Military Medical Care: Frequently Asked Questions
Changes from November 8, 2018 to December 20, 2018
This page shows textual changes in the document between the two versions indicated in the dates above. Textual matter removed in the later version is indicated with red strikethrough and textual matter added in the later version is indicated with blue.
Contents
- Background
- Questions and Answers
- 1. How is the Military Health System Structured?
- MHS Governance Entities
- Defense Health Agency
- Military Service Medical Departments
- 2. How is the Military Health System Funded?
- 3. What is the Medicare-Eligible Retiree Health Care Fund (MERHCF)?
- 4. What is TRICARE?
- TRICARE Regional Managed Health Care Support Contracts
- 5. Who Is Eligible for TRICARE?
- 6. What are the Different TRICARE Plans?
- TRICARE Prime
- TRICARE Select
- TRICARE Reserve Select
- TRICARE Retired Reserve
- TRICARE Young Adult
- TRICARE for Life
- 7. When can beneficiaries enroll in or change their TRICARE plan?
- 8. What is the DOD Pharmacy Benefits Program?
- 9. What is the Extended Care Health Option (ECHO) Program?
- 10. How Are Priorities for Care in Military Treatment Facilities Assigned?
- 11. What are DOD's Access to Care Standards?
- 12. How Does the Patient Protection and Affordable Care Act Affect TRICARE?
- 13. How does TRICARE Determine its Reimbursement Rates?
- 14. What Health Benefits are Available to Reservists?
- 15. Have Military Personnel Been Promised Free Medical Care for Life?
- 16. What is the Congressionally Directed Medical Research Program?
- 17. Does TRICARE Cover Abortion?
- 18. Does DOD Use Animals in Medical Research or Training?
Figures
- Figure 1. Military Health System Governance
- Figure 2. Military Health System Organizational Structure through September 2021
- Figure 3. Military Health System Organizational Structure after September 2021
- Figure 4. FY2019 Unified Medical Budget Request
- Figure 5. TRICARE Regions in the United States
- Figure 6. Eligible Beneficiaries, FY2017
Tables
- Table 1. Cost Sharing Features for TRICARE Prime
- Table 2. Cost Sharing Features for TRICARE Select
- Table 3. Qualifying Life Events
- Table 4. TRICARE Pharmacy Copayments, 2018-2027
- Table 5. ECHO-Covered Services & Supplies
- Table 6. ECHO Monthly Cost Share
- Table 7. DOD Health Benefits Available to Members of the Reserve Component
- Table 8. Appropriation Levels for Selected CDMRP Research Areas, FY2014-FY2019
Appendixes
Summary
Military medical care is a congressionally authorized entitlement that has expanded in size and scope since the late 19th19th century. Chapter 55 of Title 10 U.S. Code, entitles certain health benefits to military personnel, retirees, and their families. These health benefits are administered by a Military Health System (MHS). The primary objectives of the MHS, which includes the Defense Department's hospitals, clinics, and medical personnel, are (1) to maintain the health of military personnel so they can carry out their military missions and (2) to be prepared to deliver health care during wartime. Health care services are delivered through either Department of Defense (DOD) medical facilities, known as military treatment facilities (MTFs) as space is available, or through civilian health care providers. As of 2017, the MHS operates 681 MTFs, employs nearly 63,000 civilians and 84,000 military personnel, and serves 9.4 million beneficiaries across the United States and in overseas locations.
Since 1966, civilian care for millions of retirees, as well as dependents of active duty military personnel and retirees, has been provided through a program still known in law as the Civilian Health and Medical Program of the Uniformed Services (CHAMPUS), more commonly known as TRICARE. TRICARE has three main benefit plans: a health maintenance organization option (TRICARE Prime), a preferred provider option (TRICARE Select), and a Medicare supplement option (TRICARE for Life) for Medicare-eligible retirees. Other TRICARE plans include TRICARE Young Adult, TRICARE Reserve Select, and TRICARE Retired Reserve. TRICARE also includes a pharmacy program and optional dental and vision plans. Options available to beneficiaries vary by the sponsor's duty status and geographic location.
This report answers selected frequently asked questions about military health care, including
- How is the Military Health System structured?
- What is TRICARE?
- What are the different TRICARE plans and who is eligible?
- What are the costs of military health care to beneficiaries?
- What is the relationship of TRICARE to Medicare?
- How does the Affordable Care Act affect TRICARE?
- When can beneficiaries change their TRICARE plan?
- What is the Medicare Eligible Retiree Health Care fund, which funds TRICARE for Life?
This report does not address issues specific to battlefield medicine, veterans, or the Veterans Health Administration. Veterans' health issues are addressed in CRS Report R42747, Health Care for Veterans: Answers to Frequently Asked Questions, by [author name scrubbed].
Military medical care is a congressionally authorized entitlement that has expanded in size and scope since the late 19th19th century. Chapter 55 of Title 10 U.S. Code, entitles certain health benefits to military personnel, retirees, and their families. These health benefits are administered by a Military Health System (MHS). The primary objectives of the MHS, which includes the Defense Department's hospitals, clinics, and medical personnel, are (1) to maintain the health of military personnel so they can carry out their military missions and (2) to be prepared to deliver health care during wartime. Health care services are delivered through either Department of Defense (DOD) medical facilities, known as military treatment facilities (MTFs) as space is available, or through civilian health care providers. As of 2017, the MHS operates 681 MTFs, employs nearly 63,000 civilians and 84,000 military personnel, and serves 9.4 million beneficiaries across the United States and in overseas locations.
Since 1966, civilian care for millions of retirees, as well as dependents of active duty military personnel and retirees, has been provided through a program still known in law as the Civilian Health and Medical Program of the Uniformed Services (CHAMPUS), more commonly known as TRICARE. TRICARE has three main benefit plans: a health maintenance organization option (TRICARE Prime), a preferred provider option (TRICARE Select), and a Medicare supplement option (TRICARE for Life) for Medicare-eligible retirees. Other TRICARE plans include TRICARE Young Adult, TRICARE Reserve Select, and TRICARE Retired Reserve. TRICARE also includes a pharmacy program and optional dental and vision plans. Options available to beneficiaries vary by the sponsor's duty status and geographic location.
This report answers selected frequently asked questions about military health care, including
- How is the Military Health System structured?
- What is TRICARE?
- What are the different TRICARE plans and who is eligible?
- What are the costs of military health care to beneficiaries?
- What is the relationship of TRICARE to Medicare?
- How does the Affordable Care Act affect TRICARE?
- When can beneficiaries change their TRICARE plan?
- What is the Medicare Eligible Retiree Health Care fund, which funds TRICARE for Life?
This report does not address issues specific to battlefield medicine, veterans, or the Veterans Health Administration. Veterans' health issues are addressed in CRS Report R42747, Health Care for Veterans: Answers to Frequently Asked Questions, by [author name scrubbed].
Military medical care is a congressionally authorized entitlement that has expanded in size and scope since the late 19th19th century. Chapter 55 of Title 10 U.S. Code, entitles certain health benefits to military personnel, retirees, and their families. These health benefits are administered by a Military Health System (MHS). The primary objectives of the MHS, which includes the Defense Department's hospitals, clinics, and medical personnel, are (1) to maintain the health of military personnel so they can carry out their military missions and (2) to be prepared to deliver health care during wartime. Health care services are delivered through either Department of Defense (DOD) medical facilities, known as military treatment facilities (MTFs) as space is available, or through civilian health care providers. As of 2017, the MHS operates 681 MTFs, employs nearly 63,000 civilians and 84,000 military personnel, and serves 9.4 million beneficiaries across the United States and in overseas locations.
Since 1966, civilian care for millions of retirees, as well as dependents of active duty military personnel and retirees, has been provided through a program still known in law as the Civilian Health and Medical Program of the Uniformed Services (CHAMPUS), more commonly known as TRICARE. TRICARE has three main benefit plans: a health maintenance organization option (TRICARE Prime), a preferred provider option (TRICARE Select), and a Medicare supplement option (TRICARE for Life) for Medicare-eligible retirees. Other TRICARE plans include TRICARE Young Adult, TRICARE Reserve Select, and TRICARE Retired Reserve. TRICARE also includes a pharmacy program and optional dental and vision plans. Options available to beneficiaries vary by the sponsor's duty status and geographic location.
This report answers selected frequently asked questions about military health care, including
- How is the Military Health System structured?
- What is TRICARE?
- What are the different TRICARE plans and who is eligible?
- What are the costs of military health care to beneficiaries?
- What is the relationship of TRICARE to Medicare?
- How does the Affordable Care Act affect TRICARE?
- When can beneficiaries change their TRICARE plan?
- What is the Medicare Eligible Retiree Health Care fund, which funds TRICARE for Life?
This report does not address issues specific to battlefield medicine, veterans, or the Veterans Health Administration. Veterans' health issues are addressed in CRS Report R42747, Health Care for Veterans: Answers to Frequently Asked Questions, by [author name scrubbed].
Background
Military medical care is a congressionally authorized entitlement that has expanded in size and scope since the late 19th century. Chapter 55 of Title 10 U.S. Code, entitles certain health benefits to military personnel, retirees, and their families. These health benefits are administered by a Military Health System (MHS). The primary objectives of the MHS, which includes the Defense Department's hospitals, clinics, and medical personnel, are (1) to maintain the health of military personnel so they can carry out their military missions and (2) to be prepared to deliver health care during wartime. The MHS is one of the largest health systems in the United States and serves over 9.4 million beneficiaries.1 The primary mission of the MHS is to maintain the health and wellness of military personnel so they can carry out their military missions, and to be prepared to deliver health care during wartime.2 This mission is further defined in law:
- "…to create and maintain high morale in the uniformed services by providing an improved and uniform program of medical and dental care for members and certain former members of those services, and their dependents."3
- "To support the medical readiness of the armed forces and the readiness of medical personnel…"4
- Perform medical research that is "of potential medical interest to the Department of Defense."5
- Conduct "humanitarian and civic assistance activities in conjunction with authorized military operations…"6
Health care within the MHS is delivered through either Department of Defense (DOD) medical facilities, known as military treatment facilities (MTFs) as space is available, or through civilian health care providers. The MHS operates 681 MTFs and employs nearly 63,000 civilians and 84,000 military personnel across the United States and in overseas locations.7
The MHS also covers dependents of active duty personnel, military retirees, and their dependents, including some members of the reserve components. Since 1966, civilian healthcarehealth care to millions of retirees, as well as dependents of active duty military personnel and retirees, has been provided through a program still known in law as the Civilian Health and Medical Program of the Uniformed Services (CHAMPUS), but more commonly known as TRICARE.8 A Medicare wrap-around option (TRICARE for Life) for Medicare-eligible retirees was added in 2002. Other TRICARE plans include TRICARE Young Adult, TRICARE Reserve Select, and TRICARE Retired Reserve. TRICARE also includes a pharmacy program, optional dental plans, and a vision plan that are to be made available for certain beneficiaries in 2019. Options available to beneficiaries vary by the sponsor's duty status and geographic location.
Questions and Answers
1. How is the Military Health System Structured?
The MHS is administered by five primary DOD organizations: Office of the Assistant Secretary of Defense for Health Affairs (ASD(HA)), Defense Health Agency (DHA), Army Medical Command (MEDCOM), Navy Bureau of Medicine and Surgery (BUMED), and Air Force Medical Service (AFMS). Each maintains separate and distinct responsibilities in executing the primary mission of the MHS. In general, the development of MHS-wide policies, budget administration, and oversight activities are assigned to the Office of the ASD(HA), while policy execution functions and the delivery of health care is assigned to the DHA and the Service medical departments. Despite being administered by various DOD entities, a governance structure has been established to facilitate the decision-making process, maintain oversight of DOD health care, and coordinate health programs, services, and benefits.
MHS Governance Entities
Military Health System Executive Review (MHSER)
The MHSER serves as a senior-level forum for DOD leadership input on strategic, transitional, and emerging issues. The MHSER advises the Office of the Secretary of Defense (SECDEF) and the Office of the Deputy Secretary of Defense (DEPSECDEF) about performance challenges and direction. The MHSER is comprised of the following senior DOD leaders:
- Under Secretary of Defense (Personnel and Readiness) (USD(P&R)) (Chair);
- Principal Deputy Under Secretary of Defense (Personnel and Readiness);
- ASD(HA);
- Military Service Vice Chiefs (including the Assistant Commandant of the Marine Corps);
- Military Department Assistant Secretaries for Manpower and Reserve Affairs;
- Director of Cost Assessment and Program Evaluation;
- Principal Deputy Under Secretary of Defense (Comptroller);
- Director of the Joint Staff; and
- Military Service Surgeons General (ex-officio members).9
Senior Military Medical Action Council (SMMAC)
The SMMAC is the highest governing body in the MHS, which presents enterprise-level guidance and operational issues for decision-making by the ASD(HA). The following senior military health leaders are members of the SMMAC:
- ASD(HA) (Chair);
- Principal Deputy Assistant Secretary of Defense (Health Affairs) (PDASD(HA));
- Military Service Surgeons General;
- DHA Director;
- Joint Staff Surgeon; and
- other attendees as required.10
Medical Deputies Action Group (MDAG)
Reporting to the SMMAC is the MDAG, which ensures that actions are coordinated and aligned with MHS strategy, policies, directives, and initiatives. The MDAG is comprised of:
- PDASD(HA) (Chair);
- Military Service Deputy Surgeons General;
- DHA Deputy Director; and
- Joint Staff Surgeon Representative.11
Reporting to the MDAG are four supporting governing bodies:
- The Medical Operations Group (MOG) consists of the senior
healthcarehealth care operations directors of the Service medical departments, the DHA Director of Healthcare Operations, and a Joint Staff Surgeon representative, with the chairmanship rotating among these members. The MOG carries out MDAG assigned tasks and provides a collaborative and transparent forum supporting enterprise-wide oversight of direct and purchased care systems focused on sustaining and improving the MHS.12 - The Medical Business Operations Group (MBOG) consists of the senior resource managers of the Service medical departments and the DHA Director of Business Operations, with the chairmanship rotating among these members. The MBOG provides a forum for providing resource management input to the MDAG on direct and purchased care issues and initiatives focused on sustaining and improving the MHS.13
- The Manpower and Personnel Operations Group (MPOG) consists of the senior human resources and manpower representatives from the Service medical departments and the DHA, with the chairmanship rotating among these members. The MPOG supports centralized, coordinated policy execution, and guidance for development of coordinated human resources and manpower policies and procedures for the MHS.14
- The Enhanced Multi-Service Markets (eMSM) Leadership Group. eMSMs are geographic MHS markets served by more than one military department under the direction of a designated Market Manager (typically a general or flag officer) with limited authorities.15 The six eMSMs are:
- 1. Tidewater, Virginia
- 2. Puget Sound, Washington
- 3. Colorado Springs, Colorado
- 4. San Antonio, Texas
- 5. Oahu, Hawaii
- 6. National Capital Region
- The eMSM Leadership Group is composed of the six Market Managers with the chairmanship rotating among these members. The eMSM Leadership Group provides a forum for eMSM Managers to discuss clinical and business issues, policies, performance standards, and opportunities.16
Finally, the ASD(HA) is supported and advised by the Policy Advisory Council (PAC), composed of the Deputy Assistant Secretaries of Defense (Health Affairs), DHA Deputy Director, Deputy Surgeons General, and a representative of the Joint Staff. The PAC provides a forum for supporting MHS-wide policy development and oversight in a unified manner.17
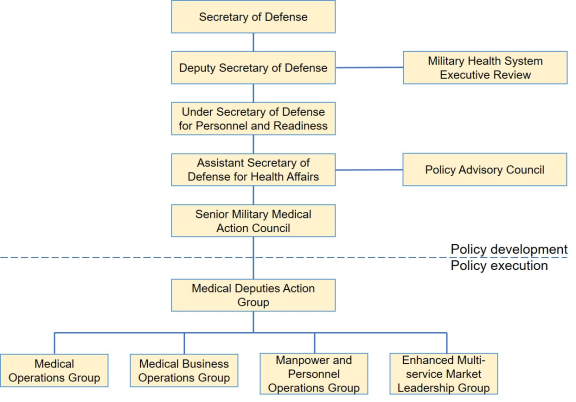 |
|
Source: Department of Defense, 2018. Notes: Adapted by CRS. |
Defense Health Agency
The DHA is a designated Combat Support Agency that focuses on enabling medical readiness of the Armed Forces and delivering a ready medical force to Combatant Commanders during peacetime and wartime.18 Established in September 2013, the role of DHA is to:
- manage the TRICARE program;
- manage and execute the Defense Health Program appropriation and the Medicare Eligible Retiree Health Care Fund (MERHCF);
- support coordinated management of the eMSMs to create and sustain a cost-effective, coordinated, and high-quality health care system;
- exercise management responsibility for shared services, functions, and activities of the MHS;
- exercise authority, direction, and control over MTFs within the National Capital Region;19
;and - support the effective execution of the DOD medical mission.20
The DHA Director leads the organization and is appointed by and reports to the ASD(HA). The Director is typically a general or flag officer in the grade of Lieutenant General/Vice Admiral.
On October 1, 2018, the military service medical departments began transferring the responsibilities to administer and manage each MTF to the DHA, as directed by sectionSection 702 of the National Defense Authorization Act (NDAA) for Fiscal Year 2017 (P.L. 114-328). The first wave of MTFs transferred to the DHA include:
- Womack Army Medical Center and all associated clinics;
- Naval Hospital Jacksonville and all associated clinics;
- 81st Medical Group;
- 4th Medical Group; and
- 43rd Medical Squadron.21
The transfer of these responsibilities is required to be completed no later than September 30, 2021.22
Military Service Medical Departments
The military service medical departments (i.e., MEDCOM, BUMED, AFMS) are established under each respective military department to organize, train, and equip military medical personnel, maintain medical readiness of the Armed Forces, and administer, manage, and provide health care in MTFs. The medical departments are led by a Surgeon General,23, who also functions as the principal advisor to their respective military service secretary and service chief for all health and medical matters.24
|
Figure 2. Military Health System Organizational Structure through September 2021 |
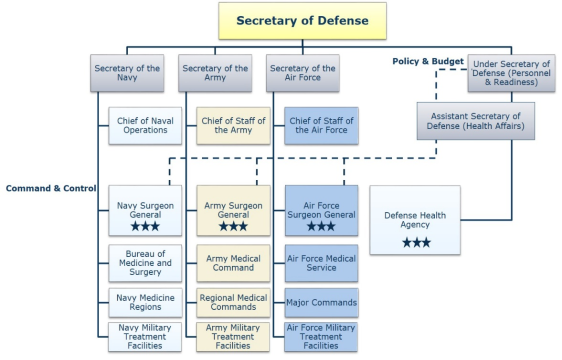 |
|
Source: Department of Defense, 2018. Notes: Adapted by CRS. |
After September 30, 2021, the military departments are no longer to administer and manage MTFs; instead, they are to focus on other statutory responsibilities (e.g., medical readiness, providing DHA with medical personnel to staff MTFs, providing medical personnel to support combatant commander requirements).25
|
Figure 3. Military Health System Organizational Structure after September 2021 |
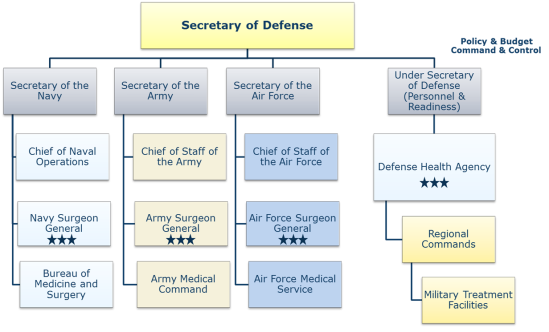 |
|
Source: Department of Defense, 2018. Notes: Adapted by CRS. |
2. How is the Military Health System Funded?
The ASD(HA) prepares and submits a unified medical budget that includes resources for the medical activities under his or her control within DOD. The unified medical budget is primarily discretionary funding for all fixed MTFs and military medical activities, including costs for real property maintenance, environmental compliance, minor construction, base operations support, health care delivery, and medical personnel. Accrual payments to the Medicare Eligible Retiree Health Care Fund (MERHCF) are also included as mandatory spending.26 The unified medical budget does not include funding associated with combat support medical units/activities; in these instances the funding responsibility is assigned to combatant or military service commands.
Unified medical budget funding has traditionally been appropriated through the following means:
- The defense appropriations bill provides Operation and Maintenance (O&M), Procurement, and Research, Development, Test and Evaluation (RDT&E) funding under the heading Defense Health Program.
- Funding for military medical personnel (doctors, nurses, medics, technicians, and other health care providers) and TRICARE for Life accrual payments are generally provided in the defense appropriations bill under the Military Personnel (MILPERS) title.
- Funding for medical military construction (MILCON) is generally provided under the Department of Defense title of the Military Construction and Veterans Affairs bill.
- A standing authorization for transfers from the MERHCF to reimburse TRICARE for the cost of services provided to Medicare eligible retirees is provided by 10 U.S.C. §1113 as mandatory spending.
- Costs of war-related military health care are generally funded through supplemental appropriations bills.
Other resources are made available to the MHS from third-party collections27 authorized by 10 U.S.C. §1097b(b) and a number of other reimbursable program and transfer authorities.
As illustrated in Figure 4 the Trump Administration's FY2019 unified medical budget request totals $50.6 billion and includes the following: 28
- $33.7 billion for the DHP;
- $8.9 billion for MILPERS;
- $0.4 billion for medical MILCON; and
- $7.5 billion for accrual payments to the MERHCF.
|
Figure 4. FY2019 Unified Medical Budget Request (billions) |
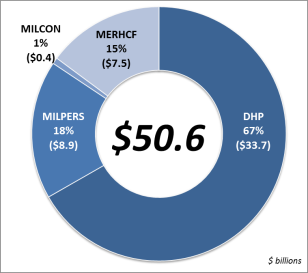 |
|
Source: Department of Defense, FY 2019 Budget Request Overview, February 2018, p. 5-4. Notes: Graphic adapted by CRS. |
3. What is the Medicare-Eligible Retiree Health Care Fund (MERHCF)?
The Floyd D. Spence NDAA for FY2001 directed the establishment of the Medicare-Eligible Retiree Health Care Fund to pay for Medicare-eligible retiree health care beginning on October 1, 2002, via a new program called TRICARE for Life.29 Prior to this date, Medicare-eligible beneficiaries could only receive space-available care in an MTF. The MERHCF covers Medicare-eligible beneficiaries, regardless of age.
The FY2001 NDAA also established an independent three-member DOD Medicare-Eligible Retiree Health Care Board of Actuaries appointed by the Secretary of Defense. Accrual deposits into the MERHCF are made by the agencies that employ future beneficiaries of the uniformed services based upon estimates of future TRICARE for Life expenses.30 Transfers out are made to the Defense Health Program based on estimates of the cost of care actually provided each year. As of September 30, 2016, the Fund had assets of over $239.3 billion to cover future expenses.31
The Board is required to review the actuarial status of the fund, report annually to the Secretary of Defense, and report to the President and Congress on the status of the fund at least every four years. The DOD Office of the Actuary provides all technical and administrative support to the Board. The Secretary of Defense delegates operational oversight responsibilities and management of the MERHCF to the ASD(HA). The Defense Finance and Accounting Service provides accounting and investment services for the Fund.
4. What is TRICARE?
TRICARE is a health insurance-like program that pays for care delivered by civilian providers. TRICARE has three main benefit plans: a health maintenance organization option (TRICARE Prime), a preferred provider option (TRICARE Select), and a Medicare wrap-around option (TRICARE for Life) for Medicare-eligible retirees. Other TRICARE plans include TRICARE Young Adult, TRICARE Reserve Select, and TRICARE Retired Reserve. TRICARE also includes a pharmacy program and optional dental or vision plans. Options available to beneficiaries vary by the beneficiary's relationship to a sponsor, sponsor's duty status, and geographic location.
The foundations of TRICARE began with the Dependents Medical Care Act of 1956 (P.L. 84-569), which provided a statutory basis for dependents of active duty members, retirees, and dependents of retirees to seek care at MTFs. The 1956 act allowed DOD to contract for a health insurance plan for coverage of civilian hospital services for active duty dependents. Due to growing use of MTFs by eligible civilians and resource constraints, Congress adopted the Military Medical Benefits Amendments in 1966 (P.L. 89-614), which allowed DOD to contract with civilian health providers to provide non-hospital-based care to eligible dependents and retirees. Since 1966, civilian care to millions of retirees and dependents of active duty military personnel and retirees has been provided through a program still known in law as the Civilian Health and Medical Program of the Uniformed Services (CHAMPUS), but since 1994 more commonly known as TRICARE.32
TRICARE Regional Managed Health Care Support Contracts
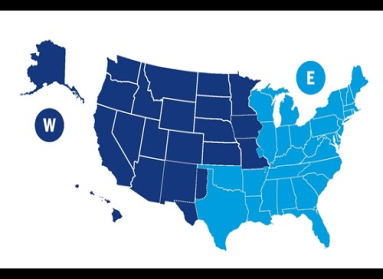
TRICARE within the United States (not including certain U.S. commonwealths or territories) is overseen by two TRICARE regional offices and administered through two managed care support contracts. Each contractor is required to perform the following functions: claims processing, management of enrollment processes, health care finder and referral services, establishment and maintenance of adequate provider networks, customer services for beneficiaries and network providers, and medical management of certain beneficiary populations.33
- TRICARE Regional Office – East oversees the East Region, which includes Alabama, Arkansas, Connecticut, Delaware, the District of Columbia, Florida, Georgia, Illinois, Indiana, Kentucky, Louisiana, Maine, Maryland, Massachusetts, Michigan, Mississippi, New Hampshire, New Jersey, New York, North Carolina, Ohio, Oklahoma, Pennsylvania, Rhode Island, South Carolina, Vermont, Virginia, West Virginia, Wisconsin, and portions of Iowa, Missouri, Tennessee, and most of Texas. The TRICARE East regional contractor is Humana Military.
- TRICARE Regional Office – West oversees the West Region, which includes Alaska, Arizona, California, Colorado, Hawaii, Idaho, most of Iowa, Kansas, Minnesota, most of Missouri, Montana, Nebraska, Nevada, New Mexico, North Dakota, Oregon, South Dakota, western portions of Texas, Utah, Washington, and Wyoming. The TRICARE West regional contractor is HealthNet Federal Services.
 |
|
Source: Department of Defense, Defense Health Agency, TRICARE Regions, accessed August 9, 2018, https://www.tricare.mil/About/Regions. Notes: Graphic adapted from the Defense Health Agency. |
These two contracts were re-competed in 2015, and after resolving bid protests, the new contracts known as T-2017 became operational in 2017.34 Health care delivery under the T-2017 contracts began on January 1, 2018.
TRICARE outside of the United States (including certain U.S. commonwealths and territories) is overseen by the TRICARE Overseas Program Office and administered by the health services support contractor, International SOS.
5. Who Is Eligible for TRICARE?
Eligibility for TRICARE is determined by the uniformed services and recorded in the Defense Enrollment Eligibility Reporting System (DEERS). All eligible beneficiaries must have their eligibility status recorded in DEERS.
TRICARE beneficiaries can be divided into two main categories: sponsors and dependents. Sponsor refers to the person who is serving or who has served on active duty or in the National Guard or Reserves. Dependent is defined in 10 U.S.C. §1072 and includes a variety of familial relationships, (e.g., spouses (including same-sex spouses), children, certain unremarried former spouses, and dependent parents).
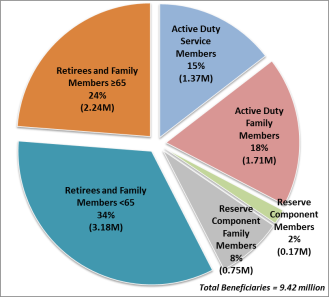
Figure 6 illustrates the major categories of eligible beneficiaries.
 |
|
Source: Defense Health Agency, Evaluation of TRICARE Program: Fiscal Year 2018 Report to Congress, Washington, DC, 2018, p. 18. |
6. What are the Different TRICARE Plans?
TRICARE Prime
TRICARE Prime is a managed health care option similar to a health maintenance organization (HMO) program. This plan features a military or civilian primary care provider who manages a beneficiary's overall health care and facilitates referrals to specialists. Referrals generally are required for specialty care visits. Enrollees receive first priority for appointments at MTFs and pay less out of pocket than beneficiaries who use the other TRICARE plans. TRICARE Prime does not have an annual deductible.
Active duty service membersservicemembers are required to use TRICARE Prime. Active duty service membersservicemembers, their dependents, and transitional survivors35 are exempt from the annual enrollment fee. Retired service membersservicemembers, their families, survivors of active duty service membersservicemembers, eligible former spouses, and others are required to pay an annual enrollment fee, which is applied to the annual catastrophic cap.36.
TRICARE Prime is offered only in geographic areas designated as a Prime Service Area (PSA). PSAs are typically near an MTF and former military locations subjected to Base Realignment and Closure (BRAC).37
Table 1 outlinesshows the costs and fees associated with TRICARE Prime.
|
Group Aa |
Group Bb |
|
|
Annual Enrollment Fee |
ADSMs, ADFMs, Transitional Survivors: $0 Retirees, their families, others: $ $ |
ADSMs, ADFMs, Transitional Survivors: $0 Retirees, their families, others: $ $ |
|
Annual Deductible |
$0 |
$0 |
|
Preventive Care Visit |
ADSMs, ADFMs, Transitional Survivors: $0 Retirees, their families, others: $0 |
ADSMs, ADFMs, Transitional Survivors: $0 Retirees, their families, others: $0 |
|
Primary Care Outpatient Visit |
ADSMs, ADFMs, Transitional Survivors: $0 Retirees, their families, others: $20 |
ADSMs, ADFMs, Transitional Survivors: $0 Retirees, their families, others: $20 |
|
Specialty Care Outpatient Visit |
ADSMs, ADFMs, Transitional Survivors: $0 Retirees, their families, others: $30 |
ADSMs, ADFMs, Transitional Survivors: $0 Retirees, their families, others: $30 |
|
Urgent Care Center Visit |
ADSMs, ADFMs, Transitional Survivors: $0 Retirees, their families, others: $30 |
ADSMs, ADFMs, Transitional Survivors: $0 Retirees, their families, others: $30 |
|
Emergency Room Visit |
ADSMs, ADFMs, Transitional Survivors: $0 Retirees, their families, others: $ |
ADSMs, ADFMs, Transitional Survivors: $0 Retirees, their families, others: $ |
|
Inpatient Admission (Hospitalization) |
ADSMs, ADFMs, Transitional Survivors: $0 Retirees, their families, others: $ |
ADSMs, ADFMs, Transitional Survivors: $0 Retirees, their families, others: $ |
|
Maximum Annual Out-of-Pocket Charge (Catastrophic Cap) |
ADSMs $0 ADFMs, Transitional Survivors: $1,000 per family Retirees, their families, others: $3,000 per family |
ADSMs $0 ADFMs, Transitional Survivors: $1, Retirees, their families, others: $3, |
Source: Department of Defense, TRICARE Costs and Fees 2019, November, May 2018, https://www.tricare.mil/-/media/Files/TRICARE/Publications/Misc/Costs_Sheet.pdf?la=en&hash=4A7B695166EEF6BB88606FB836D5DDB4D7DC92701BEEAAA91DC205AFD2DE7C14Costs_Sheet_2019.pdf?la=en&hash=10163205984EF86728CAE4BF3B335E02C1E4D88494A1134B03986A00403A2D02.
Notes: ADSM = active duty service member; ADFM = active duty family member.
a. Group A includes beneficiaries whose uniformed services sponsor entered initial military service prior to January 1, 2018.
b. Group B includes beneficiaries whose uniformed services sponsor entered initial military service on or after January 1, 2018.
TRICARE Select
TRICARE Select is a self-managed, preferred provider option (PPO) available worldwide for eligible beneficiaries. Active duty service membersservicemembers and TRICARE for Life beneficiaries are not eligible for this plan. TRICARE Select allows beneficiaries greater flexibility in managing their own health care and do not require a referral for specialty care. This plan allows enrollees to use authorized, non-network civilian providers, but at a higher out of pocket cost than using a network civilian provider. Some services may require prior authorization (e.g., hospice care, home health services, applied behavioral analysis).
TRICARE Select features an annual enrollment fee, deductibles, and fixed co-pays when receiving care from a network provider or paying a percentage of the allowable charge when receiving care from a TRICARE-authorized, non-network provider. Eligible beneficiaries residing outside of the United States may still enroll in TRICARE Select, however the availability of network providers may be limited based on geographic location.
Table 2 outlines the costs and fees associated with TRICARE Select.
|
Group Aa |
Group Bb |
|
|
Annual Enrollment Fee |
ADFMs, Transitional Survivors: $0 Retirees, their families, others: $0 |
ADFMs, Transitional Survivors: $0 Retirees, their families, others: $ $ |
|
Annual Deductible |
Sponsor is E-4 and below $50 (Individual) $100 (Family) Sponsor is E-5 and above $150 (Individual) $300 (Family) Retirees, their families, others: $150 (Individual) $300 (Family) |
Sponsor is E-4 and below $ $ Sponsor is E-5 and above $ $ Retirees, their families, others: $ $ |
|
Preventive Care Visit |
ADFMs, Transitional Survivors: $0 Retirees, their families, others: $0 |
ADFMs, Transitional Survivors: $0 Retirees, their families, others: $0 |
|
Primary Care Outpatient Visit |
ADFMs, Transitional Survivors: $21 Network 20%c Non-Network Retirees, their families, others: $ 25%c Non-Network |
ADFMs, Transitional Survivors: $15 Network 20%c Non-Network Retirees, their families, others: $25 Network 25%c Non-Network |
|
Specialty Care Outpatient Visit |
ADFMs, Transitional Survivors: $31 Network 20%c Non-Network Retirees, their families, others: $41 Network 25%c Non-Network |
ADFMs, Transitional Survivors: $25 Network 20%c Non-Network Retirees, their families, others: $ 25%c Non-Network |
|
Urgent Care Center Visit |
ADFMs, Transitional Survivors: $21 Network 20%c Non-Network Retirees, their families, others: $ 25%c Non-Network |
ADFMs, Transitional Survivors: $20 Network 20%c Non-Network Retirees, their families, others: $ 25%c Non-Network |
|
Emergency Room Visit |
ADFMs, Transitional Survivors: $ 20%c Non-Network Retirees, their families, others: $ 25%c Non-Network |
ADFMs, Transitional Survivors: $ 20%c Non-Network Retirees, their families, others: $ 25%c Non-Network |
|
Inpatient Admission (Hospitalization) |
ADFMs, Transitional Survivors: $ (whichever is greater) Retirees, their families, others: $250/day or up to 25% hospital charge (whichever is less); plus 20% separately billed services; Network $ |
ADFMs, Transitional Survivors: $ $20%c Non-Network Retirees, their families, others: $ 25%c Non-Network |
|
Inpatient Admission (MTF Hospitalization) |
$ |
|
|
Maximum Annual Out-of-Pocket Charge (Catastrophic Cap) |
ADSMs $0 ADFMs, Transitional Survivors: $1,000 per family Retirees, their families, others: $3,000 per family |
ADSMs $0 ADFMs, Transitional Survivors: $1, Retirees, their families, others: $3, |
Source: Department of Defense, TRICARE Costs and Fees 2019, November, May 2018, https://www.tricare.mil/-/media/Files/TRICARE/Publications/Misc/Costs_Sheet.pdf?la=en&hash=4A7B695166EEF6BB88606FB836D5DDB4D7DC92701BEEAAA91DC205AFD2DE7C14.
Notes: Network means a provider in the TRICARE network. Non-Network means a TRICARE-authorized provider not in the TRICARE network. ADSM = active duty service member; ADFM = active duty family member.
a. Group A includes beneficiaries whose uniformed services sponsor entered initial military service prior to January 1, 2018.
b. Group B includes beneficiaries whose uniformed services sponsor entered initial military service on or after January 1, 2018.
c. Percentage of TRICARE maximum-allowable charge after deductible is met.
TRICARE Reserve Select
The TRICARE Reserve Select (TRS) program was authorized by sectionSection 701 of the Ronald W. Reagan NDAA for FY2005 (P.L. 108-375).38 TRS is a premium-based health plan available worldwide for qualified Selected Reserve members of the Ready Reserve and their families.39 Servicemembers39. Service members are not eligible for TRS if they are on active duty orders, covered under the Transitional Assistance Management Program,40, eligible for or enrolled in the Federal Employees Health Benefits Program (FEHBP), or currently covered under the FEHBP through a family member.41
In general, TRS mirrors the benefits, costs, and fees established for TRICARE Select. The government subsidizes the cost of the program with members paying 28% of the cost of the program in the form of premiums. For CY2018CY2019, the monthly premiums are $46.0942.83 for member-only and $221.38218.01 for member and family coverage.42
TRICARE Retired Reserve
Section 705 of the NDAA for FY2010 (P.L. 111-84) authorized a TRICARE coverage option for so-called gray area reservists, defined as those who have retired but are too young to draw retirement pay.43,44 The program established under this authority is known as TRICARE Retired Reserve (TRR). Previously, such individuals were not eligible for any TRICARE coverage.
TRR is a premium-based health plan that qualified retired members of the National Guard and Reserve under the age of 60 may purchase for themselves and eligible family members. TRR differs from TRS in that there is no government subsidy. As such, retired Reserve Component members who elect to purchase TRICARE Retired Reserve must pay the full cost of the calculated premium plus an additional administrative fee. For CY2018CY2019, the monthly premiums are $431.35451.51 for member-only and $1,038.31083.40 for member and family coverage.45 Upon reaching the age of 60, retired Reserve Component members and their eligible family members become eligible to purchase TRICARE Prime or TRICARE Select.
TRICARE Young Adult
Section 702 of the Ike Skelton NDAA for Fiscal Year 2011 (P.L. 111-383) extended TRICARE eligibility for dependents, allowing unmarried children up to age 26, who are not otherwise eligible to enroll in an employer-sponsored plan, to purchase TRICARE coverage.46 The option established under this authority is known as TRICARE Young Adult (TYA). Unlike insurance coverage mandated by the Patient Protection and Affordable Care Act (P.L. 111-148), TYA provides individual coverage, rather than coverage under a family plan. A separate premium is charged. The law requires payment of a premium equal to the cost of the coverage as determined by the Secretary of Defense on an appropriate actuarial basis.47 For CY2018CY2019, the monthly premiums are $324358 for TYA Prime and $225214 TYA Select.48
TRICARE for Life
TRICARE for Life (TFL) was created as supplemental coverage for Medicare-eligible military retirees by sectionSection 712 of the Floyd D. Spence NDAA for FY2001 (P.L. 106-398). TFL functions as a secondary payer, or wrap-around, to Medicare. As a wrap-around, TFL will pay the out of pocket costs for Medicare-covered services as well as those only covered by TRICARE. Prior to the creation of TFL, coverage for Medicare-eligible individuals was limited to space-available care in MTFs. TFL cost sharing for beneficiaries is limited and there is no enrollment charge or premium.
To participate in TFL, TRICARE-eligible beneficiaries must enroll in and pay monthly premiums for Medicare Part B.49 TRICARE-eligible beneficiaries who are entitled to Medicare Part A based on age, disability, or diagnosis of End Stage Renal Disease (ESRD), but decline Part B, lose eligibility for TRICARE benefits.50 Individuals who choose not to enroll in Medicare Part B upon becoming eligible may elect to do so later during the special enrollment period or an annual enrollment period; however, the Medicare Part B late enrollment penalty may apply (Seesee question "12. How Does the Patient Protection and Affordable Care Act Affect TRICARE?").51
7. When can beneficiaries enroll in or change their TRICARE plan?
In general, eligible beneficiaries may enroll in a TRICARE health plan during the annual open enrollment season (November 12-December 12), or within 90 days after a Qualifying Life Event (QLE).52 Table 3 identifies military or family-related life changes that are deemed a QLE:
|
Military Changes |
Family Changes |
|
|
Source: 32 C.F.R. §199.17(o).
Notes: Adapted by CRS.
8. What is the DOD Pharmacy Benefits Program?
Section 701 of the NDAA for FY2000 (P.L. 106-65) directed the creation of an "effective, efficient, integrated pharmacy benefits program," also known as the DOD pharmacy benefits program.53 Features of the program include:
- Availability of pharmaceutical agents for all therapeutic classes;
- Establishing a uniform formulary based on clinical effectiveness and cost-effectiveness; and
- Assuring the availability of clinically appropriate pharmaceutical agents to uniformed services members, retirees, and family members.
The program dispenses pharmaceuticals to eligible beneficiaries through three venues: MTF pharmacies, TRICARE retail pharmacies, and the TRICARE Mail Order Program. Currently, MTF pharmacies are administered and managed by each military service medical department (i.e., MEDCOM, BUMED, and AFMS), while the TRICARE retail and mail order pharmacy programs are managed by the DHA. Since 2003, DOD has contracted a pharmacy benefits manager, Express Scripts, Inc. (ESI), to administer the TRICARE pharmacy programs.54 ESI maintains a national network of retail pharmacies and a home-delivery program and it processes pharmacy claims on behalf of beneficiaries. There are no additional costs to participate in the DOD pharmacy benefits program.
The program is required to maintain a formulary of pharmaceutical agents (hereinafter also referred to as drugs or medications) in the complete range of therapeutic classes. This is known as the Uniform Formulary. Selection of drugs for inclusion on the formulary is based on the relative clinical and cost effectiveness of the agents in each class.55 The law further specifies that the formulary is to be maintained and updated by a Pharmacy and Therapeutics Committee whose membership is composed of representatives of both MTF pharmacies and health care providers.56
A Beneficiary Advisory Panel (BAP) is required to review and comment on formulary recommendations presented by the Pharmacy and Therapeutics Committee prior to those recommendations going to the DHA Director for approval. 57 The BAP is composed of representatives of non-governmental organizations and associations that represent the views and interests of a large number of eligible covered beneficiaries, contractors responsible for the TRICARE retail pharmacy program, contractors responsible for the national mail-order pharmacy program, and TRICARE network providers.
Prescriptions Filled through Military Treatment Facilities
At an MTF, TRICARE beneficiaries may fill prescriptions from a civilian or military provider without a copayment. Enrollment in a specific TRICARE plan is not required to fill a prescription at an MTF. As of June 2018, 167 MTF pharmacies accept electronic prescriptions from civilian health care providers.58
MTFs are required to stock a subset of the Uniform Formulary known as the Basic Core Formulary. Additional drugs on the Uniform Formulary may also be carried by individual MTFs in order to meet local requirements. Non-formulary drugs are generally not available through MTFs. Certain Uniform Formulary-covered pharmaceuticals, however, may not be carried due to national contracts with pharmaceutical manufacturers.59 The DHA's Pharmacy Operations Division collaborates with the Defense Supply Center Philadelphia (DSCP) in coordination with the Department of Veterans Affairs (VA) Pharmacy Benefits Management Strategic Health Group and the VA National Acquisition Center in Hines, Illinois, in developing contracting strategies and technical evaluation factors for national pharmaceutical contracting initiatives.60
Prescriptions Filled through Retail Pharmacies
TRICARE beneficiaries may also fill prescriptions through retail pharmacies. DOD contracts for a TRICARE pharmacy benefit manager to administer both the retail and mail order options. The current contractor is ESI, to which DOD awarded a seven-year contract in 2014.61 Among other matters, ESI maintains a national network of retail pharmacies that beneficiaries may use without having to file a claim for reimbursement. Beneficiaries may also use non-network pharmacies. However, at non-network pharmacies, beneficiaries pay the full price of the medication up front and then file a claim for reimbursement.
DOD requires prescriptions to be filled with generic drugs when available.62 These are defined as medications approved by the Food and Drug Administration that are clinically the same as brand-name medications. Brand-name drugs that have a generic equivalent are only dispensed after the prescribing provider completes a clinical assessment that indicates the brand-name drug should be used in place of the generic medication and ESI grants approval.
Prescriptions Filled by Mail Order
TRICARE beneficiaries may arrange for home delivery of prescription drugs through the mail by registering with ESI. DOD negotiates drug prices with pharmaceutical manufacturers. The prices for drugs dispensed by mail order are considerably lower than drugs dispensed through retail pharmacies. Use of home delivery by TRICARE beneficiaries increased by 23% from FY2013 to FY2017.63 DOD attributes this increase to the education campaign it launched in 2009, copayment adjustments that incentivize the mail order program, and a pilot program that requires TFL beneficiaries to obtain brand-name maintenance medication refills through home delivery or MTF pharmacies.64
Copayment Adjustments
Section 702 of the NDAA for FY2018 (P.L. 115-91) adjusted pharmacy copayment amounts. The copayment amounts for 2018 to 2027 are codified in 10 U.S.C. §1074g(a) and are listed in Table 4. After 2027, the Secretary of Defense is authorized to set and adjust cost sharing amounts to "reflect changes in the costs of pharmaceutical agents and prescription dispensing, rounded to the nearest dollar."65
|
Retail Generic (30-day supply) |
Retail Brand (30-day supply) |
Mail Order Generic (90-day supply) |
Mail Order Brand (90-day supply) |
Mail Order Non-Formulary (90-day supply) |
|
|
2018 |
$11 |
$28 |
$7 |
$24 |
$53 |
|
2019 |
$11 |
$28 |
$7 |
$24 |
$53 |
|
2020 |
$13 |
$33 |
$10 |
$29 |
$60 |
|
2021 |
$13 |
$33 |
$10 |
$29 |
$60 |
|
2022 |
$14 |
$38 |
$12 |
$34 |
$68 |
|
2023 |
$14 |
$38 |
$12 |
$34 |
$68 |
|
2024 |
$16 |
$43 |
$13 |
$38 |
$76 |
|
2025 |
$16 |
$43 |
$13 |
$38 |
$76 |
|
2026 |
$16 |
$48 |
$14 |
$44 |
$85 |
|
2027 |
$16 |
$48 |
$14 |
$44 |
$85 |
Source: 10 U.S.C. §1074g(a)(6)(A)
Notes: Retail pharmacy copayments are applicable when using a network pharmacy. Additional cost sharing is applied when using a non-network pharmacy.
9. What is the Extended Care Health Option (ECHO) Program?
The Extended Care Health Option (ECHO) program provides supplemental health care and non-medical services and supplies for military families with special needs.66 ECHO pays for services and supplies designed to reduce the disabling effects of a qualifying condition and would generally not be covered under a TRICARE health plan. Qualifying conditions include:
- Autism Spectrum Disorder;
- Moderate or severe intellectual disability;
- Serious physical disability;67
; - Extraordinary physical or psychological conditions causing the beneficiary to be homebound;
- Diagnosis in an infant or toddler (under age 3) of a neuromuscular developmental condition or other condition expected to precede a diagnosis of moderate or severe mental retardation or serious physical disability; and
- Multiple disabilities, which may qualify if there are two or more disabilities impacting separate body systems.
There are three distinct categories of ECHO benefits: general services and supplies, ECHO Home Health Care (EHHC), and applied behavioral analysis for autism spectrum disorder. In general, beneficiaries are required to access federal, state and local services, such as Medicaid's Home and Community-Based Services, prior to utilizing ECHO.
|
Assistive interpreter or translation services |
Rehabilitative services |
Transportation to/from institutions or facilities |
|
Durable equipment, including adaptation and maintenance equipment |
Short-term relief for primary care givers (respite care) |
Institutional care |
|
Applied Behavioral Analysis |
Training for special education and assistive technology devices |
Expanded in-home respite care, such as home health care, physical/occupational/speech therapy, or medical case management (EHHC) |
Source: Defense Health Agency, TRICARE Fact Sheet, Extended Care Health Option, March 2018.
Dependents of active duty service membersservicemembers are the only category of DOD beneficiaries eligible for ECHO. Neither reservists and their dependents nor retirees and their dependents are eligible. To participate in ECHO, the dependent must be enrolled in a TRICARE health plan (e.g., Prime, Select, or the Uniformed Services Family Health Plan), enrolled in their service's Exceptional Family Member Program69, and have a qualifying physical or mental disability/condition. Eligible dependents register for ECHO through their respective TRICARE contractor's case management program.
There are no costs to register in ECHO. For months in which beneficiaries use the ECHO benefit, cost shares are required. Monthly cost shares are based on the sponsor's pay grade and the benefit is capped at $36,000 per beneficiary, per fiscal year. Annual service and supply costs exceeding this amount are the responsibility of the beneficiary. Respite care provided under EHHC does not count towards the general benefit cap, however it is limited to what TRICARE would pay if a dependent resided in a skilled nursing facility.
|
Sponsor Pay Grade |
Monthly Cost Share |
|
E-1 to E-5 |
$25 |
|
E-6 |
$30 |
|
E-7, O-1 |
$35 |
|
E-8, O-2 |
$40 |
|
E-9, W-1, W-2, O-3 |
$45 |
|
W-3, W-4, O-4 |
$50 |
|
W-5, O-5 |
$65 |
|
O-6 |
$75 |
|
O-7 |
$100 |
|
O-8 |
$150 |
|
O-9 |
$200 |
|
O-10 |
$250 |
Source: 32 C.F.R. §199.5.
Notes: Adapted by CRS.
10. How Are Priorities for Care in Military Treatment Facilities Assigned?
Title 10 of the U.S. Code assigns general priorities for MTF care. "A member of the uniformed services on active duty" is the only TRICARE beneficiary group entitled to care in any MTF. 70 Dependents of active duty personnel are also entitled to receive MTF care on a space-available basis.71 Military retirees and their dependents do not have an entitlement or right to MTF care, although they may receive care on a space-available basis (see question "15. Have Military Personnel Been Promised Free Medical Care for Life?").72
DOD issued regulations and implementation policy to clarify the basic priorities for MTF care:
Priority 1: Active-duty service membersservicemembers;
Priority 2: Active-duty family members enrolled in TRICARE Prime;
Priority 3: Retirees, their family members and survivors enrolled in TRICARE Prime;
Priority 4: Active-duty family members not enrolled in TRICARE Prime and TRICARE Reserve Select enrollees; and
Priority 5: All other eligible persons.73
MTF commanders are also authorized to grant certain exceptions to these priority groups. These may include care required by law or DOD policy (e.g., employees exposed to health hazards, occupational health, workplace injuries, medical emergencies), patients needed to support the clinical case mix of a Graduate Medical Education program, overseas or remote geographic location, or other extraordinary cases.
11. What are DOD's Access to Care Standards?
In 1995, DOD established access to care standards to ensure beneficiaries enrolled in TRICARE Prime receive timely care in an MTF or from a civilian health care provider. The current access to care standards, outlined in DOD regulation and implementation policy, include:
- Urgent/Acute Care: Beneficiary must be offered an appointment to visit an appropriate health care provider within 24 hours and within a 30-minute drive-time from the beneficiary's residence;
- Routine Care: Beneficiary must be offered an appointment to visit an appropriate health care provider within one week and within a 30-minute drive-time from the beneficiary's residence;
- Well-Patient Visit/Preventative Care: Beneficiary must be offered an appointment to visit an appropriate health care provider within four weeks
- Specialty Care: Beneficiary must be offered an appointment to visit an appropriate health care provider within four weeks and within a 1-hour drive-time from the beneficiary's residence;
- Office Wait Times: In non-emergency circumstances, office waiting times shall not exceed 30 minutes; and
- Access to Primary Care Manager: Beneficiary must have access to their primary care manager or designee by telephone, 24 hours a day, 7 days a week.74
12. How Does the Patient Protection and Affordable Care Act Affect TRICARE?
In general, the Patient Protection and Affordable Care Act (ACA)75 does not directly affect TRICARE administration, health care benefits, eligibility, or cost to beneficiaries.76
Section 3110 of the ACA did open a special Medicare Part B enrollment window to enable certain individuals to gain eligibility for TFL.77 The ACA also waived the Medicare Part B late enrollment penalty during the 12-month special enrollment period (SEP) for military retirees, their spouses (including widows/widowers), and dependent children who are otherwise eligible for TRICARE and are entitled to Medicare Part A based on disability or end-stage renal disease, but had previously declined Part B. The ACA required the SECDEF to identify and notify individuals of their eligibility for the SEP. Section 3110 of the ACA was amended by the Medicare and Medicaid Extenders Act of 201078 to clarify that sectionSection 3110 applies to Medicare Part B elections made on or after the date of enactment of the ACA, which was on March 23, 2010.
13. How does TRICARE Determine its Reimbursement Rates?
In general, DOD utilizes reimbursement methods similar to those of Medicare for inpatient care, outpatient care, and other related services. 10 U.S.C. §1079(h) and (j) require that payment levels for health care services provided under TRICARE be aligned with Medicare's fee schedule "to the extent practicable." DOD has the authority to grant exceptions to deviate from Medicare's fee schedule when "adequate access to care would be impaired."79
Reimbursement for Inpatient Care
The CHAMPUS Diagnosis Related Groups (DRG)-based payment system is used to reimburse civilian hospitals and other health care facilities for providing inpatient care to TRICARE beneficiaries. To ensure standardization with U.S.-based medical coding and reimbursement classifications, DOD adopted the same DRG coding scheme and nomenclature as Medicare.80 Reimbursement rates assigned to each DRG are determined by DOD and updated annually. In general, rates are calculated in a similar manner as those published by the Centers for Medicare and Medicaid Services (CMS).81
Reimbursement for Hospital-based Outpatient Care
Hospital-based outpatient services are reimbursed using the TRICARE outpatient prospective payment system (OPPS). Modeled after Medicare's OPPS program, TRICARE pays for hospital-based outpatient services on a rate-per-service basis.82 Each service is assigned a Health Care Procedure Coding System (HCPCS) code and descriptor, then categorized into an Ambulatory Payment Classification (APC) group based on clinical and cost similarities. A reimbursement rate is assigned to each group, which applies to any service in the APC. DOD publishes quarterly updates for TRICARE APC reimbursement rates, which are consistent with those published by the CMS.83
Reimbursement for Outpatient Care and Health Care-related Services
Other outpatient care and services provided in a non-hospital setting are reimbursed using the allowable charge method.84 By law (P.L. 102-396) and federal regulation (32 C.F.R. §199.14), civilian health care providers treating TRICARE patients cannot bill more than 115% of charges authorized by the DOD fee schedule, also known as the CHAMPUS Maximum Allowable Charge (CMAC). CMAC rates are updated annually, calculated on a national basis, and then adjusted for locality differences.85
TRICARE reimburses health care providers at the CMAC rate or the billed charge, whichever is lower. In some instances, TRICARE may reimburse above the CMAC rate in localities where excessive balance billing86 occurs or to ensure "adequate beneficiary access to care."87
14. What Health Benefits are Available to Reservists?
In recent years, especially as members of the Reserve Component88 have had a larger role in combat operations overseas, Congress has enlarged the health benefits available for members of the Reserve Component. Typically, DOD health benefits for members of the Reserve Component vary based on their duty status, which are outlined in Table 7.
Members of the National Guard, who are activated by their governor for state active duty (e.g., disaster response duty), may also be eligible for their state's employee health insurance program.
|
Duty Status of Reserve Component Member |
DOD Health Benefit |
Statutory Reference |
|
Serving on active duty ≥30 consecutive days |
Same health benefits as regular active component members (i.e., TRICARE Prime) |
10 U.S.C. §1074 |
|
TRICARE Prime coverage up to 180 days prior to activation if orders are in support of a contingency operation |
10 U.S.C. §1074 |
|
|
Selected Reservist in an inactive duty training status (i.e., "drilling reservist") |
Eligible to enroll in TRICARE Reserve Select, a premium-based, preferred provider organization- structured health plan |
10 U.S.C. §1076d |
|
Eligible to enroll in the premium-based TRICARE Dental Plan |
||
|
Illness or injury during inactive duty training, including travel to/from drill site |
Illness or injury-specific care at an MTF or TRICARE-authorized provider |
10 U.S.C. §1074a |
|
Separating from a period of >30 consecutive days of active duty while supporting a contingency operation |
Transitional Assistance Management Program – 180 days of eligibility for premium-free TRICARE Prime or TRICARE Select, beginning on the day of separation from active duty |
10 U.S.C. §1145 |
|
Retired Reservist (not yet eligible to receive retirement pay) |
Eligible to enroll in TRICARE Retired Reserve, a premium-based, preferred provider organization- structured health plan |
10 U.S.C. §1086 |
|
Eligible to enroll a dental plan offered by the Federal Employee Dental and Vision Program (FEDVIP) |
10 U.S.C. §1076c |
|
|
Retired Reservist (eligible to receive retirement pay, but not yet eligible for Medicare) |
Same health benefits as retirees of the active component who are not yet eligible for Medicare (e.g., TRICARE Prime or TRICARE Select) |
10 U.S.C. §1097 |
|
Eligible to enroll a dental plan offered by the Federal Employee Dental and Vision Program (FEDVIP) |
10 U.S.C. §1076c |
|
|
Retired Reservist (eligible to receive retirement pay and Medicare) |
TRICARE for Life |
10 U.S.C. §1086 |
15. Have Military Personnel Been Promised Free Medical Care for Life?
Some military personnel and retirees maintain that they and their dependents were promised "free medical care for life" at the time of their enlistment. Such promises may have been made by military recruiters and in recruiting brochures; however, if they were made, they were not based upon laws or official regulations.89 In 1993, the Deputy Assistant Secretary of Defense for Health Affairs acknowledged this notion in a statement to the House Committee on Armed Services and attempted to clarify that an entitlement to free medical care for life does not exist:
We have a medical care program for the life of our beneficiaries, and it is pretty well defined in the law. That easily gets interpreted to, or reinterpreted into, free medical care for the rest of your life. That is a pretty easy transition for people to make in their thinking, and it is pervasive. We spend an incredible amount of effort trying to reeducate people that that is not their benefit.90
Federal courts have held that current statutes or regulations do not grant a right or promise for free medical care for retirees and their dependents.91 In Sebastian v. U.S., the U.S. Court of Appeals for the Eleventh Circuit ruled that:
Nothing in these regulations provided for unconditional lifetime free medical care or authorized recruiters to promise such care as an inducement to joining or continuing in the armed forces. While the Retirees argue that the above mentioned section 4132.1 gave those of them who served as officers in the Navy and Marine Corps the right to free unconditional medical care, we cannot agree. The [1922 Manual of the Medical Department of the United States Navy] Manual provided guidelines for the Navy's Medical Department, but did not create any right in such officers to the free unconditional lifetime medical care they claim. It related only to hospital care, not the broader services that these Retirees seek, and covered only the period when it was in effect. In any event, in view of the general pattern of the military regulations that provides medical care to retirees only when facilities and personnel were available, we decline to read into the creation of such an enduring and broad right to unconditional free lifetime medical care.
In sum, we conclude that the Retirees have not shown that they have a right to the health care they say was "taken" by the government. Since the basic premise of their claim fails, their taking claim necessarily also fails.92
In 2002, an appeal of Schism v. U.S. also held that a legal, contractual right to free health care for life does not exist:
The promise of such health care was made in good faith and relied upon. Again, however, because no authority existed to make such promises in the first place, and because Congress has never ratified or acquiesced to this promise, we have no alternative but to uphold the judgement against the retirees' breach-of-contract claim.93
16. What is the Congressionally Directed Medical Research Program?
The Congressionally Directed Medical Research Program (CDMRP) is a congressional appropriation to the DOD, explicitly for peer-reviewed biomedical research in congressionally specified health matters. In general, Congress inserts CDMRP funding in the Defense Health Program's Research, Development, Test, and Evaluation (RDT&E) account in the annual DOD appropriation. CDMRP funding is not part of the President's budget request for overall RDT&E. In FY2019, 67% ($1.47 billion) of the Defense Health Program's RDT&E appropriation was for the CDMRP.94 Biomedical research conducted by the Defense Advanced Research Projects Agency or other military research agencies are funded through separate accounts and are not reflected in the CDMRP. Table 8 depicts appropriations for selected CDMRP programs in the past five years.
The U.S. Army Medical Research and Material Command (USAMRMC) administers the CDMRP and is responsible for awarding and managing competitive grants. USAMRMC solicits CDMRP grant opportunities through Program Announcements or Broad Agency Announcements, which are posted on their website or through http://www.grants.gov.
Members of Congress may request funding for medical research during the annual defense appropriations process. The appropriations committees typically send Members a memorandum with instructions for submitting requests.
Table 8. Appropriation Levels for Selected CDMRP Research Areas, FY2014-FY2019
(in millions of dollars)
|
FY2015a |
FY2016b |
FY2017c |
FY2018d |
FY2019e |
|
|
Alcohol and Substance Abuse Disorders |
4 |
4 |
4 |
4 |
4 |
|
Alzheimer's Disease |
12 |
15 |
15 |
15 |
15 |
|
Amyotrophic Lateral Sclerosis |
7.5 |
7.5 |
7.5 |
10 |
10 |
|
Autism |
6 |
7.5 |
7.5 |
7.5 |
7.5 |
|
Bone Marrow Failure |
3.2 |
3 |
3 |
3 |
3 |
|
Breast Cancer |
120 |
120 |
120 |
130 |
130 |
|
Chronic Pain Management |
- |
- |
- |
- |
10 |
|
Combat Readiness |
- |
- |
- |
- |
15 |
|
Duchenne Muscular Dystrophy |
3.2 |
3.2 |
3.2 |
3.2 |
3.2 |
|
Epilepsy |
7.5 |
7.5 |
7.5 |
7.5 |
7.5 |
|
Global HIV/AIDS |
8 |
8 |
8 |
8 |
8 |
|
Gulf War Illness |
20 |
20 |
20 |
21 |
21 |
|
Hearing Restoration |
- |
- |
10 |
10 |
10 |
|
HIV/AIDS |
12.9 |
12.9 |
12.9 |
12.9 |
12.9 |
|
Joint Warfighter Medical |
50 |
50 |
50 |
50 |
50 |
|
Kidney Cancer |
- |
- |
10 |
15 |
15 |
|
Lung Cancer |
10.5 |
12 |
12 |
14 |
14 |
|
Lupus |
- |
- |
5 |
5 |
5 |
|
Melanoma |
- |
- |
- |
- |
10 |
|
Multiple Sclerosis |
5 |
6 |
6 |
6 |
6 |
|
Orthotics and Prosthetics Outcomes |
10 |
10 |
10 |
10 |
10 |
|
Ovarian Cancer |
20 |
20 |
20 |
20 |
20 |
|
Peer-Reviewed Cancer |
50 |
50 |
60 |
80 |
80 |
|
Peer-Reviewed Medical |
247.5 |
278.7 |
300 |
330 |
330 |
|
Peer-Reviewed Orthopedic |
30 |
30 |
30 |
30 |
30 |
|
Prostate Cancer |
80 |
80 |
90 |
100 |
100 |
|
Psychological Health/Traumatic Brain Injury |
125 |
125 |
125 |
125 |
125 |
|
Reconstructive Transplant |
15 |
12 |
12 |
12 |
12 |
|
Spinal Cord Injury |
30 |
30 |
30 |
30 |
30 |
|
Therapeutic Service Dog Training |
3 |
- |
- |
- |
- |
|
Tick-Borne Disease |
- |
5 |
5 |
5 |
5 |
|
Trauma Clinical |
- |
10 |
10 |
10 |
10 |
|
Tuberous Sclerosis |
6 |
6 |
6 |
6 |
6 |
|
Vision |
10 |
10 |
15 |
15 |
15 |
|
Core Program Funding |
179.8 |
207.5 |
264.6 |
291 |
291 |
Sources:
a. Funds appropriated by P.L. 113-235. See Congressional Record, December 11, 2014, p. H9604.
b. Funds appropriated by P.L. 114-113. See House Committee on Appropriations Explanatory Statement, Division C, p. 87B.
c. Funds appropriated by P.L. 115-31. See House Committee on Appropriations Explanatory Statement, Division C, p. 76B.
d. Funds appropriated by P.L. 115-91. See House Committee on Appropriations Explanatory Statement, Division C, p. 94B.
e. Funds appropriated by P.L. 115-245. See House Committee on Appropriations Explanatory Statement, Division C, p. 96C.
Notes: The CDMRP website (http://cdmrp.army.mil/) also provides specific descriptions and funding histories of the different research programs. The "Peer-Reviewed Medical" and "Peer-Reviewed Cancer" research categories typically include multiple research areas that are eligible for funding. Eligible research areas are outlined in the explanatory statement accompanying the Defense Appropriations bill for that year.
17. Does TRICARE Cover Abortion?
10 U.S.C. §1093 provides that "Funds available to the Department of Defense may not be used to perform abortions except where the life of the mother would be endangered if the fetus were carried to term or in a case in which the pregnancy is the result of an act of rape or incest."95
18. Does DOD Use Animals in Medical Research or Training?
Yes. DOD policy is that live animals will not be used for training and education except where, after exhaustive analysis, no alternatives are available.96 Currently approved uses include pre-deployment training for medical personnel and include infant intubation (ferrets), microsurgery (rodents), and combat trauma training (goats and swine).
Appendix. Glossary of Acronyms
Glossary of Acronyms
|
ACA |
Affordable Care Act |
MBOG |
Medical Business Operations Group |
|
ADFM |
Active Duty Family Member |
MDAG |
Medical Deputies Action Group |
|
ADSM |
Active Duty Service Member |
MEDCOM |
Army Medical Command |
|
AFMS |
Air Force Medical Service |
MERHCF |
Medicare-Eligible Retiree Health Care Fund |
|
APC |
Ambulatory Payment Classification |
MHS |
Military Health System |
|
ASD(HA) |
Assistant Secretary of Defense (Health Affairs) |
MHSER |
Military Health System Executive Review |
|
BAP |
Beneficiary Advisory Panel |
MILCON |
Military Construction |
|
BUMED |
Navy Bureau of Medicine and Surgery |
MILPERS |
Military Personnel |
|
CBO |
Congressional Budget Office |
MOG |
Medical Operations Group |
|
CDMRP |
Congressionally Directed Medical Research Program |
MPOG |
Manpower and Personnel Operations Group |
|
CHAMPUS |
Civilian Health and Medical Program of the Uniformed Services |
MTF |
Military Treatment Facility |
|
CMAC |
CHAMPUS Maximum Allowable Charge |
NDAA |
National Defense Authorization Act |
|
CRS |
Congressional Research Service |
O&M |
Operations & Maintenance |
|
CSA |
Combat Support Agency |
OPPS |
Outpatient Prospective Payment System |
|
DEERS |
Defense Enrollment Eligibility Reporting System |
PAC |
Policy Advisory Council |
|
DEPSECDEF |
Deputy Secretary of Defense |
PDASD(HA) |
Principal Deputy Assistant Secretary of Defense (Health Affairs) |
|
DHA |
Defense Health Agency |
QLE |
Qualifying Life Event |
|
DHP |
Defense Health Program |
RDT&E |
Research, Development, Testing, and Evaluation |
|
DOD |
Department of Defense |
SECDEF |
Secretary of Defense |
|
DSCP |
Defense Supply Center Philadelphia |
SEP |
Special Enrollment Period |
|
ECHO |
Extended Care Health Option |
SMMAC |
Senior Military Medical Action Council |
|
EFMP |
Exceptional Family Member Program |
TAMP |
Transitional Assistance Management Program |
|
EHHC |
ECHO Home Health Care |
TFL |
TRICARE for Life |
|
eMSM |
Enhanced Multi-Service Market |
TRR |
TRICARE Retired Reserve |
|
ESI |
Express Scripts, Inc. |
TRS |
TRICARE Reserve Select |
|
FEHBP |
Federal Employee Health Benefits Program |
TYA |
TRICARE Young Adult |
|
FY |
Fiscal Year |
USAMRMC |
United States Army Medical Research and Materiel Command |
|
GAO |
Government Accountability Office |
USD(P&R) |
Under Secretary of Defense (Personnel and Readiness) |
|
HCBS |
Home and Community-Based Services |
USFHP |
Uniformed Services Family Health Plan |
|
HCPCS |
Healthcare Common Procedure Coding System |
VA |
Department of Veterans Affairs |
Author Contact Information
Acknowledgments
This product was originally prepared by [author name scrubbed], former CRS Specialist in Defense Health Care Policy.
Footnotes
| 1. |
David J. Smith, Raquel C. Bono, and Bryce J. Slinger, "Transforming the Military Health System," Journal of the American Medical Association, vol. 318, no. 24 (2017), pp. 2427-2428. |
| 2. |
For more information about the Military Health System's mission and strategic initiatives, see https://health.mil/About-MHS. |
| 3. |
10 U.S.C. §1071. |
| 4. |
10 U.S.C. §1073d. |
| 5. |
10 U.S.C. §2358. |
| 6. |
10 U.S.C. §401. Humanitarian and civic assistance activities includes medical, surgical, dental, and veterinary care, among others. |
| 7. |
Department of Defense, Evaluation of the TRICARE Program: Fiscal Year 2018 Report to Congress, April 5, 2018, p. 17, https://www.health.mil/Reference-Center/Reports/2018/05/09/Evaluation-of-the-TRICARE-Program-Fiscal-Year-2018-Report-to-Congress. |
| 8. |
The "TRI" in "TRICARE" originally referred to its initial three main benefit plan options: a health maintenance organization option (TRICARE Prime), a preferred provider option (formerly known as "TRICARE Extra"), and a fee-for-service option (formerly known as "TRICARE Standard"). |
| 9. |
Department of Defense, Plan for Reform of the Administration of the Military Health System, October 25, 2013, p. 3, https://health.mil/Reference-Center/Reports/2013/11/25/Plan-for-Reform-of-the-Administration-of-the-Military-Health-System. |
| 10. |
ibid. |
| 11. |
ibid. |
| 12. |
ibid, p. 4. |
| 13. |
ibid, p. 4. |
| 14. |
ibid, p. 4. The Human Resources and Manpower Workgroup (HR&MANPOWER WG) was the name identified in the planning process, however DOD chartered the group as the Manpower and Personnel Operations Group (MPOG). |
| 15. |
eMSM Market Managers are authorized to manage the respective market's budget, standardize clinical and business functions, support medical readiness activities, and direct the movement of manpower and workload between MTFs within the market. For more information about eMSM management, see Department of Defense, Deputy Secretary of Defense Memorandum, Implementation of Military Health System Governance Reform, March 11, 2013, p. 3, https://www.health.mil/Reference-Center/Policies/2013/03/11/Implementation-of-Military-Health-System-Governance-Reform. |
| 16. |
ibid, p. 4. |
| 17. |
ibid, p. 4. |
| 18. |
A Combat Support Agency (CSA) is defined in DOD Directive 3000.06 as an organization, designated by 10 U.S.C. §193 or the Secretary of Defense, to "provide and plan for the optimum support capabilities attainable within existing and programmed resources to the operational commanders within the parameters of the CSA's statutory responsibility and its chartering DOD Directive." |
| 19. |
MTFs in the National Capital Region include Walter Reed National Military Medical Center, Fort Belvoir Community Hospital, DiLorenzo TRICARE Health Clinic, Tri-Service Dental Clinic, Family Health Center Fairfax, and Family Health Center Dumfries. |
| 20. |
Department of Defense, DOD Directive 5136.13, Defense Health Agency, September 30, 2013. |
| 21. |
Department of Defense, Deputy Secretary of Defense Memorandum, Implementing Congressional Direction for Reform of the Military Health System, September 28, 2018, https://health.mil/Reference-Center/Policies/2018/09/28/Implementing-Congressional-Direction-for-Reform-of-the-Military-Health-System. |
| 22. |
P.L. 115-232 §711. |
| 23. |
Service Surgeons General are typically general or flag officers in the grade of Lieutenant General/Vice Admiral. |
| 24. |
Statutory duties assigned to the Service Surgeons General are described in 10 U.S.C. §§3036, 5136, 8036. |
| 25. |
Additional duties assigned to the Service Surgeons General were included in |
| 26. |
See question "3. What is the Medicare-Eligible Retiree Health Care Fund (MERHCF)?" for a discussion of the MERHCF. |
| 27. |
Third-party collections are funds collected from additional health insurance payers for beneficiary care delivered by an MTF. |
| 28. |
Department of Defense, FY 2019 Budget Request Overview, February 2018, |
| 29. |
P.L. 106-398 §712. |
| 30. |
Federal agencies that contribute to the MERHCF are DOD (Air Force, Army, Marine Corps, Navy), Department of Health and Human Services (Public Health Service), Department of Homeland Security (Coast Guard), and Department of Commerce (National Oceanic and Atmospheric Administration). |
| 31. |
Department of Defense, Valuation of the Medicare-Eligible Retiree Health Care Fund, December 2017, p. 4, https://media.defense.gov/2018/Apr/12/2001902556/-1/-1/0/MERHCF%20VAL%20RPT%202016.PDF. |
| 32. |
P.L. 103-337 §738. |
| 33. |
Department of Defense, Request for Proposals – Section C: Description/Specifications/Work Statement (HT9402-15-R-0002), November 3, 2014, https://www.fbo.gov/notices/157d8d11c7087ac0a3bb5f2fe10a7b83. |
| 34. |
U.S. Government Accountability Office, GAO Decision in the Matter of UnitedHealth Military & Veteran Services LLC; WellPoint Military Care Corporation; Health Net Federal Services, LLC, B-411837.2, November 9, 2016, https://www.gao.gov/assets/690/681207.pdf. |
| 35. |
Dependents of active duty |
| 36. |
The catastrophic cap is an annual maximum limit that a beneficiary pays out of pocket for TRICARE cost sharing. In general, point of service charges, TRS, TRR, and TYA premiums, non-TRICARE covered benefits, and balance billing charges do not apply to the catastrophic cap. |
| 37. |
32 C.F.R. § |
| 38. |
10 U.S.C. §1076d. |
| 39. |
For more on the Ready Reserve and Selected Reserve see CRS Report RL30802, Reserve Component Personnel Issues: Questions and Answers, by [author name scrubbed] and [author name scrubbed], Question 2. |
| 40. |
The Transitional Assistance Management Program (TAMP) provides an additional 180 days of premium-free coverage for TRICARE Prime or TRICARE Select. Beneficiaries are eligible for TAMP if their sponsor is subject to certain transitional events, such as involuntary separation under honorable conditions, demobilizing member of the Reserve Component, sole survivorship discharge, or transition from the Active Component to the Reserve Component. For more information about TAMP, see https://tricare.mil/tamp. |
| 41. |
10 U.S.C. §1076d specifies that members of the Selected Reserves who are "eligible to enroll in a health benefits plan under chapter 89 of title 5" are not eligible to enroll in TRICARE Reserve Select. |
| 42. |
Department of Defense, Assistant Secretary of Defense (Health Affairs) Memorandum, Policy Memorandum to Establish |
| 43. |
10 U.S.C. §1076e. |
| 44. |
For more on military retirement, see CRS Report RL34751, Military Retirement: Background and Recent Developments, by [author name scrubbed]. |
| 45. |
Department of Defense, Assistant Secretary of Defense (Health Affairs) Memorandum, Policy Memorandum to Establish |
| 46. |
10 U.S.C. §1110b. |
| 47. |
P.L. 111-383 §702. |
| 48. |
Department of Defense, Assistant Secretary of Defense (Health Affairs) Memorandum, |
| 49. |
Medicare Part B is covers medically necessary outpatient services and equipment (e.g., physicians' and non-physician services, outpatient hospital services, durable medical equipment, clinical laboratory tests, ambulance services, and limited prescription drugs and biologics). Participation in Medicare Part B is voluntary, however enrollment and monthly premiums are required for those who opt-in. For more information on Medicare Part B, see CRS Report R40425, Medicare Primer, coordinated by [author name scrubbed]. |
| 50. |
10 U.S.C. §1086(d). |
| 51. |
CRS Report R40082, Medicare: Part B Premiums, by [author name scrubbed]. |
| 52. |
Department of Defense, "TRICARE Open Season Begins November 12," press release, August 1, 2018, https://www.health.mil/News/Articles/2018/08/01/TRICARE-Open-Season-Begins-November-12. |
| 53. |
10 U.S.C. §1074g. |
| 54. |
Express Scripts, Inc., "Express Scripts Awarded TRICARE Pharmacy Program Contract," press release, June 27, 2008, https://globenewswire.com/news-release/2008/06/27/380555/145445/en/Express-Scripts-Awarded-TRICARE-Pharmacy-Program-Contract.html. |
| 55. |
10 U.S.C. §1074g(a)(2)(A). |
| 56. |
10 U.S.C. §1074g(b). The Pharmacy and Therapeutics Committee meets at least quarterly and its minutes are publicly available at the Defense Health Agency Pharmacy Operations Division website: https://health.mil/About-MHS/OASDHA/Defense-Health-Agency/Operations/Pharmacy-Division/DoD-Pharmacy-and-Therapeutics-Committee . |
| 57. |
The Beneficiary Advisory Panel (BAP) is a federal advisory committee established by 10 U.S.C. §1074g(c). For more information on the BAP, see https://health.mil/bap. |
| 58. |
DHA provides a publicly-available list of MTF pharmacies that accept electronic prescriptions from civilian providers. See https://www.health.mil/Military-Health-Topics/Access-Cost-Quality-and-Safety/Access-to-Healthcare/Pharmacy-Program/Electronic-Prescribing. |
| 59. |
Office of the Assistant Secretary of Defense (Health Affairs), Memorandum subject "TRICARE Pharmacy Benefit Program Formulary Management" dated December 22, 2004. Accessed August 7, 2018, at https://www.health.mil/Reference-Center/Policies/2005/12/19/Clarification-to-HA-Policy-04-032--TRICARE-Pharmacy-Benefit-Program-Formulary-Management--December-2. |
| 60. |
The VA has authority delegated from the General Services Administration to manage the medical care sections of the Federal Supply Schedule, which includes pharmaceuticals. For more information on the delegation of authority authorized in Federal Acquisition Regulation Subpart 8.402(a), see https://www.acquisition.gov/far/current/html/Subpart%208_4.html. |
| 61. |
ESI was awarded the TRICARE pharmacy benefit manager contract, which includes a base year, seven one-year option periods, and options for a phase-out period. The estimated value of the contract is $5.3 billion. For more information, see https://www.fbo.gov/notices/7701a811be0214a23f04b4e284f8b13b. |
| 62. |
32 C.F.R. §199.21(j). |
| 63. |
Department of Defense, "Evaluation of the TRICARE Program: Fiscal Year 2017 Report to Congress," April 5, 2018, p. 35, https://www.health.mil/Reference-Center/Reports/2018/05/09/Evaluation-of-the-TRICARE-Program-Fiscal-Year-2018-Report-to-Congress. |
| 64. |
ibid. |
| 65. |
10 U.S.C. §1074g(a). |
| 66. |
For additional information please see the ECHO web page at http://www.tricare.mil/echo. |
| 67. |
"Serious physical disability" is defined in 32 C.F.R. §199.2 as a "physiological disorder or condition or anatomical loss affecting one or more body systems which has lasted, or with reasonable certainty is expected to last, for a minimum period of 12 contiguous months, and which precludes the person with the disorder, condition or anatomical loss from unaided performance of at least one major life activity as defined in this section." |
| 68. |
Qualifying conditions are outlined in 32 C.F.R. §199.5(b)(2). |
| 69. |
EFMP is a program for active duty family members with special medical or education needs. The program coordinates support services from the MHS and DOD education systems. Each military service mandates enrollment in EFMP if a family member has special needs. Additional information on EFMP can be found at https://www.militaryonesource.mil/-/the-exceptional-family-member-program-for-families-with-special-needs. |
| 70. |
10 U.S.C. §1074. |
| 71. |
10 U.S.C. §1076. |
| 72. |
10 U.S.C. §1074. |
| 73. |
DOD clarified the basic priorities for MTF care in 32 C.F.R. §199.17(d) and Department of Defense, Health Affairs Policy 11-005, TRICARE Policy for Access to Care, February 23, 2011. |
| 74. |
DOD access to care standards are elaborated in Department of Defense, Health Affairs Policy 11-005, TRICARE Policy for Access to Care, February 23, 2011. There are stipulated in 32 C.F.R. §199.17(p)(5). |
| 75. | |
| 76. |
CRS Report R41198, TRICARE and VA Health Care: Impact of the Patient Protection and Affordable Care Act (ACA), by [author name scrubbed] and [author name scrubbed]. |
| 77. |
P.L. 111-148 §3110. |
| 78. |
P.L. 111-309 §201. |
| 79. |
32 C.F.R. §199.14(j)(iv)(C). |
| 80. |
Diagnosis Related Groups (DRGs) is a method of assigning a predetermined cost of inpatient care for a specific diagnosis. Costs assigned to each DRG are determined prospectively by the U.S. Centers for Medicare and Medicaid Services (CMS), and accounts for severity of illness, prognosis, treatment difficulty, need for intervention, and resource intensity. Additional cost adjustments may be made for geographic or other factors impacting wage differences. The DRG-based payment system is required by 42 U.S.C. §1395ww for all civilian health care facilities that participate in Medicare. For more information about DRGs, see https://www.cms.gov/ICD10Manual/version34-fullcode-cms/fullcode_cms/Design_and_development_of_the_Diagnosis_Related_Group_(DRGs)_PBL-038.pdf. |
| 81. |
TRICARE DRG rates are available at https://health.mil/Military-Health-Topics/Business-Support/Rates-and-Reimbursement/Diagnosis-Related-Group-Rates. |
| 82. |
For more information on Medicare's Outpatient Prospective Payment System (OPPS), see https://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNProducts/downloads/HospitalOutpaysysfctsht.pdf. |
| 83. |
Quarterly TRICARE APC reimbursement rate updates are available at https://health.mil/Military-Health-Topics/Business-Support/Rates-and-Reimbursement/Outpatient-Prospective-Payment-System. Reimbursement rates for TRICARE-specific APCs are updated on an annual basis instead of quarterly. |
| 84. |
Outpatient care and services provided in a non-hospital setting can include laboratory services, rehabilitation therapy, radiology, durable medical equipment, certain drugs, professional provider services, facility charges, and ambulance services. |
| 85. |
Locality configurations and adjustments are made in the same manner as Medicare's Fee Schedules. For more information on Medicare's Fee for Service localities, see https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/PhysicianFeeSched/Locality.html. CMAC rates are available at https://health.mil/Military-Health-Topics/Business-Support/Rates-and-Reimbursement/CMAC-Rates. |
| 86. |
Balance billing occurs when a health care provider or facility bills a patient for the difference between what was charged and the allowed reimbursement rate. |
| 87. |
32 C.F.R. 199.14(j)(1)(iv). |
| 88. |
For additional information on Reserve Component pay and benefits, see CRS Report RL30802, Reserve Component Personnel Issues: Questions and Answers, by [author name scrubbed] and [author name scrubbed]. |
| 89. |
Under current laws and federal regulations only active duty personnel are entitled to military health care. Active duty dependents also have an entitlement to care, however, may be seen in an MTF on a space-available basis. Retirees and their dependents have no such entitlement, but may be seen in an MTF on a space-available basis. See question "10. How Are Priorities for Care in Military Treatment Facilities Assigned?". |
| 90. | |
| 91. |
See Coalition of Retired Military Veterans, et al. v. United States of America, U.S. Dist. of South Carolina, C.A.#2:96-3822-23, Dec. 10, 1997: 11-12; Sebastian v. United States, 185 F.3d 1368, 1372 (Fed. Cir. 1999); or Schism and Reinlie v. United States, 2002 WL 31549178 (Fed.Cir. (Fla.)), November 18, 2002. |
| 92. |
Sebastian v. U.S., 185 F.3d 1368 (11th Cir. 2002). |
| 93. |
Schism and Reinlie v. U.S., 239 F.3d 1280 (11th Cir. 2001). |
| 94. |
U.S. Congress, House Committee on Appropriations, Explanatory Statement to P.L. 115-245, 115th Cong., 2018. |
| 95. |
The clause "or in a case in which the pregnancy is the result of an act of rape or incest" was added by |
| 96. |
Department of Defense, Department of Defense Instruction 3216.01, Use of Animals in DoD Programs, at http://www.esd.whs.mil/Portals/54/Documents/DD/issuances/dodi/321601p.pdf?ver=2017-10-03-131649-680. |