAID had announced more than $148 million for direct support to the Ebola response within DRC and another $9.8 million to support preparedness and prevention activities in neighboring countries.26 Those funds were drawn primarily ($156.1 million) from unobligated FY2015 International Disaster Assistance (IDA) funds that Congress appropriated on an emergency basis for Ebola response during the West Africa outbreak (P.L. 113-235). According to USAID, the available balance of FY2015 emergency IDA Ebola funds stood at $105.5 million as of September 9.27
More broadly, the United States is the top bilateral humanitarian donor to DRC and the top financial contributor to MONUSCO, which is providing logistical and security support to Ebola response efforts. USAID Administrator Green testified before Congress in April 2019 that "there is sufficient money for fighting Ebola in DRC," asserting that nonfinancial challenges posed the primary constraint to containment efforts.28 U.S. funding commitments have continued to grow since then, however, as the outbreak has persisted and broadened.
U.S. personnel are providing technical support from Kinshasa, Goma, and neighboring Rwanda and Uganda, while implementing partners (U.N. agencies and NGOs) are administering Ebola response efforts within the outbreak zone with U.S. resources. The Administration has placed strict constraints on the movement of U.S. personnel to and within affected areas, due to security threats. In September 2018, USAID and CDC withdrew personnel from the immediate outbreak zone due to security concerns, despite CDC's stated preference to maintain staff in the field.29
U.S. support for outbreak control has included the following:
USAID has provided grant funding to NGOs and U.N. entities carrying out Ebola response and preparedness activities, drawing primarily on IDA funds (as noted above). In October 2018, USAID deployed a Disaster Assistance Response Team (DART) to coordinate the U.S. response in support of the DRC government, the WHO, and other partners. USAID Ebola response funds have supported disease surveillance, infection prevention and control, safe and dignified burials, water and sanitation aid, prepositioning of medical supplies, humanitarian coordination, and logistics.30 U.S. bilateral economic and health aid funding for DRC has also supported programs that may ease humanitarian access or otherwise complement Ebola response activities.
CDC personnel have provided direct technical support to the DRC government, the WHO, and USAID's DART for disease surveillance, contact tracing, data management, infection protection and control, risk communication and community engagement, laboratory strengthening, emergency management, and surveillance at points of entry. CDC staff also have supported Ebola preparedness efforts in neighboring countries.
The Department of Defense has supplied laboratory training to Ugandan researchers and has partnered with them to conduct clinical Ebola vaccine trials.
Challenges
Security Threats and Political Tensions
Security threats have periodically forced the temporary cessation of Ebola case management in some areas, interrupted contact tracing, and frustrated surveillance efforts in high-transmission areas. Dozens of armed groups are active in the areas most affected by the outbreak. These include an array of local militias, along with the Allied Democratic Forces (ADF), a relatively large and opaque group implicated in attacks on U.N. peacekeepers, local military forces, and civilians.31 Road travel is often dangerous, with frequent reports of militia attacks, armed robbery, and kidnappings.32 In April 2019, the Islamic State claimed responsibility for an attack on local soldiers previously attributed to the ADF, the latest in a series of signs of emerging ties between the two. State security force personnel reportedly maintain ties with armed groups and have been implicated in atrocities, including civilian massacres in Beni territory since 2014.33
Local mistrust of government officials and outsiders (including Congolese who are not from the immediate area)—sometimes rooted in conflict dynamics, ethnic tensions, and political friction—has prompted some community resistance to Ebola control efforts and led to attacks on health workers and facilities, including Ebola treatment centers. Some communities in Beni and Butembo have long opposed DRC's central government and complained of neglect and persecution. WHO officials have urged broader international support for "political mediation, engagement with opposition, and negotiated solutions," asserting that "[j]ust purely focusing on community engagement and participation will not fix what are deep seated political issues that need to be addressed at a higher level."34
Perceptions that outsiders are profiting financially from the outbreak, or that international intervention is driven more by fear of contagion than concern for locals' wellbeing, appear to have fueled conspiracy theories and community resistance. At a July 15 donors event on Ebola response in Geneva, WHO Director-General Dr. Tedros Adhanom Ghabreyesusi said that Congolese in the outbreak zone had asked him, "Are you here to help us, or to prevent this thing from coming to you? Are you doing this for us, or for yourself?" He added, "It embarrasses me.… We should not appear to be seen as if we are parachuting in and out because of Ebola."35 DRC's then-Health Minister argued in the same meeting that local perceptions that the response was bringing cash into the region had fueled threats to health workers, including kidnappings.
Health System Constraints
Local perceptions that donors are more concerned with preventing the spread of Ebola to their countries than with helping Congolese communities are rooted, in part, in enduring health challenges. Maternal and infant deaths, for example, have for years regularly exceeded the current count of Ebola deaths but have received comparatively little attention. Authorities have redirected health resources in some areas for Ebola control, deepening local frustrations. Vaccination campaigns have also been interrupted in some Ebola hotspots. In Ituri province, for example, inadequate supply of measles vaccine has limited containment of a measles outbreak that began in January and has infected over 161,000 people, claiming over 3,000 lives.36 Health workers also are fighting a cholera outbreak that has infected over 15,000 people and killed at least 287.37
The WHO has reported that Ebola transmission is likely occurring in ill-equipped and understaffed health facilities. Inconsistent adherence to infection prevention and control, periodic disruptions in supply chain systems, and limited access to water for handwashing in some health facilities have complicated Ebola control efforts. In addition, some health workers have refused to wear personal protective equipment in health facilities or perform rudimentary infection prevention and control measures due to threats of violence by some members of the community.38 As of August 27, 2019, 156 health workers had contracted Ebola, at least 34 of whom had died.39 The MoH, WHO, and other partners have identified health facilities of concern and are addressing lapses in triage, case detection, and infection prevention and control.
Reported Progress
Community Engagement. The WHO and implementing partners have worked to deepen local engagement, with some reported positive results. Local Ebola committees in Butembo and Katwa (at the center of the outbreak zone in North Kivu), for example, are chaired and managed by community members who plan Ebola awareness and sensitization campaigns.40 Improved community engagement has reportedly contributed to increased participation in vaccine campaigns and safe and dignified burial practices. For example, the WHO reported in July 2019 that a high-risk contact in Katwa had sought vaccination and offered to bring other contacts.41 In an effort to reduce the risk of transmission and broaden access to Ebola treatment and case finding, the WHO also plans to establish smaller patient transit centers closer to communities. Replicating engagement activities in emergent hot spots remains a challenge, however.42
Ebola Therapeutics Advance. In August 2019, a clinical trial of four investigational Ebola treatments in DRC identified two "strong performers," leading the WHO to state that "these are the only drugs that future patients will be treated with."43 The trial, launched in late 2018, was co-sponsored by DRC's national biomedical research institute and the U.S. National Institutes of Health, and was carried out by an international research consortium coordinated by the WHO.44
Issues for Congress
U.S. Funding for DRC Ebola Response
In FY2015, in the context of the West Africa outbreak, Congress appropriated $5.1 billion for Ebola response and preparedness on an emergency basis, including $1.436 billion in multiyear International Disaster Assistance (IDA) funds (Title IX of Division J, P.L. 113-235). U.S. funding for responding to the current outbreak has drawn primarily on the unobligated balance of these IDA funds. According to USAID, $105.5 million of these funds remained available for expenditure as of September 9, 2019.45 Should the outbreak continue or expand in new ways, Congress may consider what funding mechanisms, if any, the United States might use to support Ebola control. At the same time, the United States remains the lead country donor to the current Ebola response effort. Members may examine the U.S. role, vis-à-vis other actors (including other countries, multilateral entities, and private sources), in financing Ebola response activities, and may debate strategies for securing additional contributions from other donors.
U.S. Aid Restrictions Related to Trafficking in Persons
DRC is ranked as "Tier III" (worst) under the Trafficking Victims Protection Act (TVPA, P.L. 106-386, as amended), which triggers prohibitions on certain types of U.S. aid absent a full or partial presidential waiver. In FY2019, in a departure from previous practice, President Trump did not partially waive the restrictions for DRC.46 Thus, pursuant to the TVPA, no "nonhumanitarian, nontrade-related" assistance may be provided "to the government" of DRC.47
IDA funds, the core source of funding for U.S. Ebola response support to date, are exempt from the TVPA restrictions (22 U.S.C. §7102[10]). The TVPA further exempts economic and development assistance "in support of programs of nongovernmental organizations." In practice, the Administration has interpreted the TVPA restrictions to apply broadly to various programs funded through the Development Assistance (DA) and Economic Support Fund (ESF) accounts, including some that would be implemented by NGOs, though it has not publicly provided a full account of affected activities. Some Members of Congress have expressed concern that some U.S. assistance that could help promote humanitarian access in Ebola-affected areas has been held up as a result.48 Testifying before the Senate in July 2019, a senior USAID official affirmed that some FY2018 aid resources that could help with Ebola control remained restricted in connection with the TVPA, but he and other Administration witnesses did not provide further details.49
Two bills introduced in the 116th Congress (S. 1340, the Ebola Eradication Act of 2019, and H.R. 3085, a House companion bill) would authorize assistance for a range of activities that could help lower community resistance or otherwise support Ebola control efforts in DRC and neighboring states, "notwithstanding" the TVPA restrictions. S. 1340 passed the Senate on September 23, 2019. Similar language was included in a draft FY2020 State, Foreign Operations Appropriations bill circulated by the Senate Appropriations Committee on September 18, 2019. That bill would also broadly provide at least $298.3 million in U.S. bilateral assistance for "stabilization, global health, and bilateral economic assistance" to DRC—slightly higher than the U.S. allocation for DRC in recent years, not counting food aid—"including in areas affected by, and at risk from, the Ebola virus disease."
Global Health Security
The current Ebola outbreak has prompted resumption of discussions about strengthening health systems worldwide, particularly with regard to pandemic preparedness. In 2014, during the Obama Administration, the United States and the WHO co-launched the Global Health Security Agenda (GHSA) to improve countries' ability to prevent, detect, and respond to infectious disease threats.50 The United States, the largest donor to this multilateral effort, pledged to support it with $1 billion from FY2015 through FY2019. The Trump Administration has built on these efforts. In May 2019, the White House released the United States Government Global Health Security Strategy, which outlined the U.S. role in extending the Global Health Security Agenda and improving global health security worldwide.51 Although the Trump Administration, through the strategy and public statements, has supported extending the GHSA through 2024, officials have not provided comprehensive information on what that support would entail.
Members of Congress may continue to debate what role, if any, the United States should play in supporting global health system strengthening efforts to bolster global health security, and whether to adjust funding levels to meet ongoing and future infectious disease threats. Through regular appropriations, disease outbreak prevention and global health security efforts are funded through USAID pandemic influenza and CDC global health protection line items (Table 2).
|
FY2015 Enacted |
FY2016 Enacted |
FY2017 Enacted |
FY2018 Enacted |
FY2019 Enacted |
FY2020 Request |
|
|
CDC |
55.1 |
55.1 |
55.1 |
108.2 |
108.2 |
100.0 |
|
USAID |
72.5 |
72.5 |
72.5 |
72.5 |
100.0 |
90.0 |
Source: Created by CRS from appropriations legislation and congressional budget justifications.
Note: Excludes emergency Ebola appropriations.
On September 19, 2019, the House passed the Continuing Appropriations Act, 2020, and Health Extenders Act of 2019 (H.R. 4378), which would authorize the transfer to the CDC of up to $20 million for Ebola preparedness and response activities from the Infectious Disease Rapid Response Reserve Fund.52 Other relevant bills introduced in the 116th Congress include H.R. 2166, which would codify U.S. engagement in the GHSA as specified in an executive order issued by the Obama Administration,53 and H.R. 826, which seeks to facilitate research and treatment of neglected tropical diseases, including Ebola.
Author Contact Information
Footnotes
| 1. |
WHO, Ebola Virus Disease Democratic Republic of the Congo: External Situation Report 58, September 10, 2019. |
| 2. |
For more information on the 2014-2016 West Africa Ebola outbreak, see CRS Report R44507, Status of the Ebola Outbreak in West Africa: Overview and Issues for Congress, by Tiaji Salaam-Blyther, Susan B. Epstein, and Bolko J. Skorupski. |
| 3. |
As of October 2018 (before the outbreak had substantially spread), 4.3 million people were in need of humanitarian aid in the two provinces, according to U.N. Office for the Coordination of Humanitarian Affairs (UNOCHA) data. |
| 4. |
See CRS Report R43166, Democratic Republic of Congo: Background and U.S. Relations. |
| 5. |
WHO, "Ebola Virus Disease-Democratic Republic of the Congo," Disease Outbreak News, September 19, 2019. |
| 6. |
See, for example, House Foreign Affairs Subcommittee on Africa, Global Health, Global Human Rights and International Organizations ("HFAC Africa Subcommittee"), hearing, "Eradicating Ebola: Lessons Learned and Medical Achievements," June 4, 2019; and WHO, "High-Level Event on Ebola Virus Disease in DRC," July 15, 2019. |
| 7. |
Senate Appropriations Subcommittee on State, Foreign Operations, and Related Programs, hearing, "Review of the FY2020 Budget Request for USAID," April 30, 2019. |
| 8. |
Mark Green, "How to End the Ebola Crisis [Op-Ed]," CNN, August 22, 2019. |
| 9. |
See WHO, Cases of Undiagnosed Febrile Illness-United Republic of Tanzania, Disease Outbreak News, September 21, 2019. On September 14, Tanzanian officials reported to WHO that two suspected Ebola cases had tested negative for the virus. On September 19, WHO received information through unofficial channels that a contact of one of the cases deemed Ebola-negative had been hospitalized. WHO sent a verification request to which Tanzanian officials reported that there were no confirmed or suspected Ebola cases admitted anywhere. |
| 10. |
World Bank, World Bank Mobilizes US$300 Million to Finance the Ebola Response in Democratic Republic of Congo, July 24, 2019. |
| 11. |
WHO Ebola funding website, https://www.who.int/emergencies/diseases/ebola/drc-2019/funding, accessed on September 24, 2019. |
| 12. |
New York Times, "Ebola Outbreak Reaches Major City in Congo, Renewing Calls for Emergency Order," July 15, 2019. |
| 13. |
WHO, WHO Adapts Ebola Vaccination Strategy in the Democratic Republic of the Congo to Account for Insecurity and Community Feedback," News Release, May 7, 2019. |
| 14. |
Doctors Without Borders (MSF), "Independent Ebola Vaccination Committee Is Needed to Overcome Lack of WHO Transparency," Press Release, September 23, 2019. |
| 15. |
WHO, "Second Ebola Vaccine to Complement 'Ring Vaccination' Given Green Light in DRC," September 23, 2019; and Ebola Virus Disease, Democratic Republic of Congo, External Situation Report 58, September 10, 2019. |
| 16. |
WHO, "Ebola Outbreak in the Democratic Republic of the Congo," Press Briefing, June 6, 2019. |
| 17. |
New York Times, "In Congo, a New Plan to Fight Ebola Follows a Government Power Struggle," July 26, 2019. |
| 18. |
Testimony of USAID then-Acting Assistant Administrator Tim Ziemer before the House Foreign Affairs Subcommittee on Africa, Global Health, Global Human Rights and International Organizations, hearing, "Eradicating Ebola: Lessons Learned and Medical Advancements," June 4, 2019; Green, "How to End the Ebola Crisis," op. cit. |
| 19. |
WHO, United Nations Strengthens Ebola Response in Democratic Republic of the Congo, May 23, 2019. |
| 20. |
Ibid. |
| 21. |
Ziemer testimony before the HFAC Africa Subcommittee, "Eradicating Ebola," June 4, 2019, op. cit.; The New Humanitarian, "Q&A: Tackling Congo's Ebola Outbreak 'More Than a Public Health Response,'" July 11, 2019. |
| 22. |
World Bank, "Support to the 10th Ebola Outbreak in Democratic Republic of Congo," July 24, 2019. |
| 23. |
Developed in the aftermath of the 2014-2016 West Africa Ebola outbreak, the World Bank's PEF is designed to be an innovative and flexible source of financing to help the world's poorest countries respond to cross-border, large-scale disease outbreaks. See "Pandemic Emergency Financing Facility: Frequently Asked Questions," at https://www.worldbank.org/en/topic/pandemics/brief/pandemic-emergency-facility-frequently-asked-questions. |
| 24. |
World Bank, "The Pandemic Emergency Financing Facility pays out an additional US$30 million to support the Ebola response in the Democratic Republic of Congo," August 23, 2019. |
| 25. |
Africa CDC, "African Union To Deploy More Experts In Response To Ebola Outbreak in the DRC," July 19, 2019. |
| 26. |
USAID, Democratic Republic of the Congo – Ebola Outbreak, Fact Sheet #2, September 10, 2019. |
| 27. |
CRS correspondence with USAID on September 9, 2019. |
| 28. |
House Foreign Affairs Committee hearing on the FY2020 Foreign Assistance Budget, April 9, 2019. |
| 29. |
STAT, "CDC Director Says He Pushed to Keep U.S. Experts in Ebola Zone But Was Overruled," October 23, 2018. |
| 30. |
USAID, "Democratic Republic of the Congo – Ebola Outbreak," FY2019 Fact Sheet #2, September 10, 2019. |
| 31. |
See CRS Report R43166, Democratic Republic of Congo: Background and U.S. Relations, for background on the ADF, and on security conditions in eastern DRC more broadly. |
| 32. |
See, for example, Congo Research Group and Human Rights Watch, "Kivu Security Tracker," https://kivusecurity.org/map#. |
| 33. |
Congo Research Group, Who Are the Killers of Beni? March 2016. |
| 34. |
WHO, Press Conference on Ebola Disease Outbreak in the Democratic Republic of Congo, May 28, 2019. |
| 35. |
New York Times, "Ebola Outbreak Reaches Major City in Congo, Renewing Calls for Emergency Order," July 15, 2019. |
| 36. |
WHO, "As Ebola Cases Reach 3,000 in DRC, WHO Calls on All Partners to Fulfill Promises to Communities," August 29, 2019. |
| 37. |
Ibid. |
| 38. |
WHO, Ebola Virus Diseases, Democratic Republic of Congo, External Situation Report 42, May 21, 2019. |
| 39. |
The WHO does not regularly report on health worker deaths. The May 7 External Situation Report was the last report to include the number of deaths among health workers who contracted Ebola. WHO, "Ebola Virus Disease—Democratic Republic of Congo," Disease Outbreak News, July 11, 2019; and External Situation Report 40, May 7, 2019. The most recent count of health worker Ebola infections was reported in an August 29, 2019, Disease Outbreak News Report on the DRC. |
| 40. |
WHO, Press Conference on Ebola Disease Outbreak in the Democratic Republic of Congo, May 28, 2019. |
| 41. |
WHO, Ebola Virus Disease, Democratic Republic of Congo, External Situation Report 51, July 23, 2019. |
| 42. |
WHO, "Ebola Virus Disease-Democratic Republic of the Congo," Disease Outbreak News, September 19, 2019. |
| 43. |
WHO, "Update on Ebola Drug Trial: Two strong performers identified," August 12, 2019. |
| 44. |
National Institutes of Health, "Independent Monitoring Board Recommends Early Termination of Ebola Therapeutics Trial in DRC Because of Favorable Results with Two of Four Candidates," August 12, 2019. |
| 45. |
CRS correspondence with USAID on September 9, 2019. |
| 46. |
Presidential Determination No. 2017-15, September 30, 2017 (for FY2018); "Presidential Determination with Respect to the Efforts of Foreign Governments Regarding Trafficking in Persons," November 29, 2018 (for FY2019). |
| 47. |
Exceptions to the prohibition are further defined under 22 U.S.C. §7102, while certain other funds are authorized or appropriated "notwithstanding" other legal restrictions and may thus therefore be provided. See CRS Report R44953, The State Department's Trafficking in Persons Report: Scope, Aid Restrictions, and Methodology, by Liana W. Rosen. |
| 48. |
See, for example, Sen. Robert Menendez, Remarks in the Senate, Congressional Record, vol. 165 (2019), pp. S5294-S5295. |
| 49. |
Ziemer testimony before the Senate Foreign Relations Subcommittee on Africa and Global Health Policy, hearing on "Confronting Ebola: Addressing a 21st Century Global Health Crisis," July 24, 2019. |
| 50. |
For more information on the GHSA, see CRS In Focus IF10022, The Global Health Security Agenda and International Health Regulations, by Tiaji Salaam-Blyther. |
| 51. |
White House, United States Government Global Health Security Strategy, 2019. |
| 52. |
This Fund was established by §231 of the Department of Defense and Labor, Health and Human Services, and Education Appropriations Act, 2019 and Continuing Appropriations Act, 2019 (P.L. 115-245), which provided $50 million for activities "to prevent, prepare for, or respond to an infectious disease emergency." The funds were to remain available until expended and only to be used for an infectious disease emergency that (1) is declared by the Secretary of Health and Human Services (HHS); or (2) as determined by the Secretary, has significant potential to imminently occur and potential, on occurrence, to affect national security or the health and security of United States citizens, domestically or internationally. The Secretary of HHS has not declared that the ongoing Ebola outbreak in DRC is a threat to national security or to U.S. citizens to date, but §138 of H.R. 4378 would allow the transfer absent such a declaration. |
| 53. |
Executive Order 13747, "Advancing the Global Health Security Agenda to Achieve a World Safe and Secure from Infectious Disease Threats," 78701-78706 (2016). |