Medicare Part B: Enrollment and Premiums
Changes from July 5, 2018 to April 4, 2019
This page shows textual changes in the document between the two versions indicated in the dates above. Textual matter removed in the later version is indicated with red strikethrough and textual matter added in the later version is indicated with blue.
Contents
- Introduction
- Medicare Part B Eligibility and Enrollment
- Initial Enrollment Periods
- General Enrollment Period
- Late-Enrollment Premium Penalty and Exemptions
- Calculation of Penalty
- Penalty Exemptions
- Current Workers
- International Volunteers
- Equitable Relief
- Collection of the Part B Premium
- Deduction of Part B Premiums from Social Security Checks
- Part B Enrollees Who Do Not Receive Social Security Benefits
- Determining the Part B Premium
- Premium Calculation for
20182019
- Contingency Margin
- Income-Related Premiums
- Determination of Income
- Income Categories and Premium Adjustments
- Income Thresholds
- Premium Assistance for Low-Income Beneficiaries
- Qualified Medicare Beneficiaries
- Specified Low-Income Medicare Beneficiaries
- Qualifying Individuals
- Protection of Social Security Benefits from Increases in Medicare Part B Premiums
- Some Beneficiaries Are Not Protected by the Hold-Harmless Provision
- Application of the Hold-Harmless Rule in Years Prior to 2016
- Application of the Hold-Harmless Rule in 2016
- Application of the Hold-Harmless Rule in 2017
- Application of the Hold-Harmless Rule in 2018
- Application of the Hold-Harmless Rule in 2019
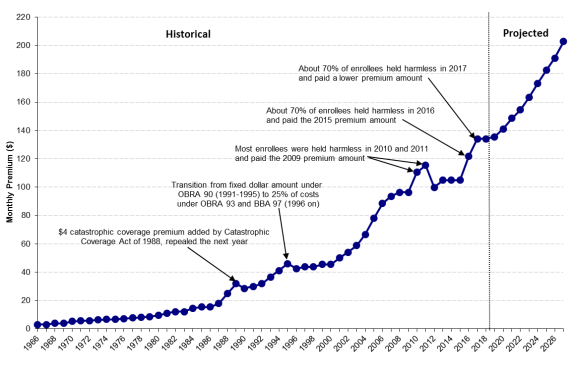
Part B Premiums over Time- Current Issues
- Premium Amount and Annual Increases
- Impact of the Hold-Harmless Provision on Those Not Held Harmless
- Proposals to Modify the Late-Enrollment Penalty
- Deficit Reduction Proposals
- Increasing Medicare Premiums
- Impose a Part B Premium Surcharge for Beneficiaries in Medigap Plans with Near First-Dollar Coverage
- Limit Federal Subsidies
- Considerations
Tables
- Table 1. Initial Enrollment Period
- Table 2. Monthly Medicare Part B Premiums for
20182019
- Table 3. Part B Premium Adjustment for Married Beneficiaries Filing Separately for
20182019
- Table 4. Medicare High-Income Premium Thresholds: 2017 to 2019
- Table 5.
20182019 Medicare Savings Program Eligibility Standards - Table A-1. Monthly Part B Premiums, 1966-
20182019
- Table B-1. Income Levels for Determining Part B Premium Adjustment and Per Person Premium Amounts, 2007-
20182019
- Table B-2. Income Levels for Determining Part B Premium Adjustment for Married Beneficiaries Filing Separately and Associated Premiums, 2007-
20182019
- Table C-1. Projected Part B Premiums
Appendixes
- Appendix A. History of the Part B Premium Statutory Policy and Legislative Authority
- Appendix B. Standard and High-Income Part B Premiums and Income Thresholds: 2007-
20182019
- Appendix C. Estimated Future Part B Premiums
- Appendix D. Bipartisan Budget Act of 2015 Changes to 2016 Part B Premiums
- Appendix E. Part A Premiums
Summary
Medicare is a federal insurance program that pays for covered health care services of most individuals aged 65 and older and certain disabled persons. In calendar year 20182019, the program is expected to cover about 6061 million persons (5152 million aged and 9 million disabled) at a total cost of $745798 billion. Most individuals (or their spouses) aged 65 and older who have worked in covered employment and paid Medicare payroll taxes for 40 quarters receive premium-free Medicare Part A (Hospital Insurance). Those entitled to Medicare Part A (regardless of whether they are eligible for premium-free Part A) have the option of enrolling in Part B, which covers such things as physician and outpatient services and medical equipment.
Beneficiaries have a seven-month initial enrollment period, and those who enroll in Part B after this initial enrollment period and/or reenroll after a termination of coverage may be subject to a late-enrollment penalty. This penalty is equal to a 10% surcharge for each 12 months of delay in enrollment and/or reenrollment. Under certain conditions, some beneficiaries are exempt from the late-enrollment penalty; these exempt beneficiaries include working individuals (and their spouses) with group coverage through their current employment, some international volunteers, and those granted "equitable relief."
Whereas Part A is financed primarily by payroll taxes paid by current workers, Part B is financed through a combination of beneficiary premiums and federal general revenues. The standard Part B premiums are set to cover 25% of projected average per capita Part B program costs for the aged, with federal general revenues accounting for the remaining amount. In general, if projected Part B costs increase or decrease, the premium rises or falls proportionately. However, some Part B enrollees are protected by a provision in the Social Security Act (the hold-harmless provision) that prevents their Medicare Part B premiums from increasing more than the annual increase in their Social Security benefit payments. This protection does not apply to four main groups of beneficiaries: low-income beneficiaries whose Part B premiums are paid by the Medicaid program; high-income beneficiaries who are subject to income-related Part B premiums; those whose Medicare premiums are not deducted from Social Security benefits; and new Medicare and Social Security enrollees.
Most Part B participants must pay monthly premiums, which do not vary with a beneficiary's age, health status, or place of residence. However, since 2007, higher-income enrollees pay higher premiums to cover a higher percentage of Part B costs. Additionally, certain low-income beneficiaries may qualify for Medicare cost-sharing and/or premium assistance from Medicaid through a Medicare Savings Program. The premiums of those receiving benefits through Social Security are deducted from their monthly payments.
Each year, the Centers for Medicare & Medicaid Services (CMS) determines the Medicare Part B premiums for the following year. The standard monthly Part B premium for 2018 is $134.00. However, due to a relatively low (2.0%) Social Security cost-of-living adjustment (COLA) in 20182019 is $135.50. However, in 2019, the hold-harmless provision applies to about 283.5% of Part B enrollees, and these individuals pay lower premiums. (The premiums of those held harmless vary depending on the dollar amount of the increase in their Social Security benefits.) Higher-income beneficiaries, currently defined as individuals with incomes over $85,000 per year or couples with incomes over $170,000 per year, pay $187.50, $267.90, $348.30, or $428.60189.60, $270.90, $352.20, $433.40, or $460.50 per month, depending on their income levels.
Starting in 2018, the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA; P.L. 114-10) reducesreduced the income thresholds in the highest two income tiers so that more enrollees will pay higher premiums. The Bipartisan Budget Act of 2018 (BBA 18; P.L. 115-123) addsadded an additional income tier beginning in 2019 for individuals with annual incomes of $500,000 or more or couples filing jointly with incomes of $750,000 or more.
Current issues related to the Part B premium that may come before Congress include the amount of the premium and its rate of increase (and the potential net impact on Social Security benefits), the impact of the hold-harmless provision on those not held harmless, modifications to the late-enrollment penalty, and possible increases in Medicare premiums as a means to reduce federal spending and deficits.
Introduction
Medicare is a federal insurance program that pays for covered health care services of most individuals aged 65 and older and certain disabled persons. Medicare serves approximately one in six Americans and virtually all of the population aged 65 and over. In calendar year (CY) 20182019, the program is expected to cover about 6061 million persons (5152 million aged and 9 million disabled) at a total cost of about $745798 billion, accounting for approximately 3.78% of gross domestic product.1 The Medicare program is administered by the Centers for Medicare & Medicaid Services (CMS) within the Department of Health and Human Services (HHS), and individuals enroll in Medicare through the Social Security Administration (SSA).
Medicare consists of four parts—Parts A through D. Part A covers hospital services, skilled nursing facility services, home health visits, and hospice services. Part B covers a broad range of medical services and supplies, including physician services, laboratory services, durable medical equipment, and outpatient hospital services. Enrollment in Part B is voluntary; however, most Medicare beneficiaries (about 91%) are enrolled in Part B. Part C (Medicare Advantage) provides private plan options, such as managed care, for beneficiaries who are enrolled in both Part A and Part B. Part D provides optional outpatient prescription drug coverage.2
Each part of Medicare is funded differently.3 Part A is financed primarily through payroll taxes imposed on current workers (2.9% of earnings, shared equally between employers and workers), which are credited to the Hospital Insurance (HI) Trust Fund. Beginning in 2013, workers with annual wages over $200,000 for single tax filers or $250,000 for joint filers pay an additional 0.9%.4 Beneficiaries generally do not pay premiums for Part A. In 20182019, total Part A expenditures are expected to reach about $311328 billion, representing about 4241% of program costs.5 Parts B and D, the voluntary portions, are funded through the Supplementary Medical Insurance (SMI) Trust Fund, which is financed primarily by general revenues (transfers from the U.S. Treasury) and premiums paid by enrollees. In 20182019, about $4.12.8 billion in fees on manufacturers and importers of brand-name prescription drugs also will be used to supplement the SMI Trust Fund.6 In 20182019, Part B expenditures are expected to reach about $340367 billion, and Part D expenditures are expected to reach about $95104 billion, representing 46% and 13% of program costs, respectively. (Part C is financed proportionately through the HI and SMI Trust Funds; expenditures for Parts A and B services provided under Part C are included in the above expenditure figures.)
Part B beneficiary premiums are normally set at a rate each year equal to 25% of average expected per capita Part B program costs for the aged for the year.7 Higher-income enrollees pay higher premiums set to cover a greater percentage of Part B costs,8 while those with low incomes may qualify for premium assistance through one of several Medicare Savings Programs administered by Medicaid.9 Individuals who receive Social Security or Railroad Retirement Board (RRB) retirement or disability benefits have their Part B premiums automatically deducted from their benefit checks. Part B premiums are generally announced in the fall prior to the year that they are in effect (e.g., the 20182019 Part B premiums were announced in November 2017October 2018).10
In 20182019, the standard monthly Part B premium is $134.00135.50.11 However, about 283.5% of Part B enrollees are protected by a provisionhold-harmless provision in the Social Security Act (the hold-harmless provision) that prevents their Medicare Part B premiums from increasing more than the annual dollar amount of the increase in their Social Security benefit payments. These individuals pay premiums of less than $134.00.12 About 72% of beneficiaries do not qualify for protection under the hold-harmless provision in 2018. This includes those who had been held harmless in 2017 but whose 2018 Social Security COLA benefit increases were large enough to cover their Medicare premium increases (42% of enrollees), along with the approximately 30% of enrollees who do not normally qualify to be held harmless, such as high-income enrollees, those who do not receive Social Security benefits, and those whose premiums are paid by Medicaid.13
|
433.40 Greater than or equal to $500,000 Greater than or equal to $750,000 460.50 |
In addition to premiums, Part B beneficiaries may pay other out-of-pocket costs when they use services. The annual deductible for Part B services is $183185.00 in 2018.142019.13 After the annual deductible is met, beneficiaries are responsible for coinsurance costs, which are generally 20% of Medicare-approved Part B expenses.
This report provides an overview of Medicare Part B premiums, including information on Part B eligibility and enrollment, late-enrollment penalties, collection of premiums, determination of annual premium amounts, premiums for high-income enrollees, premium assistance for low-income enrollees, protections for Social Security recipients from rising Part B premiums, and historical Medicare Part B premium trends. This report also provides a summary of various premium-related issues that may be of interest to Congress. Specific Medicare and Social Security publications and other resources for beneficiaries, and those who provide assistance to them, are cited where appropriate.
Medicare Part B Eligibility and Enrollment
An individual (or the spouse of an individual) who has worked in covered employment and paid Medicare payroll taxes for 40 quarters is entitled to receive premium-free Medicare Part A benefits upon reaching the age of 65. Those who have paid in for fewer than 40 quarters may enroll in Medicare Part A by paying a premium.1514 All persons entitled to Part A (regardless of whether they are eligible for premium-free Part A) are also entitled to enroll in Part B. An aged person not entitled to Part A may enroll in Part B if he or she is aged 65 or over and either a U.S. citizen or an alien lawfully admitted for permanent residence who has resided in the United States continuously for the immediately preceding five years.
Those who are receiving Social Security or RRB benefits are automatically enrolled in Medicare, and coverage begins the first day of the month they turn 65.1615 These individuals will receive a Medicare card and a "Welcome to Medicare" package about three months before their 65th birthday.1716 Those who are automatically enrolled in Medicare Part A also are automatically enrolled in Part B.1817 However, because beneficiaries must pay a premium for Part B coverage, they have the option of turning it down.1918 Disabled persons who have received cash payments for 24 months under the Social Security or RRB disability programs also automatically receive a Medicare card and are enrolled in Part B unless they specifically decline such coverage.2019 Those who choose to receive coverage through a Medicare Advantage plan (Part C) must enroll in Part B.
Persons who are not receiving Social Security or RRB benefits, for example because they are still working2120 or have chosen to defer enrollment because they have not yet reached their full retirement benefit eligibility age,2221 must file an application with the SSA or RRB for Medicare benefits.2322 There are two kinds of enrollment periods, one that occurs when individuals are initially eligible for Medicare and one annual general enrollment period for those who missed signing up during their initial enrollment period. A beneficiary may drop Part B enrollment and reenroll an unlimited number of times; however, premium penalties may be incurred.
Initial Enrollment Periods
Those who are not automatically enrolled in Medicare may sign up during a certain period when they first become eligible. The initial enrollment period is seven months long and begins three months before the month in which the individual first turns 65. (See Table 1.) Beneficiaries who do not file an application for Medicare benefits during their initial enrollment period could be subject to the Part B late-enrollment penalty. (See "Late-Enrollment Premium Penalty and Exemptions.") If an individual accepts the automatic enrollment in Medicare Part B, or enrolls in Medicare Part B during the first three months of the initial enrollment period, coverage will start with the month in which an individual is first eligible, that is, the month of the individual's 65th birthday. Those who enroll during the last four months will have their coverage start date delayed from one to three months after enrollment.2423 The initial enrollment period of those eligible for Medicare based on disability or permanent kidney failure is linked to the date the disability or treatment began.25
|
3 Months Before the Month One Turns 65 |
The Month During Which One Turns 65 |
Up to 3 Months After the Month One Turns 65 |
|
|
Effective Dates |
If one signs up during the first 3 months of one's initial enrollment period, Part B coverage starts the 1st day of one's birthday month.a |
If one enrolls during one's birthday month, the start date will be the 1st day of the next month. |
The start date will be delayed if one enrolls during the last 3 months of the initial enrollment period.
|
|
Example for Someone Turning 65 During the Month of June (The seven-month initial enrollment period would run from March 1 through September 30.) |
If one enrolls in March, April, or May, coverage begins June 1. |
If one enrolls in June, coverage begins July 1. |
|
Source: Table prepared by CRS based on Social Security Administration, "Medicare," Publication No. 05-10043, at https://www.ssa.gov/pubs/EN-05-10043.pdf.
a. If one's birthday falls on the 1st of the month, then the enrollment period starts a month earlier and coverage may begin on the 1st day of the month prior to one's birthday month.
General Enrollment Period
An individual who does not sign up for Medicare during the initial enrollment period must wait until the next general enrollment period. In addition, persons who decline Part B coverage when first eligible, or terminate Part B coverage, must also wait until the next general enrollment period to enroll or reenroll. The general enrollment period lasts for three months from January 1 to March 31 of each year, with coverage beginning on July 1 of that year. A late-enrollment penalty may apply.26
Late-Enrollment Premium Penalty and Exemptions
Beneficiaries who do not sign up for Part B when first eligible, or who drop it and then sign up again later, may have to pay a late-enrollment penalty for as long as they are enrolled in Part B.2726 Monthly premiums for Part B may go up 10% for each full 12-month period that one could have had Part B but did not sign up for it. (See "Calculation of Penalty.") Some may be exempt from paying a late-enrollment penalty if they meet certain conditions that allow them to sign up for Part B during a special enrollment period (SEP). (See "Penalty Exemptions.") In 20172018, about 1.34% of Part B enrollees (about 701760,000) paid this penalty.2827 On average, their total premiums (standard premium plus penalty) were about 3128% higher than what they would have been had they not been subject to the penalty.
Those who receive premium assistance through a Medicare Savings Program do not pay the late-enrollment penalty.2928 Additionally, for those disabled persons under the age of 65 subject to a premium penalty, once the individual reaches the age of 65, he or she qualifies for a new enrollment period and no longer pays a penalty.
The penalty provision was included in the original Medicare legislation enacted in 1965 to help prevent adverse selection by creating a strong incentive for all eligible beneficiaries to enroll in Part B.3029 Adverse selection occurs when only those persons who think they need the benefits actually enroll in the program. When this happens, per capita costs are driven up and premiums go up, causing more enrollees (presumably the healthier and less costly ones) to drop out of the program.3130 With most eligible persons over the age of 65 enrolled in Part B, the costs are spread over the majority of this population and per capita costs are less than would be the case if adverse selection had occurred.
As the Part B late-enrollment penalty is tied to Medicare eligibility and not to access to covered services, individuals who live in areas where Medicare benefits are generally not provided, such as outside of the United States or in prison, could still be subject to the Part B late-enrollment penalty if they do not sign up for (or if they drop) Part B when eligible.3231 To illustrate, if a retired Medicare-eligible individual stopped paying Part B premiums while living overseas for a three-year period and reenrolled when returning to the United States, he or she would not be entitled to ana SEP. This individual would instead need to enroll during the general enrollment period and could also be subject to late-enrollment penalties based on that three-year lapse in coverage.
Additionally, Part B does not have a "creditable" coverage exemption similar to that under the Part D outpatient prescription drug benefit.3332 Except for certain circumstances discussed below, having equivalent coverage does not entitle one to ana SEP should one decide to enroll in Part B later. For example, an individual who has retiree coverage similar to Part B and therefore decides not to enroll in Part B when first eligible could be subject to late-enrollment penalties if he or she enrolls in Part B at a later time (for example, because the retiree coverage was discontinued).
Calculation of Penalty
The late-enrollment penalty is equal to a 10% premium surcharge for each full 12 months of delay in enrollment and/or reenrollment during which the beneficiary was eligible for Medicare.3433 The period of the delay is equal to (1) the number of months that elapse between the end of the initial enrollment period and the end of the enrollment period in which the individual actually enrolls or (2) for a person who reenrolls, the months that elapse between the termination of coverage and the close of the enrollment period in which the individual enrolls.
Generally, individuals who do not enroll in Part B within a year of the end of their initial enrollment period would be subject to the premium penalty. For example, if an individual's initial enrollment period ended in September 20152016 and the individual subsequently enrolled during the 20162017 general enrollment period (January 1 through March 31), the delay would be less than 12 months and the individual would not be subject to a penalty. However, if that individual delayed enrolling until the 20182019 general enrollment period, the premium penalty would be 20% of that year's standard premium. (Although the elapsed time covers a total of 30 months of delayed enrollment, the episode includes only two full 12-month periods.) An individual who waits 10 years to enroll in Part B could pay twice the standard premium amount.
The late-enrollment surcharge is calculated as a percentage of the monthly standard premium amount (e.g., $134.00 in 2018),35135.50 in 2019),34 and that amount is added to the beneficiary's premium each month. The hold-harmless provision does not provide protection from increases in the penalty amounts. This means that although those who are held harmless in 2018 pay reduced premiums, any late-enrollment penalties are based on the 20182019 premium of $134.00135.50 per month.
Using the example above in which an individual is subject to a 20% premium penalty, the total monthly premium in 20182019 would be calculated as follows (see text box):
|
Calculation of Late-Enrollment Penalty
Example of a 20% penalty in 201
Premium Penalty = $ Penalty-Adjusted Premium = $
Premium Penalty = $ Penalty-Adjusted Premium = $ *Premium amounts are rounded to the nearest 10 cents. **Actual premiums of those held harmless in |
For those subject to the high-income premium (see "Income-Related Premiums"), the late-enrollment surcharge applies only to the standard monthly premium amount and not to the higher-income adjustment portion of their premiums. Using the example of a 20% penalty for a beneficiary with an income of between $85,000 and $107,000, the applicable income-related adjustment of $53.5054.10 would be added on to the penalty-adjusted premium of $160.80 ($134.00 + $26.80162.60 ($135.50 + $27.10 penalty), for a total monthly premium of $214.30.36
There is no upper limit on the amount of the surcharge that may apply, and the penalty continues to apply for the entire time the individual is enrolled in Part B. Each year, the surcharge is calculated using the standard premium amount for that particular year. Therefore, if premiums increase in a given year, the dollar value of the surcharge will increase as well.
Penalty Exemptions
Under certain conditions, select beneficiaries may be exempt from the late-enrollment penalty. Beneficiaries who are exempt include working individuals (and their spouses) with group coverage, some international volunteers, and those who based their nonenrollment decision on incorrect information provided by a federal representative. Individuals who are permitted to delay enrollment have their own SEPs.
Current Workers
A working individual and/or the spouse of a working individual may be able to delay enrollment in Medicare Part B without being subject to the late-enrollment penalty. Delayed enrollment is permitted when an individual aged 65 or older has group health insurance coverage based on the individual's or spouse's current employment (with an employer with 20 or more employees). About 1.9In 2018, about 2.0 million of the 3.38 million working aged population arewere enrolled in Part A only, with most of the rest enrolled in both Parts A and B.3736 Delayed enrollment is also permitted for certain disabled persons who have group health insurance coverage based on their own or a family member's current employment with a large group health plan. For the disabled, a large group health plan is defined as one that covers 100 or more employees.
Specifically, persons permitted to delay coverage without penalty are those persons whose Medicare benefits are determined under the Medicare Secondary Payer program.3837 Under Medicare Secondary Payer rules, an employer (with 20 or more employees) is required to offer workers aged 65 and over (and workers' spouses aged 65 and over) the same group health insurance coverage that is made available to other employees.3938 The worker has the option of accepting or rejecting the employer's coverage. If he or she accepts the coverage, the employer plan is primary (i.e., pays benefits first) for the worker and/or spouse aged 65 or over, and Medicare becomes the secondary payer (i.e., fills in the gaps in the employer plan, up to the limits of Medicare's coverage). Similarly, a group health plan offered by an employer with 100 or more employees is the primary payer for its employees under 65 years of age, or their dependents, who are entitled to Medicare because of disability.40
Such individuals may sign up for Medicare Part B (or Part A) anytime that they (or their spouse) are still working, and they are covered by a group health plan through the employer or union based on that work. Additionally, those who qualify for Medicare based on age may sign up during the eight-month period after employment or retirement or the ending of group health plan coverage ends, whichever happens first. (If an individual's group health plan coverage, or the employment on which it is based, ends during the initial enrollment period, that individual would not qualify for ana SEP.)4140 Disabled individuals whose group plan is involuntarily terminated have six months to enroll without penalty.4241
Individuals who fail to enroll during this special enrollment period are considered to have delayed enrollment and thus could be subject to the penalty. For example, even though an individual may have continued health coverage through the former employer after retirement or have COBRA coverage,4342 he or she must sign up for Part B within eight months of retiring to avoid paying a Part B penalty if he or she eventually enrolls. Individuals who return to work and receive health care coverage through that employment may be able to drop Part B coverage, qualify for a new special enrollment period upon leaving that employment, and reenroll in Part B without penalty as long as enrollment is completed within the specified time frame.
International Volunteers
Some international volunteers may also be exempt from the Part B late-enrollment penalty. The Deficit Reduction Act of 2005 (P.L. 109-171) permits certain individuals to delay enrollment in Part B without a late-enrollment penalty if they volunteered outside of the United States for at least 12 months through a program sponsored by a tax-exempt organization defined under Section 501(c)(3) of the Internal Revenue Code.4443 These individuals must demonstrate that they had health insurance coverage while serving in the international program. Individuals permitted to delay enrollment have a six-month SEP, which begins on the first day of the first month they no longer qualify under this provision.
Equitable Relief
Under certain circumstances, a SEP may be created and/or late-enrollment penalties may be waived if a Medicare beneficiary can establish that an error, misrepresentation, or inaction of a federal worker or an agent of the federal government (such as an employee of the Social Security Administration, CMS, or a Medicare administrative contractor) resulted in late Part B enrollment.4544 To qualify for an exception under these conditions, the beneficiary must provide documentary evidence of the error, which "can be in the form of statements from employees, agents, or persons in authority that the alleged misinformation, misadvice, misrepresentation, inaction, or erroneous action actually occurred."46
Time-limited equitable relief also may be granted for certain categories of individuals. For example, CMS is providing equitable relief during September 1, 2017, through May 31, 2018, to individuals affected by recent hurricanes who were unable to enroll in Medicare during their initial enrollment periods.47may provide a special enrollment period to those affected by a weather related emergency or a major disaster.46 Additionally, as described in more detail below, CMS determined that it did not provide adequate information regarding Part B enrollment to certain individuals with exchange coverage who enrolled in Medicare Part A and is allowing equitable relief to these individuals through September 20182019.
Limited Time Equitable Relief for Individuals with Medicare Part A and Exchange Coverage
CMS generally encourages those who have coverage through an individual exchange (also known as marketplace) plan, and subsequently become eligible for Medicare, to drop the exchange coverage and enroll in Medicare during their initial enrollment period. After an individual has become eligible for Medicare Part A, any tax credits and cost-sharing reductions that individual receives through an exchange plan end.4847 CMS recognized that "many of these individuals did not receive the information necessary at the time of their Medicare [initial enrollment period or initial enrollment in coverage through the [exchange]], Part B SEP for the working aged or disabled, or initial enrollment in the Exchange to make an informed decision regarding their Medicare Part B enrollment."4948 This may have resulted in these individuals not enrolling in Part B, or enrolling in Part B late and being subject to a late enrollment penalty.
CMS is thus offering time-limited equitable relief through September 30, 20182019, for certain individuals enrolled in both premium-free Medicare Part A and in a plan provided through the health insurance exchanges.5049 Specifically, those who are currently, or had previously been, enrolled in an exchange plan and in premium-free Medicare Part A, and had an initial enrollment period that began on or after April 1, 2013, (or a Part B SEP that ended on or after October 1, 2013) may enroll in Part B without penalty through September 30, 20182019. Additionally, the Part B late enrollment penalties of those who had both Part A and exchange coverage and signed up for Part B outside of their initial enrollment period may be reduced or eliminated. To request this equitable relief, qualifying individuals must contact the Social Security Administration and provide appropriate documentation indicating that they were enrolled in an exchange plan and eligible for Medicare during the specified period.51
Collection of the Part B Premium
Part B premiums may be paid in a variety of ways.5251 If an enrollee is receiving Social Security or Railroad Retirement benefits,5352 the Part B premiums must, by law, be deducted from these benefits. Additionally, Part B premiums are deducted from the benefits of those receiving a Federal Civil Service Retirement annuity.5453 The purpose of collecting premiums by deducting them from benefits is to keep premium collection costs at minimum.
This withholding does not apply to those beneficiaries receiving state public assistance through a Medicare Savings Program because their premiums are paid by their state Medicaid program. (See "Premium Assistance for Low-Income Beneficiaries.") Additionally, premium payments may be made on behalf of Medicare beneficiaries by an employee, union, lodge, or other organization, or by an entity of a state or local government if it enters into a group-billing arrangement with CMS. Those approved as group billers include such entities as city and county governments, state teacher retirement systems, and certain religious orders.
Any
Part B enrollees whose premiums are not deducted from Social Security, Railroad Retirement, or Civil Service Retirement monthly benefits; are paid by Medicaid; or paid under an approved group-billing arrangement by a privateare paid by another person or organization must pay premiums directly to CMS.55
Deduction of Part B Premiums from Social Security Checks
By law, a Social Security beneficiary who is enrolled in Medicare Part B must have the Part B premium automatically deducted from his or her Social Security benefits.5655 Automatic deduction from the Social Security benefit check also applies to Medicare Advantage participants who are enrolled in private health care plans in lieu of traditional Medicare.5756 In 20172018, about 7568% of Medicare Part B enrollees (3940.7 million) had their Part B premiums deducted from their Social Security benefit checks.5857
Social Security beneficiaries who do not pay Medicare Part B premiums include those who are under the age of 65 and do not yet qualify for Medicare (e.g., began receiving Social Security benefits at the age of 62); receive low-income assistance from Medicaid to pay the Part B premium; have started to receive Social Security disability insurance (SSDI) but are not eligible for Medicare Part B because they have not received SSDI for 24 months; or chose not to enroll in Medicare Part B.
The amount of an individual's Social Security benefits cannot go down from one year to the next as a result of the annual Part B premium increase, except in the case of higher-income individuals subject to income-related premiums. (See "Protection of Social Security Benefits from Increases in Medicare Part B Premiums.") For those beneficiaries "held harmless," the dollar amount of their Part B premium increases would be held below or equal to the amount of the increase in their monthly Social Security benefits.
Part B Enrollees Who Do Not Receive Social Security Benefits
A small percentage of Medicare Part B enrollees do not receive Social Security benefits. For example, some individuals aged 65 and older may have deferred signing up for Social Security for various reasons, for instance if they have not yet reached their full Social Security retirement age5958 or are still working. Additionally, certain persons who spent their careers in employment that was not covered by Social Security—including certain federal, state, or local government workers and certain other categories of workers—do not receive Social Security benefits but may still qualify for Medicare. For those who receive benefit payments from the RRB6059 or the Civil Service Retirement System (CSRS),6160 Part B premiums are deducted from the enrollees' monthly benefit payments. While RRB retirement benefit amounts are protected by the hold-harmless provision, CSRS benefits are not held harmless from annual increases in the Part B premium.
For those who do not receive these types of benefit payments, Medicare will generally bill directly for their premiums every three months.6261 The enrollee who is being billed does not necessarily have to pay his or her own premiums; premiums may be paid by the enrollee, a relative, friend, organization, or anyone else.63 Additionally, in62 In cases where an organization wants to be billed for the Part B premiums of a number of Medicare beneficiaries, it may enter into a formal group-billing arrangement with CMS.63 Those approved as group billers include such entities as city and county governments, state teacher retirement systems, and certain religious orders.
In instances in which a beneficiary's monthly Social Security benefit is not sufficient to cover the entire Part B premium amount, Medicare may bill the beneficiary for the balance.64 Nonpayment of premiums results in termination of enrollment in the Part B program, although a grace period (through the last day of the third month following the month of the due date) is allowed for beneficiaries who are billed and pay directly.65
Determining the Part B Premium
Each year, the CMS actuaries estimate total per capita Part B costs for beneficiaries aged 65 and older over for the following year and set the Part B premium to cover 25% of expected Part B expenditures.66 However, because prospective estimates may differ from the actual spending for the year, contingency margin adjustments are made to ensure sufficient income to accommodate potential variation in actual expenditures during the year. (See "Contingency Margin.") The Part B premium is a single national amount that does not vary with a beneficiary's age, health status, or place of residence. Premiums may be adjusted upward for late enrollment (see "Late-Enrollment Premium Penalty and Exemptions") and for beneficiaries with high incomes (see "Income-Related Premiums"), or they may be adjusted downward for those protected by the hold-harmless provision (see "Protection of Social Security Benefits from Increases in Medicare Part B Premiums").
Monthly Part B premiums are based on the estimated amount that would be needed to finance Part B expenditures on an incurred basis during the year. In estimating needed income and to account for potential variation, CMS takes into consideration the difference in prior years of estimated and actual program costs, the likelihood and potential impact of potential legislation affecting Part B in the coming year, and the expected relationship between incurred and cash expenditures (e.g., payments for some services provided during a particular year may not be paid until the following year). Once the premium has been set for a year, it will not be changed during that year.
While both aged and disabled Medicare beneficiaries may enroll in Part B, the statute provides that Part B premiums are to be based only on the expected program costs—that is, the monthly actuarial rate—for the aged (those 65 years of age and older).67 The actuarial rate for the aged is defined as one-half of the expected average monthly per capita program costs for the aged plus any contingency margin adjustments. Standard Part B premiums are one-half of the actuarial rate. (See Appendix A for a discussion of the history of the premium methodology.) Part B costs not covered by premiums are paid for through transfers from the General Fund of the Treasury. The monthly actuarial rates for both aged and disabled enrollees are used to determine the needed amount of matching general revenue funding.68
Starting in 2016, a $3.00 per month surcharge is being added onto the standard premium (higher amounts for high-income individuals). To mitigate the expected large premium increases for those not held harmless in 2016, the Bipartisan Budget Act of 2015 (BBA 15; P.L. 114-74) required that 2016 Medicare Part B premiums be set as if the hold-harmless rule were not in effect—in other words, to calculate premiums as if all enrollees were paying the same annual inflation-adjusted standard premium. (For additional information on the changes made by BBA 15, see Appendix D.) To compensate for the lost premium revenue (below the required 25%) and to ensure that the SMI Trust Fund had adequate income to cover payments for Part B benefits in 2016, the act allowed for additional transfers from the General Fund of the Treasury to the SMI Trust Fund. To offset the approximately $9 billion in increased federal spending in 2016 resulting from the reduction in standard premiums for those not held harmless, a $3.00 surcharge was added to the monthly premium in 2016, and will continue to be applied in subsequent years until the additional federal costs are fully offset.69 For those who pay high-income premiums, the surcharge increases on a sliding scale up to $9.60. (See "Income Categories and Premium Adjustments.") It is estimated that the surcharge will be applied to premiums through 2021.70
Premium Calculation for 2018
2019
To determine the 20182019 monthly Part B premium amount,71 CMS first estimated the monthly actuarial rate for enrollees aged 65 and older using actual per-enrollee costs by type of service from program data through 20162017 and projected these costs through 20182019. CMS estimated that the monthly amount needed to cover one-half of the total benefit and administration costs for the aged in 20182019 would be $247.91263.47. However, because of expected variations between projected and actual costs, a contingency adjustment of $15.883.74 was added to this amount. (See "Contingency Margin," below.) After a reduction of $1.892.31 to account for expected interest on trust fund assets, the monthly actuarial rate for the aged was determined to be $261264.90. The 20182019 Part B standard premium is one-half of $261264.90, or $131.00132.50 per month72 (25% of the monthly expected per capita costs of the aged). The BBA 15 repayment surcharge of $3.00 was then added onto that amount for a total monthly premium of $134.00135.50. (As noted, only those not held harmless pay the standard 20182019 premium and surcharge. Those held harmless in 20182019 pay lower amounts.)
Contingency Margin
The contingency margin is the amount set aside to cover an appropriate degree of variation between actual and projected costs in a given year. For example, in some years, legislation that resulted in increased Medicare Part B expenditures for the year was enacted after the premium for the year had been set. The Medicare actuaries consider a contingency reserve ratio—net assets at the end of a year in the Part B account of the SMI Trust Fund compared to the following year's expected expenditures—in the amount of 15% to 20% to be adequate, and normally aim for a 17% ratio when determining Part B financing for the upcoming year. Financing fell short of this goal in 20172018; however, the CMS actuaries estimate that the 20182019 premium rates will allow asset levels in the Part B account to increase to appropriate levels by the end of 20182019.
The contingency margin in 20182019 is affected by a number of factors. Because about 283.5% of Part B enrollees are being held harmless and pay reduced premiums in 20182019, the premiums of the remaining 7296.5% were adjusted so that aggregate premiums would still cover 25% of Part B costs in 20182019. This increase is included in the contingency margin. Additionally, starting in 2011, manufacturers and importers of brand-name drugs began paying a fee that is allocated to the SMI Trust Fund. The contingency margin was thus reduced to account for this additional revenue. Further, certain payment incentives to encourage the development and use of health information technology (HIT) by Medicare physicians are excluded from premium determinations. (HIT bonuses or penalties are directly offset through transfers of general funds from the Treasury.) The 20182019 contingency margin adjustment of $15.883.74 reflects the expected net effects of all of the above factors.
Income-Related Premiums
For the first 41 years of the Medicare program, all Part B enrollees paid the same Part B premium, regardless of their income. However, the Medicare Modernization Act of 2003 (MMA; P.L. 108-173)73 required that, beginning in 2007, high-income enrollees pay higher premiums.74 About 3.56 million Medicare Part B enrollees (about 6.6%) paid%) pay these higher premiums in 2018.75
Adjustments, known as income-related monthly adjustment amounts (IRMAA), are made to the standard Part B premiums for high-income beneficiaries, with the share of expenditures paid by beneficiaries increasing with income. This share ranges from 35% to 8085% of the value of Part B coverage. In 20182019, individuals whose incomes exceed $85,000 and couples whose combined income exceeds $170,000 are subject to higher premium amounts.76 The hold-harmless provision that prevents a beneficiary's Social Security benefits from decreasing from one year to the next as a result of the Part B premium increase does not apply to those subject to an income-related increase in their Part B premiums. (See "Protection of Social Security Benefits from Increases in Medicare Part B Premiums.")
Determination of Income
To determine those subject to the high-income premium, Social Security uses the most recent federal tax return provided by the Internal Revenue Service. In general, the taxable year used in determining the premium is the second calendar year preceding the applicable year. For example, the 20172018 tax return (20162017 income) was used to determine who wouldwould pay the 20182019 high-income premiums.77
The income definition on which the high-income premiums are based is modified adjusted gross income (MAGI),78 which is different from gross income. Specifically, gross income is all income from all sources, minus certain statutory exclusions (e.g., nontaxable Social Security benefits).79 From gross income, adjusted gross income (AGI)80 is calculated to reflect a number of deductions, including trade and business deductions and losses from sale of property. MAGI is defined as AGI plus certain foreign-earned income and tax-exempt interest.81
If a person had a one-time increase in taxable income in a particular year (such as from the sale of income-producing property), that increase would be considered in determining the individual's total income for that year and thus his or her liability for the income-related premium two years ahead. It would not be considered in the calculations for future years.
In the case of certain major life-changing events that result in a significant reduction in MAGI, an individual may request to have the determination made for a more recent year than the second preceding year.82 Major life-changing events include (1) death of a spouse; (2) marriage; (3) divorce or annulment; (4) partial or full work stoppage for the individual or spouse; (5) loss by individual or spouse of income from income-producing property when the loss is not at the individual's direction (such as in the case of a natural disaster); and (6) reduction or loss for individual or spouse of pension income due to termination or reorganization of the plan or scheduled cessation of the pension.83 Certain types of events, such as those that affect expenses but not income or those that result in the loss of dividend income because of the ordinary risk of investment, are not considered major life-changing events.84
If Medicare enrollees disagree with decisions regarding their IRMAAs, they may file an appeal with Social Security. Enrollees may either submit a "Request for Reconsideration"85 or contact their local Social Security office to file an appeal. (An enrollee does not need to file an appeal if he or she is requesting a new decision based on a life-changing event described above or if the enrollee has shown that Social Security used the wrong information to make the original decision.)
Income Categories and Premium Adjustments
Depending on their level of income, Medicare beneficiaries may be classified into one of fivesix income categories.86 In 20182019, individuals with incomes less than $85,000 a year ($170,000 for a couple) pay the standard premium, which is based on 25% of the average Part B per capita cost. Individuals with incomes over $85,000 per year and couples with combined income over $170,000 per year pay a higher percentage of Part B costs. Depending on one's level of income over these threshold amounts, premiums may be adjusted to cover 35%, 50%, 65%, 80%, or 85or 80% of the value of Part B coverage (with the rest being subsidized through federal general revenues).87 Additionally, high-income individuals pay surcharges ranging from $4.20 to $9.6010.20 per month to offset increased federal spending in 20182019 due to premium reductions under BBA 15 (compared to a $3.00 surcharge for those who pay the standard premium). In 20182019, total IRMAAs for the fourfive high-income levels, including the additional BBA 15 surcharges, are $53.50, $133.90, $214.30, and $294.60,54.10, $135.40, $216.70, $297.90, and $325.00 respectively.
The income categories and associated premiums for 20182019, including the applicable BBA 15 repayment surcharges, are shown below in Table 2. When both members of a couple are enrolled in Part B, each pays the applicable premium amount.
|
Levels of Premium Adjustment and Percentage of Costs Covered by Premiums |
Beneficiaries Who File an Individual Tax Return with Income |
Beneficiaries Who File a Joint Tax Return with Incomea |
Income-Related Monthly Adjustment Amount (IRMAA)b |
Total Monthly Premium (premium + surcharge) |
||||
|
Held Harmless |
Less than or equal to $85,000 |
Less than or equal to $170,000 |
n/a |
Less than $ |
||||
|
Not Held Harmless |
||||||||
|
Standard (25%) |
Less than or equal to $85,000 |
Less than or equal to $170,000 |
n/a |
134.00 |
||||
|
High Income |
||||||||
|
Level 1 (35%) |
Greater than $85,000 and less than or equal to $107,000 |
Greater than $170,000 and less than or equal to $214,000 |
$ |
187.50 |
||||
|
Level 2 (50%) |
Greater than $107,000 and less than or equal to $133,500 |
Greater than $214,000 and less than or equal to $267,000 |
133.90 |
|
||||
|
Level 3 (65%) |
Greater than $133,500 and less than or equal to $160,000 |
Greater than $267,000 and less than or equal to $320,000 |
214.30 |
348.30 |
||||
|
Level 4 (80%) |
Greater than $160,000 and less than $500,000 |
Greater than $320,000 and less than $750,000 |
294.60 |
428.60
|
Level 5 (85%)
|
Greater than or equal to $500,000
|
Greater than or equal to $750,000
|
325.00 460.50 |
Source: CMS, "Medicare Program: Medicare Part B Monthly Actuarial Rates, Premium Rate, and Annual Deductible Beginning January 1, 2018," 822019," 83 Federal Register 55370, November 21, 201752462, October 17, 2018.
Notes: The hold-harmless provision does not apply to individuals in the high-income categories. n/a = not applicable.
a. Couples with a joint income of $170,000 or less could pay different premium amounts if one of them qualifies to be held harmless and the other does not. Members of a couple in the high-income categories both pay the same applicable income-adjusted premium amount.
b. Total income-related monthly adjustment amounts (IRMAAs) are the amounts by which total monthly premiums exceed the standard premium ($134.00).
c. Because there was a relatively small Social Security COLA in 2018, the135.50).
c. The premiums of those protected under the hold-harmless rule may vary depending on the amount of the actual increase in their Social Security benefits.
Married persons who lived with their spouse at some point during the year but who filed separate returns are subject to different premium amounts. The income levels and premium amounts are shown in Table 3.
|
Beneficiaries Who Are Married and Lived with Their Spouse at Any Time During the Year but File a Separate Tax Return from Their Spouse with Income |
Income-Related Monthly Adjustment Amount (IRMAA)a |
Total Monthly Premium (premium + surcharge) |
||||
|
Held Harmless |
||||||
|
Less Than or Equal to $85,000 |
n/a |
Less than $ |
||||
|
Not Held Harmless |
||||||
|
Less Than or Equal to $85,000 |
n/a |
134.00 |
||||
|
Greater Than $85,000 |
$294.60 |
428.60
|
$297.90
|
433.40
|
Greater than or equal to $415,000
|
325.00 460.50 |
Source: CMS, "Medicare Program: Medicare Part B Monthly Actuarial Rates, Premium Rate, and Annual Deductible Beginning January 1, 2018," 822019," 83 Federal Register 55370, November 21, 201752462, October 17, 2018.
Notes: n/a = not applicable.
a. Total income-related monthly adjustment amounts (IRMAAs) are the amounts by which total monthly premiums exceed the standard premium ($134.00).
b. Because there was a small Social Security COLA in 2018, the135.50).
b. The premiums of those protected under the hold-harmless rule may vary depending on the amount of the actual increase in their Social Security benefits.
Income Thresholds
The original provision establishing the Part B income-related premiums set the initial income threshold and high-income-level ranges. Prior to 2010, annual adjustments to these levels were based on annual changes in the consumer price index for urban consumers (CPI-U), rounded to the nearest $1,000. However, Section 3402 of the Patient Protection and Affordable Care Act (ACA; P.L. 111-148, as amended) froze the income thresholds and ranges at the 2010 level through 2019 rather than allowing them to rise with inflation.88 As a result, as incomes have increased with inflation, a greater share of Medicare enrollees are reaching the high-income thresholds and paying the high-income premiums than would have been the case without this freeze.
Additionally, beginning in 2018, the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA; P.L. 114-10) changed the income thresholds inof the top two income categories at that time.89 Individuals with incomes between $133,500 and $160,000 per year are now in the 65% applicable percentage category (which previously applied to those with incomes between $160,000 and $214,000 in 2010-2017). The income threshold for the highest category (80%) is nowat that time (80%) was changed to $160,000 (which previously applied to $214,000 in 2010-2017). The thresholds for the lower two income categories remain unchangedwere not changed. (See Table 4.)
In 2019, the With the exception of the addition of a new top threshold category described below, the 2019 income thresholds for the current categories will remainhigh-income categories are the same as in 2018. For years 2020 and after, the thresholds will be adjusted annually for inflation based on the new (2018 and 2019) threshold levels.90
Section 53114 of the Bipartisan Budget Act of 2018 (BBA 18; P.L. 115-123) addsadded an additional high-income category beginning in 2019 for individuals with annual income of $500,000 or more or couples filing jointly with income of $750,000 or more. (See Table 4.) Enrollees with income equal to or exceeding these thresholds will pay premiums that cover 85% of the average per capita cost of the Parts B and D benefits instead of 80%. The threshold for couples filing jointly in this new income tier will beis calculated as 150% of the individual income level rather than 200% as in the other income tiers. This new top income threshold will be frozen through 2027 and will be adjusted annually for inflation starting in 2028 based on the CPI-U.91
|
Levels of Premium Adjustment and Percentage of Costs Covered by Premiums |
Beneficiaries Who File Individual Tax Returns with Income: |
Beneficiaries Who File Joint Tax Returns with Income: |
||||||
|
2017 |
2018 |
2019 |
2017 |
2018 |
2019 |
|||
|
Standard (25%) |
Less than or equal to $85,000 |
Less than or equal to $85,000 |
Less than or equal to $85,000 |
Less than or equal to $170,000 |
Less than or equal to $170,000 |
Less than or equal to $170,000 |
||
|
High Income |
||||||||
|
Level 1 (35%) |
$85,001*- $107,000 |
$85,001-$107,000 |
$85,001-$107,000 |
$170,001-$214,000 |
$170,001-$214,000 |
$170,001-$214,000 |
||
|
Level 2 (50%) |
$107,001-$160,000 |
$107,001-$133,500 |
$107,001-$133,500 |
$214,001-$320,000 |
$214,001-$267,000 |
$214,001-$267,000 |
||
|
Level 3 (65%) |
$160,001-$214,000 |
$133,501-$160,000 |
$133,501-$160,000 |
$320,001-$428,000 |
$276,001-$320,000 |
$267,001-$320,000 |
||
|
Level 4 (80%) |
More than $214,000 |
More than $160,000 |
$160,001-$499,999 |
More than $428,000 |
More than $320,000 |
$320,001-$749,999* |
||
|
Level 5 (85%) |
n/a |
n/a |
$500,000 or more |
n/a |
n/a |
$750,000 or more |
||
Source: CMS, Annual Notices, "Medicare Program; Medicare Part B Monthly Actuarial Rates, Premium Rate, and Annual Deductible," for 2017 and, 2018, and §53114 of BBA 18 for 2019.
Notes: * Bottom thresholds in Levels 2 through 4 rounded up to the nearest dollar and upper threshold in 2019 Level 4 rounded down to the nearest dollar; n/a = not applicable.
Premium Assistance for Low-Income Beneficiaries
Medicare beneficiaries with limited incomes and resources may be able to qualify for assistance with their premiums and other out-of-pocket expenses.92 About one in five Medicare beneficiaries receives Part B premium subsidies.
Medicare beneficiaries who qualify for full Medicaid benefits (full dual-eligibles) have most of their health care expenses paid for by either Medicare or Medicaid. For these individuals, Medicaid covers the majority of Medicare premium and cost-sharing expenses, and it supplements Medicare by providing coverage for services not covered under Medicare, such as dental services and long-term services and supports. In cases where services are covered by both Medicare and Medicaid, Medicare pays first and Medicaid picks up most of the remaining costs. Each state has different rules about eligibility and applying for Medicaid.93
Beneficiaries who do not meet their respective state's eligibility criteria for Medicaid may still qualify for assistance with Part B premiums if they have incomes of less than 135% of the federal poverty level (FPL) and assets of less than $7,560730 for an individual or $11,340600 for a couple in 20182019.94 These assistance programs are commonly referred to as Medicare Savings Programs (MSPs).95 Three of these programs provide assistance with Part B premiums. The type of assistance is based on a beneficiary's level of income.
Qualified Medicare Beneficiaries
Aged or disabled persons with incomes at or below FPL may qualify for the Qualified Medicare Beneficiary (QMB) program.96 In 20182019, the QMB monthly qualifying income levels are $1,032061 for individuals and $1,392430 for a couple (annual income of $12,384732 and $16,70417,160, respectively).97 QMBs are entitled to have their Medicare Parts A and B cost-sharing charges, including the Part B premium and all deductibles and coinsurance, paid by Medicaid.98 (See Table 5.) For QMBs, Medicaid coverage is limited to the payment of Medicare premiums and cost-sharing charges (i.e., the Medicare beneficiary is not entitled to coverage of Medicaid plan services, unless the individual is otherwise entitled to Medicaid).
Specified Low-Income Medicare Beneficiaries
Individuals whose income is more than 100% but less than 120% of FPL may qualify for assistance as a Specified Low-Income Medicare Beneficiary (SLMB). In 20182019, the monthly income limits are $1,234269 for an individual and $1,666711 for a couple (annual income of $14,808 and $19,99215,228 and $20,532, respectively).99 Medicaid pays the Medicare Part B premiums for SLMBs, but not other cost sharing.
Qualifying Individuals
Individuals whose income is between 120% and 135% of FPL may qualify for assistance as Qualifying Individuals (QIs). In 20182019, the monthly income limit for a QI is $1,386426 for an individual, and for a couple, it is $1,872923 (annual income of $16,632 and $22,46417,112 and $3,076, respectively). Medicaid protection for these individuals is limited to payment of the monthly Medicare Part B premium. Expenditures under the QI program are, however, paid for (100%) by the federal government from the Medicare SMI Trust Fund up to the state's allocation level.100 A state is required to cover only the number of people that would bring the state's spending on these population groups in a year up to its allocation level. Any expenditures beyond that level are voluntary and paid entirely by the state.
Funding for the QI program was first made available by the Balanced Budget Act of 1997 (BBA97; P.L. 105-33).101 Subsequent legislation extended the program and the amounts available through allocation.102 MACRA permanently extended the QI program.103
|
Monthly Incomea |
Resourcesb |
Benefits |
|
|
Qualified Medicare Beneficiary (QMB) |
At or Below 100% FPLc $1, $1, |
$7, $11, |
Part B Premiumd Coverage of Parts A and B Deductibles and Coinsurance |
|
Specified Low-Income Medicare Beneficiary (SLMB) |
Above 100% but Less Than 120% FPLc $1, $1, |
$7, $11, |
Part B Premium |
|
Qualifying Individual (QI) |
At or Above 120% but Less Than 135% FPLc $1, $1, |
$7, $11, |
Part B Premium |
Source: Social Security Program Operations Manual, HI 00815.023 Medicare Savings Programs Income Limits, at https://secure.ssa.gov/poms.nsf/lnx/0600815023.
a. These amounts include a $20 general income exclusion, under which $20 from any income is not counted toward the income limits. CMS rounds up to the nearest dollar when computing monthly income limits.
b. Resources include money in checking and savings accounts, stocks, bonds, mutual funds, and Individual Retirement Accounts (IRAs). Resources do not include one's primary residence, a life insurance policy worth up to $1,500, one car, burial plots, up to $1,500 per person for burial expenses, and household items. Some states have no limits on resources.
c. Federal Poverty Levels (FPLs) are updated each year, usually in January or February. Income levels are higher for Hawaii and Alaska and for those living with dependents.
d. Most people do not pay a premium for Part A because they have worked 40 or more quarters in covered employment. For those without sufficient work history to qualify for premium-free Part A, Medicaid will also pay Part A premiums for QMBs.
Protection of Social Security Benefits from Increases in Medicare Part B Premiums
After a person becomes eligible to receive Social Security benefits, his or her monthly benefit amount is adjusted annually to compensate for increases in the prices of goods and services over time.104 Near the end of each year, the Social Security Administration announces the cost-of-living adjustment (COLA) payable in January of the following year. The amount of the COLA is based on inflation as measured by the Consumer Price Index-Urban Wage Earners and Clerical Workers (CPI-W).105 If the CPI-W decreases, Social Security benefits stay the same—benefits are not reduced during periods of deflation.
When the annual Social Security COLA is not sufficient to cover the standard Medicare Part B premium increase, most Medicare beneficiaries are protected by a hold-harmless provision in the Social Security Act.106 Specifically, if in a given year the increase in the standard Part B premium would cause a beneficiary's Social Security check to be less, in dollar terms, than it was the year before, then the Part B premium is reduced to ensure that the amount of the individual's Social Security check does not decline.107 This determination is made by the Social Security Administration.
To be held harmless in a given year, a Social Security beneficiary must have received Social Security benefit checks in both December of the previous year and January of the current year, and the beneficiary must also have had Part B premiums deducted from both checks.108 The hold-harmless provision operates by comparing the net dollar amounts of the two monthly benefit payments; if the net Social Security benefit for January of the current year is lower than in December of the previous year, then the hold-harmless provision applies to that person. Premiums of those held harmless are then reduced to an amount that would not cause their Social Security benefits to decline in the next year. The premium paid by those held harmless is called the Variable Supplementary Medical Insurance premium.109 Those not held harmless pay the standard premium as determined for that year.
Typically, the hold-harmless provision affects only a small number of beneficiaries and has had minimal impact on Part B financing.110 In most years, this rule primarily protects those with relatively low Social Security payments. However, in years in which there is no or a very low Social Security COLA, such as in 2010, 2011, 2016, and 2017, a large number of beneficiaries may be protected by this provision. (See "Application of the Hold-Harmless Rule in Years Prior to 2016," "Application of the Hold-Harmless Rule in 2016," and "Application of the Hold-Harmless Rule in 2017.")
Some Beneficiaries Are Not Protected by the Hold-Harmless Provision
Not all beneficiaries are protected by the hold-harmless provision and, under some circumstances, may be subject to significantly higher premiums than those who are held harmless. Groups that are not protected include the following:
- Higher-Income Beneficiaries. Higher-income beneficiaries who are required to pay income-related Part B premiums are explicitly excluded by law from protection under the hold-harmless provision. They are required to pay the full amount of any increase in their Part B premiums. (See "Income-Related Premiums.")
- Lower-Income Beneficiaries. Lower-income beneficiaries who receive premium assistance from Medicaid are not held harmless as their premiums are not deducted from their Social Security benefits. However, the Medicaid program pays the full amount of any increase in their Part B premiums. (See "Premium Assistance for Low-Income Beneficiaries.")
- Those Who Do Not Receive Social Security. This group includes those who have not yet signed up for Social Security for various reasons, for example because they have deferred signing up because they have not reached full retirement age111 or are still working. It also includes disabled beneficiaries whose Social Security Disability Insurance (SSDI) cash benefits have been discontinued because they have returned to work but who are still eligible for Medicare.112 Additionally, those who receive benefits exclusively through a different retirement plan are not held harmless.113 This group includes certain federal retirees under the Civil Service Retirement System114 as well as certain state and local government workers—such as teachers, law-enforcement personnel, and firefighters—who have their own pension programs.115
- Those Who Did Not Have Medicare Premiums Deducted from Their Social Security Checks at the End of One Year and the Beginning of the Next. This category includes those who enroll in Social Security or Medicare during the year in which the hold-harmless provision is in effect, including SSDI recipients who become eligible for Medicare that year after the 24-month waiting period.116 It also includes those who had Medicare premiums paid on their behalf one year, for example by Medicaid, but lost that coverage during the next year.
Some people protected by the hold-harmless provision may still see a decrease in their Social Security checks due to an increase in Medicare Part D premiums. Part D premiums are not covered by the hold-harmless provision, although beneficiaries with low-income subsidies would not be affected.
Additionally, those who pay the late-enrollment penalty are not fully protected from the hold-harmless rule. (See "Late-Enrollment Premium Penalty and Exemptions.") In a year in which the hold-harmless provision is in effect, the late-enrollment surcharges are calculated as a percentage of the premiums of those not held harmless. These surcharges are considered "nonstandard" premiums and thus are not limited by the hold-harmless provision.
Application of the Hold-Harmless Rule in Years Prior to 2016
As described earlier, an individual's Social Security COLA is determined by multiplying his or her benefit amount by the inflation rate, the CPI-W. Part B premiums are determined by projected Part B program costs. Thus, the number of people held harmless can vary widely from year to year, depending on inflation rates and projected Part B costs. For most years, the hold-harmless provision has affected a relatively small number of beneficiaries.117 However, due to low inflation, no COLA adjustments were made to Social Security benefits in 2010 and 2011. Most Medicare beneficiaries (about 73%) were protected by the hold-harmless provision and continued to pay the 2009 standard monthly premium of $96.40 in both 2010 and 2011.118 Because Part B expenditures were still expected to increase in those years, and because beneficiary premiums are required to cover 25% of those costs, the premiums for those not held harmless (27% of beneficiaries) were higher than they would have been had the rest of the beneficiaries not been held harmless. The standard monthly premiums paid by those not held harmless were $110.50 in 2010 and $115.40 in 2011.119 In 2011, of the 27% who were not eligible to be held harmless, about 3% were new Medicare enrollees, about 5% were high-income, about 17% had their premiums paid for by Medicaid, and the remaining 2% did not have their premiums withheld from Social Security benefit payments.
In 2012 and 2013, Social Security beneficiaries received a 3.6% and a 1.7% COLA, respectively, which more than covered the Part B premium increases in those years; therefore, the hold-harmless provision was not applicable for most beneficiaries. Similarly, in 2014 and 2015, with a Social Security COLA increase of 1.5% and 1.7%, respectively, and no increase in Part B premiums, the hold-harmless provision also was not broadly applicable in those years.120
Application of the Hold-Harmless Rule in 2016
In 2016, for a third time, there was no Social Security COLA increase, but there was a projected increase in Medicare Part B premiums—from $104.90 per month in 2015 to about $121 per month in 2016.121 Similar to its application in 2010 and 2011, the hold-harmless provision as applied in 2016 protected some beneficiaries but not others. In 2016, about 70% of Part B enrollees were held harmless and continued to pay the 2015 monthly premium amount of $104.90 through 2016. Those not held harmless included those eligible for premium assistance through their state Medicaid programs (about 19%), those who paid the high-income premiums (about 6%), those who did not receive Social Security benefits (3%), and new enrollees in 2016 (5%).122
Absent legislation, the premiums of those not held harmless (the remaining 30%) would have been higher than the premiums would have been had the hold-harmless provision not been in effect.123 However, BBA 15 mitigated the expected large increases for those not held harmless and required that their premiums be calculated as if the hold-harmless rule were not in effect. BBA 15 also required that a monthly surcharge of $3.00 be added to standard premiums (more for those with high incomes) until the increased cost to the federal government of reducing the premiums is offset. (See Appendix D.) The total standard premium amount for those Part B enrollees not held harmless in 2016, including the $3.00 per month surcharge, was $121.80.124
Application of the Hold-Harmless Rule in 2017
Should there have been a 0% Social Security COLA in 2017, BBA 15 would have allowed for a similar Medicare Part B premium setting mechanism for 2017 as in 2016. However, as there was a very small (0.3%) Social Security COLA in 2017, this provision did not apply.
Because the Social Security COLA was not large enough to cover the full Medicare Part B premium increase, about 70% of enrollees were held harmless in 2017. Those held harmless in 2017 paid, on average, about $109.00 per month for their Part B premiums. However, their actual premiums varied depending on the dollar amount of the increase in their Social Security benefit.125 Additionally, many of those not held harmless in 2016 because they were new to Medicare in that year may have qualified to be held harmless in 2017. If they qualified, the premiums for those individuals would have been equal to the 2016 premium of $121.80, plus the dollar amount of the increase in their monthly Social Security benefit.
As the premiums of those not held harmless (the remaining 30% of enrollees) had to cover both their share of the premium increases plus that of the 70% held harmless,126 the Medicare trustees estimated that their 2017 Part B premiums could be as high as $149 per month.127 However, in setting the 2017 premiums, the Secretary "exercised her statutory authority to mitigate projected premium increases for these beneficiaries"128 by setting a lower-than-normal contingency reserve ratio for the SMI Trust Fund in 2017. This had the effect of reducing premiums below what they might have been had the ratio been set at a more conventional level.129 In 2017, those not held harmless paid monthly premiums of $134.00.
Application of the Hold-Harmless Rule in 2018
In 2018, there was a 2.0% Social Security COLA and no increase in the 2018 Medicare Part B premiums (i.e., the Part B premium was $134.00 per month in both 2017 and 2018).130 For many Part B enrollees who were held harmless in 2017, the Social Security COLA was large enough to cover the difference between the full Medicare premium of $134.00 and the reduced premium amount they paid in 2017. Therefore, many of those held harmless in 2017 are no longer seeingsaw reduced premiums in 2018 and have returned to paying the standard premium amounts (which include the $3.00 BBA 15 surcharge).
To illustrate, for someone receiving a Social Security benefit of $1,404.00 per month in 2017 (the average amount for retired workers in that year),131 a 2.0% Social Security COLA would have resulted in an increased benefit of about $28.00 per month in 2018. If that person had been held harmless in 2017 and was paying a Medicare Part B premium of $109.00 per month, this Social Security benefit increase would have been more than enough to cover the $25.00 difference between that individual's reduced Part B 2017 premium amount of $109.00 and the 2018 premium of $134.00. Therefore, that person's Medicare Part B premiums could have increased up to the full premium amount of $134.00 in 2018.
CMS estimatesestimated that about 72% of Part B enrollees are not being were not held harmless in 2018.132 About 42% of enrollees were held harmless in 2017 but no longer qualifyqualified for reduced premiums in 2018 because they did not meet the requirement that their Social Security benefits would decrease as a result of the increase in their Part B premiums. The remaining 30% includesincluded those who normally do not qualify to be held harmless, for instance, because they paypaid high-income premiums, havehad their premiums paid on their behalf by Medicaid, or dodid not receive Social Security benefits.
About 28% of Part B enrollees did not receive a large enough increase in their Social Security COLAs to cover the full amount of the Part B premium and thus The 2019 Social Security COLA of 2.8% was large enough to increase the benefits of most of those who were held harmless in 2018 to levels sufficient to cover the difference between the amount of the (reduced) premiums they paid in 2018 and the 2019 premiums of $135.50. In 2019, only about 3.5% of beneficiaries (about 2 million) are being held harmless and pay premiums lower than the 2019 premium of $135.50.qualifyqualified to be held harmless and paypaid reduced premiums in 2018. Their premiums could increasehave increased from the premium amount they paid in 2017, plus the dollar amount of the increase in their monthly 2018 Social Security benefit. For example, for someone with a monthly Social Security benefit of $600.00 in 2017, the 2.0% 2018 COLA would have provided an increase of about $12.00. If that individual had been paying $109.00 per month for Medicare premiums in 2017, the $12.00 increase would not behave been sufficient to cover the full $134.00 per month. In this example, the individual would payhave paid $109.00 plus $12.00 ($121.00) per month in 2018.
Application of the Hold-Harmless Rule in 2019
$109.00 plus $12.00 ($121.00) per month in 2018.
Part B Premiums over Time
Part B premium changes over time generally reflect the growth in total Part B expenditures, although the exact relationship between Part B expenditures covered by the Part B premium has been changed by statute at various points. (See Appendix A.) The standard monthly Part B premium has risen from $3.00 in 1966 to $134.00 in 2018135.50 in 2019. (See Figure 1.) For comparison, during a similar time period, average annual Part B benefit costs per beneficiary have increased from about $101.00 in 1970 (about $8.42 per month) to a projected $6,087391 per beneficiary (about $507.25532.60 per month) in 20182019.133
Prior to 2000, the Part B premium decreased from year to year twice. The first instance was from 1989 ($31.90) to 1990 ($28.60) as a result of the repeal of the Medicare Catastrophic Coverage Act of 1988 (P.L. 100-360). The second was from 1995 ($46.10) to 1996 ($42.50) as a result of the transition from a premium as determined by a fixed dollar amount under the Omnibus Reconciliation Act of 1990 (P.L. 101-508) to 25% of costs as directed under the Omnibus Budget Reconciliation Act of 1993 (P.L. 103-66).
More recently, because of the absence of a Social Security COLA in 2010 and 2011, most beneficiaries were held harmless and paid the 2009 premium of $96.40 per month during those years. The standard 2010 and 2011 premiums, paid by those who were not held harmless, were thus higher than they would have been had the hold-harmless provision not been in effect. (See prior section "Protection of Social Security Benefits from Increases in Medicare Part B Premiums" for additional detail.)
Since 2000, the standard Medicare Part B premium has almost tripled, from $45.50 in 2000 to the current premium of $134.00 in 2018135.50 in 2019. This growth has been due to a number of factors that have increased per capita Part B expenditures during that time, including the rising prices of health care services and equipment, new technologies, and increased utilization of Medicare Part B services.134 While Part B expenditure growth has slowed in recent years, the Medicare trustees project faster benefit spending growth over the next five years (an 8.2% Part B average annual growth rate compared with a 5.5% growth rate over the last five years).135
The Medicare trustees estimate that 20192020 premiums will increase to about $135.50141.10 per month, and that premiums will increase thereafter at an average rate of about 5.23% per year through 2027.134136 (For estimates of premiums in future years through 2027, see Appendix C.)
Current Issues
Premium Amount and Annual Increases
The Medicare trustees estimate that Medicare Part B premiums will increase from $134.00135.50 per month in 20182019 to about $202.70 in 2027. (See Appendix C.) Rising Medicare premiums could have a large effect on Social Security beneficiaries, particularly on those who rely on Social Security as their primary source of income.135137 For example, in 20172018, Social Security benefits represented about 33% of the income of Americans aged 65 and older. About 5048% of married couples and 7169% of unmarried persons received more than half of their income from Social Security, and 2321% of married couples and 4344% of unmarried persons received more than 90% of their income from Social Security.136138 Some of these beneficiaries may see a decline in their standard of living as their Medicare premiums rise.
Once a person receives Social Security, his or her benefit is indexed to inflation and thereafter grows with annual Social Security COLAs.137139 However, Medicare premiums are based on the per capita cost growth of Part B benefits, which reflects the growth in the cost of medical care and in the utilization and intensity of services used by beneficiaries, factors that have historically grown faster than CPI-W. Additionally, as there has been a continuing shift from providing care in inpatient (Part A) to outpatient settings (Part B), a greater portion of Medicare spending is expected to be covered by beneficiary premiums.138140 This means that, over time, Medicare premiums are expected to represent a growing proportion of most beneficiaries' Social Security income.139141 Since 2000, Social Security's annual COLA has resulted in a cumulative benefit increase of about 50%, significantly less than the Part B premium growth of close to 195200%. The Medicare trustees estimated that average Part B plus Part D premiums would represent close to 12% of the average Social Security benefit in 2018 and would increase to an estimated 17% in 2092.140142 (See Appendix B and Appendix C for historical, current, and projected Part B premiums.)
Additionally, while the hold-harmless provision provides protection against increases in the Part B premium, the rule does not apply to Part D premiums or to late-enrollment penalties. Therefore, even in a year with a 0% or a very low Social Security COLA, beneficiaries may still see a decline in benefits as a result of increases in Part D premiums and/or any applicable late-enrollment penalties.
Impact of the Hold-Harmless Provision on Those Not Held Harmless
The law does not specify how Medicare Part B financing (premiums and general revenues) should be established in years in which the hold-harmless provision applies to a large number of Medicare beneficiaries. Under current law, the only way to generate enough premium revenue to cover 25% of Part B costs is to have those not held harmless shoulder the entire beneficiary share of any increase in premiums.141143 Absent legislation such as BBA 15, the premiums of those not held harmless can therefore be significantly greater than if there were no hold-harmless provision. As the Medicare trustees pointed out in their 2010 annual report, "(t)his approach to preventing exhaustion of the Part B trust fund account is the only one available under current law," despite the "serious equity issues" that this method raises.142144
In years in which there has been both a 0% or a very low Social Security COLA and a Medicare premium increase, concerns have been raised about the potential financial impact of the premium increases on those not held harmless as well as on the state Medicaid agencies that pay Part B premiums on behalf of low-income beneficiaries. For example, individuals in retirement systems other than Social Security or RRB may also have not received a COLA but could face significantly higher Medicare premiums than those who qualified for protection under the hold-harmless provision.143145 Some have proposed changes to the hold-harmless provision to avoid the disproportionate impact of premium increases on those not held harmless, such as holding all Part B enrollees harmless in years in which there is no Social Security COLA144146 or allowing Social Security checks to decline as a result of Medicare premium increases in some years.145147 Others have proposed linking the Social Security COLA to a measure of inflation that is based on purchasing patterns of the elderly, such as the BLS's Experimental Consumer Price Index for Americans Aged 62 and Older (CPI-E)146148 or requiring a minimum annual Social Security COLA.147
Proposals to Modify the Late-Enrollment Penalty
Periodically, proposals have been offered to modify or eliminate the Part B premium penalty either for all enrollees or alternatively for a selected population group. As an increasing number of new Medicare-eligible beneficiaries must actively sign up for Medicare because they are not yet receiving Social Security benefits (e.g., their full retirement Social Security age exceeds the Medicare age of eligibility), there is concern that more people could become subject to late-enrollment penalties. For example, the Medicare Rights Center reported a large number of calls to its hotline related to transitioning to Medicare. Their report notes that "(m)any individuals who call Medicare Rights are confused by Medicare enrollment rules, and specifically by decision-making related to taking or declining Part B" and that "Medicare-eligible people who do not understand Part B enrollment rules and fail to enroll in Medicare when they first became eligible may face late-enrollment penalties, gaps in coverage, and disruptions to access to needed care."148
Some proposals have suggested modifying the penalty provision to limit both the amount and the duration of the surcharge, as is the case for delayed Part A enrollment, which has a maximum 10% surcharge and a duration of twice the number of years that enrollment was delayed. (See Appendix E for information on the Part A premium and late-enrollment penalty.)
Some have also suggested that Medicare Part B have a creditable-coverage exemption, similar to that under Part D, that would allow Medicare beneficiaries with equivalent coverage to postpone enrollment in Part B without being subject to a penalty. For example, under the Part D prescription drug benefit, individuals are not subject to a late-enrollment penalty if they have maintained "creditable" prescription drug coverage prior to enrollment—that is, coverage that is expected to pay at least as much as Medicare's standard prescription drug coverage.149151 Creditable prescription drug coverage includes employer-based prescription drug coverage, qualified State Pharmaceutical Assistance Programs, and military-related coverage (e.g., Veterans Affairs health care system and TRICARE).150152
Other suggestions include formally training employers about Medicare coverage and interaction with other insurance; improving education on Medicare, including late-enrollment penalties, for those nearing Medicare-eligibility age; and expanding equitable relief to include remedies for actions based on misinformation provided by entities in addition to an agent of the federal government, such as an agent of state or local government, and/or an employer or insurer.
In recent Congresses, a number of bills have been introduced that would address some of the issues associated with the Part B late-enrollment penalty. For example, in the 116th Congress, H.R. 1788 would limit the penalty to 15% and twice the period of no enrollment, and would exclude periods of COBRA, retiree, and VA coverage when determining the late enrollment penalty. In the 115th Congress, H.R. 2575 and S. 1909 would requirehave required Medicare to provide advance notification to those approaching Medicare eligibility, requirerequired the creation of a centralized enrollment webpage containing both Social Security and Medicare online tools, restructurerestructured Medicare enrollment periods and coverage periods, and expandexpanded the eligibility for special enrollment periods for those who meet exceptional conditions as defined by the Secretary of HHS. Also introduced in the 115th Congress, H.R. 2342 would requirehave required that employers notify employees about the availability of special enrollment periods to obtain marketplace coverage and Medicare coverage upon termination or separation, and H.R. 5104 would establishhave established a special Medicare Part B enrollment period for individuals enrolled in COBRA (Consolidated Omnibus Budget Reconciliation Act) continuation coverage who elected not to enroll in Part B during their initial enrollment period. Additionally, H.R. 707 would have, among other changes, eliminateeliminated late-enrollment penalties for those between the ages of 65 and 70.
As introduced in the 112th Congress, in addition to creating a special enrollment period for those with COBRA coverage, H.R. 1654 would have created a continuous enrollment period that would have allowed Medicare-eligible beneficiaries to sign up for Part B outside of the general enrollment period and to receive health coverage the following month. H.R. 1654 would have also expanded eligibility for equitable relief to those who based enrollment decisions on incorrect information provided by group health plans and plan sponsors, and it would have directed the Government Accountability Office to study problems with Part B enrollment. In the 111th Congress, H.R. 2235 would have limited the penalty for late Part B enrollment to 10% and limited the duration to twice the period of no enrollment, similar to the Part A late-enrollment penalty. It also would have excluded periods of COBRA and retiree coverage from the penalty.
Deficit Reduction Proposals
As Medicare currently represents about 14% of federal spending,151153 many proposals to reduce federal deficits include suggestions to reduce Medicare program spending and/or increase program income. For example, some proposals would increase Medicare premiums as a portion of total program funding, whereas others would limit the amount of federal contributions.
Increasing Medicare Premiums
Certain proposals suggest limiting premium increases to high-income beneficiaries. For example, the President's FY2017 budget proposal would have increased the percentage of per capita expenditures paid by high-income enrollees from 35% to 80% of expenditures to a range of between 40% and 90%, and it would have increased the number of high-income brackets from four to five.152154 The proposal also would have continued the freeze on income thresholds until 25% of beneficiaries were subject to the high-income premiums. (Subsequent to that proposal, the BBA 18 added a fifth high-income bracket with premiums set at 85% of per capita expenditures. See "Income-Related Premiums.")
Other proposals suggest increasing premiums paid by all Part B enrollees. For example, a proposal introduced in 2011 by then-Senators Lieberman and Coburn153155 suggested raising the standard Part B premium from the current 25% of program costs to 35% over five years.
Impose a Part B Premium Surcharge for Beneficiaries in Medigap Plans with Near First-Dollar Coverage
About 32In 2016, about 34% of beneficiaries enrolled in traditional Medicare buybought Medigap policies from private insurance companies that cover some or all of Medicare's cost sharing.154156 Individuals who purchase Medigap must pay a monthly premium, which is set by, and paid to, the insurance company selling the policy. There are 10 standardized Medigap plans with varying levels of coverage. Two of the 10 standardized plans cover Parts A and B deductibles and coinsurance in full (i.e., offer first-dollar coverage). In 2015, 65% of all beneficiaries who purchased Medigap insurance were covered by one of these two plans.155
Some are concerned that beneficiaries enrolled in Medigap plans with low cost-sharing requirements may have less incentive to consider the cost of health care services and may thus increase costs to the Medicare program. To address this, Section 401 of MACRA prohibits the sale of Medigap policies that cover Part B deductibles to newly eligible Medicare beneficiaries beginning in 2020. Some have also proposed imposing a Part B premium surcharge for Medicare beneficiaries who purchase certain types of Medigap plans. For example, the President's FY2016 budget proposal156158 suggested imposing a Part B premium surcharge of approximately 15% of the average Medigap premium (about 30% of the Part B premium) for new Medicare beneficiaries who enroll in a near first-dollar Medigap plan.
Limit Federal Subsidies
Finally, other proposals, such as that put forth in the FY2019 House Budget Resolution,157159 would place limits on the amount of the federal subsidy for Medicare, and premiums would vary depending on the Medicare plan in which the beneficiary enrolled. In general, such premium support proposals would limit federal spending by changing the current Medicare program from a defined-benefit to a defined-contribution system.158160 Most such proposals would limit the growth in the annual federal premium subsidy. Depending on how such a proposal is designed, and should Medicare costs grow more quickly than the limit, beneficiary premiums could increase more rapidly than the amount of the premium subsidy.
Considerations
Some of the issues that would need to be addressed when evaluating these types of deficit reduction proposals include (1) the ability of Medicare beneficiaries to absorb increased costs given their current levels of income and assets, as well as their other out-of-pocket expenditures (both health and non-health related); (2) the willingness of high-income beneficiaries to continue participating in Medicare Part B should their premiums be increased; and (3) the capacity of the Medicaid program to continue providing premium assistance to low-income beneficiaries should premiums increase.
Appendix A. History of the Part B Premium Statutory Policy and Legislative Authority
The basis for determining the Part B premium amount has changed several times since the inception of the Medicare program, reflecting different legislative views of what share beneficiaries should bear as expenditures have increased. When the Medicare program first went into effect in July 1966, the Part B monthly premium was set at a level to cover 50% of Part B program costs. Legislation enacted in 1972 limited the annual percentage increase in the premium to the same percentage by which Social Security benefits were adjusted for changes in the cost-of-living adjustments (i.e., COLAs). Under this formula, revenues from premiums soon dropped from 50% to below 25% of program costs because Part B program costs increased much faster than inflation as measured by the Consumer Price Index on which the Social Security COLA is based (see Table A-1).
From the early 1980s, Congress regularly voted to set Part B premiums at a level to cover 25% of program costs, in effect overriding the COLA limitation. The 25% provisions first became effective January 1, 1984, with general revenues covering the remaining 75% of Part B program costs. Premiums increased in 1989 as a result of the Medicare Catastrophic Coverage Act of 1988 (P.L. 100-360), which added a catastrophic coverage premium to the Part B premium. The act was repealed in November 1989, and the Part B premium for 1990 fell as a result.
Congress returned to the general approach of having premiums cover 25% of program costs in the Omnibus Budget Reconciliation Act of 1990 (OBRA 90; P.L. 101-508). However, OBRA 90 set specific dollar figures, rather than a percentage, in law for Part B premiums for the years 1991-1995. These dollar figures reflected Congressional Budget Office estimates of what 25% of program costs would be over the five-year period. However, program costs grew more slowly than anticipated, in part due to subsequent legislative changes. As a result, the 1995 premium of $46.10 actually represented 31.5% of Medicare Part B program costs.
The Omnibus Budget Reconciliation Act of 1993 (OBRA 93; P.L. 103-66) extended the policy of setting the Part B premium at a level to cover 25% of program costs for the years 1996-1998. As was the case prior to 1991, a percentage rather than a fixed dollar figure was used, which meant that the 1996 premium ($42.50) and the 1997 premium ($43.80) were lower than the 1995 premium ($46.10). The Balanced Budget Act of 1997 (BBA 97; P.L. 105-33) permanently set the premium at 25% of program costs so that, generally speaking, premiums rise or fall with Part B program costs.159
The Medicare Prescription Drug, Improvement, and Modernization Act of 2003 (MMA; P.L. 108-173), as modified by the Deficit Reduction Act of 2005 (DRA; P.L. 109-171), required that beginning in 2007, higher-income beneficiaries pay higher Part B premiums.160162 The income thresholds used to determine eligibility for the high-income premium are to be adjusted each year by the growth in the Consumer Price Index.161163 The Patient Protection and Affordable Care Act (ACA; P.L. 111-148, as amended, Section 3402), however, froze these thresholds for the period of 2011 through 2019 at the 2010 levels. In 2020, the thresholds were to return to the levels they would have been had they been adjusted for inflation each year during the freeze and again indexed to inflation each year. As this would have resulted in higher income thresholds, it would have had the effect of reducing the number of beneficiaries who pay the high-income premiums in 2020.
Section 402 of the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA; P.L. 114-10) maintains the freeze on the income thresholds for all income categories through 2017 and on the lower two high-income premium tiers through 2019. Beginning in 2018, MACRA reduces the threshold levels for the two highest income tiers so that more beneficiaries will fall into the higher percentage categories. (See "Income Thresholds.") Additionally, starting in 2020, the income thresholds for all income categories will be adjusted annually for inflation based on the 2019 income thresholds. This will, in effect, maintain the proportion of beneficiaries who pay the high-income premium.
Due to a 0% Social Security COLA coupled with an increase in Medicare premiums, a large percentage of Medicare Part B enrollees were protected by the hold-harmless provision in 2016 and continued to pay the 2015 premium of $104.90 per month. The Medicare trustees estimated that the standard premiums of those not held harmless in 2016 would therefore need to be increased to approximately $159 per month for aggregate premiums to still cover 25% of per capita benefit costs. The Bipartisan Budget Act of 2015 (BBA 15; P.L. 114-74), however, mitigated this sharp premium increase and required that the 2016 Part B standard premium be calculated as if the hold-harmless rule were not in effect and the increased costs had been spread across all beneficiaries. (See Appendix D.) Instead of having those not held harmless bear the increase for all of the Part B enrollee population, the act allowed for the transfer of additional general revenues to the SMI Trust Fund to make up for the shortfall in premium revenue. As a result of this change, Part B enrollees not held harmless paid a standard monthly premium of $121.80 in 2016. To offset the increased costs, a $3.00 surcharge was added to the monthly premium in 2016 (the $121.80 premium amount included this surcharge), and will continue to be applied in subsequent years until the additional federal cost of about $9 billion is fully offset (the surcharge increases on a sliding scale for those who pay high-income premiums, up to $9.60).
BBA 15 provided for similar premium adjustments in 2017 if there were a 0% Social Security COLA again in that year. However, as there was a 0.3% 2017 Social Security COLA, this provision was not applicable in 2017.
Section 53114 of the Bipartisan Budget Act of 2018 (BBA 18; P.L. 115-123) addsadded an additional high-income category beginning in 2019 for individuals with annual incomes of $500,000 or more or couples filing jointly with incomes of $750,000 or more. Enrollees with income equal to or exceeding these thresholds will pay premiums that cover 85% of the average per capita cost of Part B benefits instead of 80%. The threshold for couples filing jointly in this new income tier will beis calculated as 150% of the individual income level rather than 200% as in the other income tiers. The BBA 15 premium surcharge for this category will beis $10.20. This new top income threshold will be frozen through 2027 and will be adjusted annually for inflation starting in 2028 based on the CPI-U.
|
Monthly Premium |
Effective Date |
Governing Policy; Legislative Authority |
||||
|
1966 |
$3.00 |
7/1966 |
Fixed dollar amount; Social Security Amendments (SSA) of 1965 |
|||
|
1967 |
$3.00 |
Fixed dollar amount; SSA of 1965 |
||||
|
1968 |
$4.00 |
4/1968 |
Fixed dollar amount through March; Medicare Enrollment Act of 1967. Beginning April: 50% of costs; SSA of 1965 |
|||
|
1969 |
$4.00 |
50% of costs; SSA of 1967 |
||||
|
1970 |
$5.30 |
7/1970 |
50% of costs; SSA of 1967 |
|||
|
1971 |
$5.60 |
7/1971 |
50% of costs; SSA of 1967 |
|||
|
1972 |
$5.80 |
7/1972 |
50% of costs; SSA of 1967 |
|||
|
1973 |
$6.30 |
9/1973 |
50% of costs; SSA of 1967 (cost-of-living adjustment [COLA] limit, added by SSA of 1972, could have applied, but was not needed). Limitations imposed by Economic Stabilization program set 7/1973 amount at $5.80 and 8/73 amount at $6.10. |
|||
|
1974 |
$6.70 |
7/1974 |
50% of costs; SSA of 1967 (COLA limit, added by SSA of 1972, could have applied, but was not needed) |
|||
|
1975 |
$6.70 |
Technical error in law prevented updating |
||||
|
1976 |
$7.20 |
7/1976 |
COLA limit; SSA of 1972 |
|||
|
1977 |
$7.70 |
7/1977 |
COLA limit; SSA of 1972 |
|||
|
1978 |
$8.20 |
7/1978 |
COLA limit; SSA of 1972 |
|||
|
1979 |
$8.70 |
7/1979 |
COLA limit; SSA of 1972 |
|||
|
1980 |
$9.60 |
7/1980 |
COLA limit; SSA of 1972 |
|||
|
1981 |
$11.00 |
7/1981 |
COLA limit; SSA of 1972 |
|||
|
1982 |
$12.20 |
7/1982 |
COLA limit; SSA of 1972 |
|||
|
1983 |
$12.20 |
Tax Equity and Fiscal Responsibility Act of 1982 (TEFRA) had set 25% rule for updates in 7/1983 and 7/1984. However, SSA of 1983 froze premiums 7/1983-12/1983 and changed future updates to January. |
||||
|
1984 |
$14.60 |
1/1984 |
25% of costs; TEFRA, as amended by SSA of 1983 |
|||
|
1985 |
$15.50 |
1/1985 |
25% of costs; TEFRA, as amended by SSA of 1983 |
|||
|
1986 |
$15.50 |
1/1986 |
25% of costs; Deficit Reduction Act (DEFRA) of 1984 |
|||
|
1987 |
$17.90 |
1/1987 |
25% of costs; DEFRA of 1984 |
|||
|
1988 |
$24.80 |
1/1988 |
25% of costs, Consolidated Omnibus Budget Reconciliation Act (OBRA) of 1985 |
|||
|
1989 |
$31.90 |
1/1989 |
25% of costs, OBRA 87, plus $4 catastrophic coverage premium added by Medicare Catastrophic Coverage Act of 1988 |
|||
|
1990 |
$28.60 |
1/1990 |
25% of costs; OBRA 89. Medicare Catastrophic Coverage Repeal Act of 1989 repealed additional catastrophic coverage premium, effective 1/90 |
|||
|
1991 |
$29.90 |
1/1991 |
Fixed dollar amount; OBRA 90 |
|||
|
1992 |
$31.80 |
1/1992 |
Fixed dollar amount; OBRA 90 |
|||
|
1993 |
$36.60 |
1/1993 |
Fixed dollar amount; OBRA 90 |
|||
|
1994 |
$41.10 |
1/1994 |
Fixed dollar amount; OBRA 90 |
|||
|
1995 |
$46.10 |
1/1995 |
Fixed dollar amount; OBRA 90 |
|||
|
1996 |
$42.50 |
1/1996 |
25% of costs; OBRA 93 |
|||
|
1997 |
$43.80 |
1/1997 |
25% of costs; OBRA 93 |
|||
|
1998 |
$43.80 |
1/1998 |
25% of costs; OBRA 93 and Balanced Budget Act (BBA) 97 |
|||
|
1999 |
$45.50 |
1/1999 |
25% of costs; BBA 97 |
|||
|
2000 |
$45.50 |
1/2000 |
25% of costs; BBA 97 |
|||
|
2001 |
$50.00 |
1/2001 |
25% of costs; BBA 97 |
|||
|
2002 |
$54.00 |
1/2002 |
25% of costs; BBA 97 |
|||
|
2003 |
$58.70 |
1/2003 |
25% of costs; BBA 97 |
|||
|
2004 |
$66.60 |
1/2004 |
25% of costs; BBA 97 |
|||
|
2005 |
$78.20 |
1/2005 |
25% of costs; BBA 97 |
|||
|
2006 |
$88.50 |
1/2006 |
25% of costs; BBA 97 |
|||
|
2007 |
$93.50 |
1/2007 |
25% of costs; BBA 97 (Medicare Modernization Act of 2003 [MMA] and Deficit Reduction Act of 2005 [DRA] authorize higher premiums for high-income enrollees: 1st year of 3-year phase-in) |
|||
|
2008 |
$96.40 |
1/2008 |
25% of costs; BBA 97 (MMA and DRA authorize higher premiums for high-income enrollees: 2nd year of 3-year phase-in) |
|||
|
2009 |
$96.40 |
1/2009 |
25% of costs; BBA 97 (MMA and DRA authorize higher premiums for high-income enrollees: 3rd year of 3-year phase-in) |
|||
|
2010 |
$110.50 |
1/2010 |
25% of costs; BBA 97 (MMA and DRA authorize higher premiums for high-income enrollees, fully phased-in); hold-harmless provision applied to most enrollees who paid the 2009 rate of $96.40 |
|||
|
2011 |
$115.40 |
1/2011 |
25% of costs; BBA 97 (MMA and DRA authorize higher premiums for high-income enrollees |
|||
|
2012 |
$99.90 |
1/2012 |
25% of costs; BBA 97 (MMA and DRA authorize higher premiums for high-income enrollees |
|||
|
2013 |
$104.90 |
1/2013 |
25% of costs; BBA 97 (MMA and DRA authorize higher premiums for high-income enrollees |
|||
|
2014 |
$104.90 |
1/2014 |
25% of costs; BBA 97 (MMA and DRA authorize higher premiums for high-income enrollees |
|||
|
2015 |
$104.90 |
1/2015 |
25% of costs; BBA 97 (MMA and DRA authorize higher premiums for high-income enrollees |
|||
|
2016 |
$121.80 |
1/2016 |
Less than 25% of costs; BBA 97 and BBA 15 (MMA and DRA authorize higher premiums for high-income enrollees |
|||
|
2017 |
$134.00 |
1/2017 |
25% of costs plus $3.00 BBA 15 surcharge; BBA 97 and BBA 15 (MMA and DRA authorize higher premiums and surcharges for high-income enrollees |
|||
|
2018 |
$134.00 |
1/2018 |
25% of costs plus $3.00 BBA 15 surcharge; BBA 97 and BBA 15 (MMA and DRA authorize higher premiums and surcharges for high-income enrollees 2019 $135.50 1/2019 |
Sources: Various annual Medicare Trustees reports and CMS, "Medicare Program: Medicare Part B Monthly Actuarial Rates, Premium Rate, and Annual Deductible Beginning January 1, 2018," 822019," 83 Federal Register 55370, November 21, 201752462, October 17, 2018, at https://www.gpo.gov/fdsys/pkg/FR-2017-11-21/pdf/2017-24877FR-2018-10-17/pdf/2018-22530.pdf.
Appendix B.
Standard and High-Income Part B Premiums and Income Thresholds: 2007-2018
Table B-1. Income Levels for Determining Part B Premium Adjustment and Per Person Premium Amounts, 2007-20182019
(in nominal dollars)
|
2007 |
2008 |
2009 |
2010 |
2011 |
2012 |
2013-2015 |
2016 |
2017 |
2018 |
2019 |
|||||||||||||
|
Standard Premium |
Less than or equal to $80,000 Less than or equal to $160,000 $93.50 |
Less than or equal to $82,000 Less than or equal to $164,000 $96.40 |
Less than or equal to $85,000 Less than or equal to $170,000 $96.40a |
Less than or equal to $85,000 Less than or equal to $170,000 $110.50b |
Less than or equal to $85,000 Less than or equal to $170,000 $115.40b |
Less than or equal to $85,000 Less than or equal to $170,000 $99.90 |
Less than or equal to $85,000 Less than or equal to $170,000 $104.90 |
Less than or equal to $85,000 Less than or equal to $170,000 $121.80b |
Less than or equal to $85,000 Less than or equal to $170,000 $134.00b |
Less than or equal to $85,000 Less than or equal to $170,000 $134.00b |
Less than or equal to $85,000individual
Less than or equal to $170,000couple
$135.50b
|||||||||||||
|
Level 1 |
$80,001-$100,000 individual $160,001-$200,000 $105.80 |
$82,001-$102,000 individual $164,001-$204,000 $122.20 |
$85,001-$107,000 individual $170,001-$214,000 $134.90 |
$85,001-$107,000 individual $170,001-$214,000 $154.70 |
$85,001-$107,000 individual $170,001-$214,000 $161.50 |
$85,001-$107,000 individual $170,001-$214,000 $139.90 |
$85,001-$107,000 individual $170,001-$214,000 $146.90 |
$85,001-$107,000 individual $170,001-$214,000 $170.50 |
$85,001-$107,000 individual $170,001-$214,000 $187.50 |
$85,001-$107,000 individual $170,001-$214,000 $187.50 |
|||||||||||||
|
Level 2 |
$100,001-$150,000 individual $200,001-$300,000 couple $124.40 |
$102,001-$153,000 individual $204,001-$306,000 couple $160.90 |
$107,001-$160,000 individual $214,001-$320,000 couple $192.70 |
$107,001-$160,000 individual $214,001-$320,000 couple $221.00 |
$107,001-$160,000 individual $214,001-$320,000 couple $230.70 |
$107,001-$160,000 individual $214,001-$320,000 couple $199.80 |
$107,001-$160,000 individual $214,001-$320,000 couple $209.80 |
$107,001-$160,000 individual $214,001-$320,000 couple $243.60 |
$107,001-$160,000 individual $214,001-$320,000 couple $267.90 |
$107,001-$133,500 individual $214,001-$267,000 couple $267.90 |
$107,001-$133,500 individual $214,001-$267,000 couple $270.90 |
||||||||||||
|
Level 3 |
$150,001-$200,000 individual $300,001-$400,000 couple $142.90 |
$153,001-$205,000 individual $306,001-$410,000 couple $199.70 |
$160,001-$213,000 individual $320,001-$426,000 couple $250.50 |
$160,001-$214,000 individual $320,001-$428,000 couple $287.30 |
$160,001-$214,000 individual $320,001-$428,000 couple $299.90 |
$160,001-$214,000 individual $320,001-$428,000 couple $259.70 |
$160,001-$214,000 individual $320,001-$428,000 couple $272.70 |
$160,001-$214,000 individual $320,001-$428,000 couple $316.70 |
$160,001-$214,000 individual $320,001-$428,000 couple $348.30 |
$133,501-$160,000 individual $267,001-$320,000 couple $348.30 $133,501-$160,000 individual $267,001-$320,000 couple $352.20 |
|||||||||||||
|
Level 4 |
$200,000+ individual $400,000+ couple $161.40 |
$205,000+ individual $410,000+ couple $238.40 |
$213,000+ individual $426,000+ couple $308.30 |
$214,000+ individual $428,000+ couple $353.60 |
$214,000+ individual $428,000+ couple $369.10 |
$214,000+ individual $428,000+ couple $319.70 |
$214,000+ individual $428,000+ couple $335.70 |
$214,000+ individual $428,000+ couple $389.80 |
$214,000+ individual $428,000+ couple $428.60 |
$160,000+ individual $320,000+ couple $428.60 |
$160,001- $499,999 individual $320,001- $749,999 couple $433.40 |
Level 5 |
n/a |
n/a |
n/a |
n/a |
n/a |
n/a |
n/a |
n/a |
n/a |
n/a |
$500,000 or more individual $750,000 or more couple $460.50 |
Sources: CMS, Annual Notices, "Medicare Program; Medicare Part B Monthly Actuarial Rates, Premium Rate, and Annual Deductible," 2007 through 20172018, and CMS, "Medicare Program: Medicare Part B Monthly Actuarial Rates, Premium Rate, and Annual Deductible Beginning January 1, 2018," 822019," 83 Federal Register 55370, November 21, 201752462, October 17, 2018.
Note: n/a = not applicable. When both are enrolled in Part B, each person in a couple pays the same individual premium amount.
a. The standard Part B premium in 2009 was the same as that in 2008; however, the lack of change was not due to the hold-harmless provision. CMS determined that 2008 premiums and revenues were slightly higher than needed to cover costs in that year and that 2009 financing would be adequate at the same premium level.
b. Due to no Social Security COLA in 2010 and 2011, most Part B enrollees were held harmless and paid the 2009 standard monthly premium of $96.40. Similarly, in 2016, those who were held harmless paid the 2015 premium of $104.90 per month, and those who were held harmless in 2017 paid, on average, $109.00 per month. In 2018, about 28% of enrollees arewere protected under the hold -harmless provision and paypaid premiums of less than $134.00 per month.
Table B-2. Income Levels for Determining Part B Premium Adjustment for Married Beneficiaries Filing Separately and Associated Premiums, 2007-2018
(in nominal dollars)
|
Income Level |
2007 |
2008 |
2009 |
2010 |
2011 |
2012 |
2013-2015 |
2016 |
2017 |
2018 |
2019 |
|
Standard |
Less than or equal to $80,000 $93.50 |
Less than or equal to $82,000 $96.40 |
Less than or equal to $85,000 $96.40 |
Less than or equal to $85,000 $110.50 |
Less than or equal to $85,000 $115.40 |
Less than or equal to $85,000 $99.90 |
Less than or equal to $85,000 $104.90 |
Less than or equal to $85,000 $121.80 |
Less than or equal to $85,000 $134.00 |
Less than or equal to $85,000 $134.00 |
Less than or equal to $85,000 $135.50 |
|
Lower Adjustment Category |
Greater than $80,000 and less than or equal to $120,000 $142.90 |
Greater than $82,000 and less than or equal to $123,000 $199.70 |
Greater than $85,000 and less than or equal to $128,000 $250.50 |
Greater than $85,000 and less than or equal to $129,000 $287.30 |
Greater than $85,000 and less than or equal to $129,000 $299.90 |
Greater than $85,000 and less than or equal to $129,000 $259.70 |
Greater than $85,000 and less than or equal to $129,000 $272.70 |
Greater than $85,000 and less than or equal to $129,000 $316.70 |
Greater than $85,000 and less than or equal to $129,000 $348.30 |
Not applicable |
Greater than $85,000 and less than $415,000 $433.40 |
|
Higher Adjustment Category |
Greater than $120,000 $161.40 |
Greater than $123,000 $238.40 |
Greater than $128,000 $308.30 |
Greater than $129,000 $353.60 |
Greater than $129,000 $369.10 |
Greater than $129,000 $319.70 |
Greater than $129,000 $335.70 |
Greater than $129,000 $389.80 |
Greater than $129,000 $428.60 |
Greater than $85,000 $428.60 |
Greater than or equal to $415,000 $460.50 |
Sources: CMS, Annual Notices, "Medicare Program; Medicare Part B Monthly Actuarial Rates, Premium Rate, and Annual Deductible," 2007 through 20172018, and CMS, "Medicare Program: Medicare Part B Monthly Actuarial Rates, Premium Rate, and Annual Deductible Beginning January 1, 2018," 812019," 83 Federal Register 55370, November 21, 201752462, October 17, 2018.
Appendix C. Estimated Future Part B Premiums
|
Percentage of Program Costs Represented by Premium |
|||||||||||
|
25% (Standard) |
35% |
50% |
65% |
80% |
85%a |
||||||
|
Actual |
|||||||||||
|
2017 |
$134.00 |
$187.50 |
$267.90 |
$348.30 |
$428.60 |
— |
|||||
|
2018 |
134.00 |
187.50 |
267.90 |
348.30 |
428.60 |
— |
|||||
|
Projected
|
135.50
|
189.60
|
270.90
|
352.20
|
433.40 $460.50 | ||||||
|
2019 |
135.50 |
189.70 |
271.00 |
352.30 |
433.60 |
$460.70 |
|||||
|
2020 |
141.10 |
197.50 |
282.20 |
366.90 |
451.50 |
479.70 |
|||||
|
2021 |
148.50 |
207.90 |
296.90 |
386.00 |
475.00 |
504.80 |
|||||
|
2022 |
154.50 |
216.20 |
308.90 |
401.60 |
494.20 |
525.10 |
|||||
|
2023 |
163.30 |
228.60 |
326.60 |
424.60 |
522.60 |
555.20 |
|||||
|
2024 |
173.20 |
242.40 |
346.30 |
450.20 |
554.10 |
588.70 |
|||||
|
2025 |
182.50 |
255.50 |
365.00 |
474.50 |
584.00 |
620.50 |
|||||
|
2026 |
191.00 |
267.30 |
381.90 |
496.50 |
611.00 |
649.20 |
|||||
|
2027 |
202.70 |
283.80 |
405.40 |
527.00 |
648.60 |
689.20 |
|||||
Sources: 2018 Medicare Trustees Report, Tables V.E2 and V.E3.
Notes: These figures, and CMS, "Medicare Program: Medicare Part B Monthly Actuarial Rates, Premium Rate, and Annual Deductible Beginning January 1, 2019," 83 Federal Register 52462, October 17, 2018.
Notes: The figures beyond 2019 only represent estimates of future premiums. Actual premiums are determined each year in the fall prior to the actual year the premium will be in effect.
a. Starting in 2019, theThe Bipartisan Budget Act of 2018 (BBA 18; P.L. 115-123) addsadded an additional income tier with premiums set at 85% of per capita program costs starting in 2019.
Appendix D. Bipartisan Budget Act of 2015 Changes to 2016 Part B Premiums
Under normal circumstances, standard Medicare Part B premiums are set at an amount to cover 25% of projected average per capita Part B expenditures plus an appropriate contingency margin. Due to expected growth in the cost of Part B benefits, the Medicare trustees projected that in order to cover 25% of benefit costs as well as to build up adequate contingency reserves, the 2016 Part B premiums would need to be increased to about $121 per month from the 2015 amount of $104.90.162164 However, due to the absence of a Social Security COLA in 2016 and the resulting widespread application of the hold-harmless provision, most Part B enrollees continued to pay the 2015 premium amount of $104.90 through 2016. With about 70% of enrollees continuing to pay $104.90, the only way that premiums could cover 25% of per capita expenditures would have been if those not held harmless (the remaining 30%) bore the entire cost increase (i.e., if the aggregate increase in premiums were spread out over fewer people). The Medicare trustees estimated that the premiums of those not held harmless would therefore need to be increased to about $159 per month.163165 The trustees also estimated that high-income beneficiaries (i.e., those earning more than $85,000) would need to pay significantly higher monthly premiums of about $223, $319, $414, or $510 depending on their level of income (compared to their respective 2015 premiums of $147, $210, $273, and $336 per month).
To mitigate the expected large premium increases for those not held harmless, the Bipartisan Budget Act of 2015 (BBA 15; P.L. 114-74) required that 2016 Medicare Part B premiums be set as if the hold-harmless rule were not in effect—in other words, to calculate premiums as if all enrollees were paying the same annual inflation-adjusted standard premium (about $121 per month). To compensate for the lost premium revenue (below the required 25%) and to ensure that the Supplementary Medical Insurance (SMI) Trust Fund had adequate income to cover payments for Part B benefits in 2016, the act allowed for additional transfers from the General Fund of the Treasury to the SMI Trust Fund.
To offset the approximately $9 billion in increased federal spending in 2016 resulting from the reduction in standard premiums for those not held harmless (i.e., the additional amounts transferred from the General Fund), as well as the loss of income due to reductions in the income-related monthly adjustment for high-income enrollees, the law required that a $3.00 per month surcharge be added to standard premiums in 2016, and each subsequent year, until the $9 billion is fully offset.164166 (For those who pay high-income premiums, the surcharge increases on a sliding scale, up to $9.60.) It is expected that this surcharge will be applied to premiums through 2021.165167 The monthly repayment surcharge is paid only by those not held harmless.
Should there have been a 0% Social Security COLA in 2017, BBA 15 allowed for a similar Medicare Part B premium setting mechanism for 2017. However, as there was a 0.3% COLA in 2017, this provision did not apply. BBA 15 did not allow for similar adjustments beyond 2017.
The vast majority of persons turning the age of 65 are automatically entitled to Medicare Part A based on their own or their spouse's work in covered employment. However, individuals aged 65 and older who are not otherwise eligible for Medicare Part A benefits and certain disabled individuals who have exhausted other entitlement may voluntarily purchase Part A coverage.166168 In most cases, persons who voluntarily purchase Part A must also purchase Part B. The periods during which one can enroll are the same as those for Part B (see "Medicare Part B Eligibility and Enrollment").
The monthly Part A premium is equal to the full average per capita value of the Part A benefit ($422437.00 per month in 20182019). Persons who have at least 30 quarters of covered employment (or are married to someone who has such coverage) pay a premium that is 45% less than the full Part A premium ($232240.00 per month in 2018).1672019).169 CMS estimates that in 20182019, about 668679,000 individuals will voluntarily enroll in Part A by paying the full premium and about 7175,000 will pay the reduced premium.168170
Similar to Part B, a penalty is imposed for persons who delay Part A enrollment beyond their initial enrollment period (which is the same seven-month period applicable for enrollment in Part B).169171 However, both the amount of the penalty and the duration of the penalty are different than under Part B. Persons who delay Part A enrollment for at least 12 months beyond their initial enrollment period are subject to a 10% premium surcharge.170172 The surcharge is 10% regardless of the length of the delay. Further the surcharge only applies for a period equal to twice the number of years (i.e., 12-month periods) during which an individual delays enrollment. Thus, an individual who delays enrollment for three years under Part A would be subject to a 10% penalty for six years, whereas a person who delays enrollment for the same three-year period under Part B would be subject to a permanent 30% penalty.171
Author Contact Information
Footnotes
| 1. |
Expenditure estimates from Boards of Trustees, Federal Hospital Insurance and Federal Supplementary Medical Insurance Trust Funds, 2018 Annual Report of the Boards of Trustees of the Federal Hospital Insurance and Federal Supplementary Medical Insurance Trust Funds, June 5, 2018, at https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/ReportsTrustFunds/index.html. (Hereinafter, 2018 Medicare Trustees Report.) |
|||
| 2. |
For additional information on the Medicare program, see CRS Report R40425, Medicare Primer. |
|||
| 3. |
See CRS Report R43122, Medicare Financial Status: In Brief. |
|||
| 4. |
See Internal Revenue Service, Questions and Answers for the Additional Medicare Tax, at http://www.irs.gov/Businesses/Small-Businesses-&-Self-Employed/Questions-and-Answers-for-the-Additional-Medicare-Tax. |
|||
| 5. |
All expenditure data are from the 2018 Medicare Trustees Report. |
|||
| 6. |
For additional information on this fee, see CRS Report R41128, Health-Related Revenue Provisions in the Patient Protection and Affordable Care Act (ACA). |
|||
| 7. |
In |
|||
| 8. |
Depending on their income |
|||
| 9. | ||||
| 10. |
Centers for Medicare & Medicaid Services (CMS), " |
|||
| 11. |
CMS, "Medicare Program: Medicare Part B Monthly Actuarial Rates, Premium Rate, and Annual Deductible Beginning January 1, |
|||
| 12. |
SSA §1839(f). The premiums of those held harmless vary depending on the dollar amount of the increase in their Social Security benefits. To be held harmless in a given year, a beneficiary must have received Social Security benefit checks in both December of the previous year and January of the current year, and also must have had Medicare Part B premiums deducted from both checks. The hold-harmless provision applies to that person if the net Social Security benefit for January of the current year is lower than in December of the previous year. | |||
| 13. | See "Protection of Social Security Benefits from Increases in Medicare Part B Premiums." |
|||
|
Annual increases in the deductibles are not protected by the hold-harmless provision. |
||||
|
For additional information on Part A premiums, see Appendix E. |
||||
|
For additional information on enrolling in Medicare Parts A and B, see Medicare publication "Enrolling in Medicare Part A & Part B," at https://www.medicare.gov/Pubs/pdf/11036-Enrolling-Medicare-Part-A-Part-B.pdf. |
||||
|
See "Welcome to Medicare" publication at https://www.medicare.gov/Pubs/pdf/11095-Welcome-to-Medicare.pdf. When first becoming eligible for Medicare, beneficiaries need to make a number of choices regarding the benefits they wish to sign up for and how they wish to receive them. For example, new enrollees need to decide whether they wish to remain in traditional Medicare (Parts A and B, the default option) or if they would like to receive their A and B benefits through a private Medicare Advantage Plan (Part C). Additionally, beneficiaries need to decide whether they would like to sign up for an outpatient prescription drug plan (Part D). These options are described in the "Welcome to Medicare" package. For free personalized health insurance counseling, beneficiaries may contact their local State Health Insurance Assistance Programs (SHIPs); contact information may be found at http://www.medicare.gov/contacts/ and https://shipnpr.acl.gov/shipprofile.aspx. |
||||
|
Those who live in Puerto Rico are not automatically enrolled in Medicare Part B. They need to sign up for Part B during the initial enrollment period or possibly be subject to a penalty. See CRS Report R44275, Puerto Rico and Health Care Finance: Frequently Asked Questions, and Social Security Administration Publication "Medicare in Puerto Rico," at http://www.socialsecurity.gov/pubs/EN-05-10521.pdf. The following bills, introduced in the 115th Congress, would |
||||
|
Should a beneficiary decline Part B coverage, a new Medicare card will be issued that indicates that the beneficiary has Part A coverage only. |
||||
|
Individuals with Amyotrophic Lateral Sclerosis are not subject to the 24-month waiting period; for these individuals Medicare coverage begins the first day of the month during which disability benefits start. Additionally, the Medicare coverage period for persons diagnosed with end-stage renal disease generally begins in the third month after the month when dialysis begins. |
||||
|
For additional information, see CMS, "Employer Community: Information about Medicare Enrollment," at https://www.cms.gov/Outreach-and-Education/Find-Your-Provider-Type/Employers-and-Unions/Employer-community.html. |
||||
|
In the past, individuals generally were eligible to receive both full Social Security retirement benefits and Medicare coverage starting at the age of 65. However, the age to receive full retirement benefits has changed for some people, depending on the year they were born. For example, those turning 65 in |
||||
|
To apply, individuals can call or visit their local Social Security office or call Social Security at 1-800-772-1213. Some people also may apply online if they meet certain rules, at https://www.ssa.gov/medicare/. For Railroad Retirement Board (RRB) retirees, application information may be found at https://www.rrb.gov/Benefits/Medicare. See also Social Security Administration, "Apply Online For Medicare In Less Than 10 Minutes—Even If You Are Not Ready To Retire," at http://www.socialsecurity.gov/pubs/EN-05-10530.pdf, and Social Security Administration, "How to Apply Online for Medicare Only," at http://www.socialsecurity.gov/pubs/EN-05-10531.pdf. |
||||
|
An eligibility, enrollment date, and premium calculator may be found on the Medicare.gov website at https://www.medicare.gov/eligibilitypremiumcalc/. |
||||
|
For additional information on eligibility for the disabled under the age of 65, see CRS Report RS22195, Social Security Disability Insurance (SSDI) and Medicare: The 24-Month Waiting Period for SSDI Beneficiaries Under Age 65. |
||||
|
The Part B general enrollment period is different from the Medicare Advantage and Part D annual enrollment period which runs from October 15 to December 7 each year, with coverage effective the following January. |
||||
|
For more information, see Medicare.gov "Part B Late Enrollment Penalty," at |
||||
|
Figures provided by CMS, |
||||
|
The state pays the standard premium regardless of the date the beneficiary first became eligible for Medicare Part B. See Social Security Administration, Program Operations Manual, Section HI 00815.001, "State Buy-In Program General Description," at https://secure.ssa.gov/apps10/poms.nsf/lnx/0600815001; and Ibid., Section HI 00815.039, "Effect of Buy-In on the Individual," at https://secure.ssa.gov/apps10/poms.nsf/lnx/0600815039. |
||||
|
Social Security Act (SSA) §1839(b). |
||||
|
Specifically, adverse selection occurs when beneficiaries, who generally have more information than insurers about their own health status and expected health care needs, make insurance purchasing decisions based on their expected use of the insurance benefit. Their decision to purchase insurance is based on a comparison of the value of the insurance coverage, given their expected use, and the cost of the insurance. Should only (or disproportionately) persons who are high health care users enroll in the program, per capita costs would increase, thereby making the health insurance purchase decision less attractive for healthier, and presumably less costly, beneficiaries who then, in turn, might drop out of the program. Subsequent iterations of this cycle would drive premium costs higher and higher for a smaller and smaller subset of ever sicker and costlier beneficiaries. |
||||
|
By comparison, to be eligible for the outpatient prescription drug benefit under Part D, a Medicare beneficiary must reside in a geographic area where a Part D plan is available. Individuals who are incarcerated or who live outside the United States are therefore not eligible to enroll in (or continue enrollment in) Part D. Because the Part D penalty is based on periods when one is eligible but not enrolled, periods of incarceration or extended residence outside of the United States would not be included in that calculation. For example, an individual living outside of the country during his or her initial enrollment period would be given a special enrollment period (SEP) upon returning to the United States and would be able to sign up for Part D at that time without penalty. See Social Security Administration, Program Operations Manual, Section HI 03001.001, "Description of the Medicare Part D Prescription Drug Program," at https://secure.ssa.gov/poms.nsf/lnx/0603001001, and CMS Publication, "Understanding Medicare Part C & D Enrollment Periods," at https://www.medicare.gov/Pubs/pdf/11219-Understanding-Medicare-Part-C-D.pdf. |
||||
|
Under Part D, individuals who have maintained drug coverage equivalent to Medicare's standard prescription drug coverage prior to enrolling in Part D are not subject to a late-enrollment penalty. Examples of "creditable" Part D drug coverage include drug coverage from a former employer or union, TRICARE, the Department of Veterans Affairs (VA), the Federal Employees Health Benefits Program (FEHBP), or the Indian Health Service. As an illustration, if an individual did not sign up for Part D when first becoming eligible because he or she already had equivalent coverage through a former employer, the individual could sign up for Part D at any time without penalty during the time he or she maintained creditable coverage. Should that coverage end, the individual would be entitled to a special enrollment period and could enroll in Part D without penalty. Beneficiaries who have a break in creditable prescription drug coverage usually have 63 consecutive days to enroll in Part D during |
||||
|
SSA §1839(b). |
||||
|
Social Security Administration, Program Operations Manual, Section HI 01001.010, "Premium Increase for Late Enrollment," at https://secure.ssa.gov/poms.nsf/lnx/0601001010. |
||||
|
Those who pay the high-income premiums are not protected by the hold-harmless provision. For additional information, see Social Security Administration, Programs Operation Manual, Section HI 01101.031, "How IRMAA is Calculated and How IRMAA Affects the Total Medicare Premium," at https://secure.ssa.gov/apps10/poms.nsf/lnx/0601101031. |
||||
|
|
||||
|
SSA §1837(i) and 42 C.F.R. §407.20. See Medicare Publication "Medicare and Other Health Benefits: Your Guide to Who Pays First," https://www.medicare.gov/Pubs/pdf/02179-Medicare-Coordination-Benefits-Payer.pdf, and CMS, "Medicare Secondary Payer," at https://www.cms.gov/Medicare/Coordination-of-Benefits-and-Recovery/Coordination-of-Benefits-and-Recovery-Overview/Medicare-Secondary-Payer/Medicare-Secondary-Payer.html. Also see CRS Report RL33587, Medicare Secondary Payer: Coordination of Benefits. |
||||
|
The requirement that large employers' coverage pays primary for Medicare-eligible employees was created by the Tax Equity and Fiscal Responsibility Act of 1982 (P.L. 97-248) and amended by the Consolidated Omnibus Budget Reconciliation Act of 1985 (P.L. 99-272). |
||||
|
For Medicare-eligible beneficiaries employed by organizations with fewer than 20 employees (or fewer than 100 employees for the disabled), Medicare generally pays primary and the employer group health plan generally pays secondary. In such cases, employers may offer coverage that wraps around the Medicare benefit and beneficiaries may need to enroll in Medicare Part B when first eligible to avoid potential late-enrollment penalties and/or gaps in coverage. Individuals who are turning 65 and still working should check with their employers' benefit administrator to learn how their employer health coverage works with Medicare. |
||||
|
See "Special Enrollment Period" section of Social Security webpage: Social Security Administration, "Retirement Planner: Applying for Medicare Only," at https://www.ssa.gov/planners/retire/justmedicare.html. |
||||
|
The Balanced Budget Act of 1997 (BBA; P.L. 105-33) added this exception to the penalty. This exception is for disabled persons (a) who, at the time they first become eligible for Part B, are enrolled in a group health plan (regardless of size) by virtue of their current or former employment and (b) whose continuous enrollment under the plan is involuntarily terminated at a time when their enrollment in the plan is by virtue of their or their spouse's former (i.e., not current) employment. These individuals have a special six-month enrollment period beginning on the first day of the month in which the termination occurs. |
||||
|
For a description of COBRA, see Department of Labor, "COBRA Continuation Coverage," at https://www.dol.gov/agencies/ebsa/laws-and-regulations/laws/cobra. |
||||
|
SSA §1837(k) and 42 C.F.R. §407.21. |
||||
|
SSA §1837(h) and 42 C.F.R. §407.32. |
||||
|
For additional information, see Social Security Administration, Program Operations Manual, Section HI 00805.170, "Conditions for Providing Equitable Relief," at https://secure.ssa.gov/poms.nsf/lnx/0600805170, and Ibid, Section HI 00805.175, "Evidence of Government Error or Delay," at https://secure.ssa.gov/poms.nsf/lnx/0600805175. |
||||
|
See SSA Emergency Message, "Medicare Enrollment for |
||||
|
CMS indicates that in this instance, the individual should contact the marketplace at least 15 days before the date one wants the coverage to end. |
||||
|
CMS Factsheet, "Assistance for Individuals with Medicare Part A and Exchange Coverage Information for SHIPs and Exchange Assisters," undated, https://www.cms.gov/Medicare/Eligibility-and-Enrollment/Medicare-and-the-Marketplace/Downloads/SHIP-and-Navigators-Fact-Sheet- |
||||
|
Individuals who pay a premium for Medicare Part A are not eligible for this equitable relief, as they are required to enroll in Part B in order to enroll in Part A. Those enrolled in a Marketplace Small Business Health Options Program (SHOP) plan are also not eligible for this equitable relief, as such plans are considered employer sponsored plans and, as described earlier, these individuals already qualify for a special enrollment period once that coverage ends. |
||||
|
Individuals may contact SSA at 1-800-772-1212 or visit their local Social Security Office. Part B coverage will generally begin the month the individual enrolls. Once they are enrolled in Part B, they will have a two month special enrollment period to enroll in Medicare Advantage and/or Part D. |
||||
|
Ibid., Section HI 01001.020, "Collection of Premiums," at https://secure.ssa.gov/poms.nsf/lnx/0601001020. |
||||
|
SSA §1840(a)(1) and §1840(b)(1). See CRS Report R42035, Social Security Primer, and CRS Report RS22350, Railroad Retirement Board: Retirement, Survivor, Disability, Unemployment, and Sickness Benefits. |
||||
|
See CRS Report 98-810, Federal Employees' Retirement System: Benefits and Financing. |
||||
|
42 C.F.R. §408.60. |
||||
|
SSA §1840(a)(1). |
||||
|
Beneficiaries who receive their Parts A and B benefits through Medicare Advantage (MA, Part C), must still pay the monthly Part B premium, but may pay different amounts. For example, some MA plans may offer an additional benefit by reducing the amount one pays for the Part B premium. Alternatively, some MA plans may be more expensive than traditional Medicare, for example because they provide benefits beyond what is provided under traditional Medicare, and may charge a premium in addition to the Part B premium. The Social Security Administration has in place a "safety net" to prevent the deduction of more than $300 of Part C and Part D plan premiums from a single Social Security check. For amounts over $300, the enrollee may be billed directly. |
||||
|
Figures provided by CMS, |
||||
|
See CRS Report |
||||
|
SSA §1840(b)(1). |
||||
|
Generally, employees of the federal government hired before 1984 are covered by the Civil Service Retirement System (CSRS) and are not covered by Social Security. Most federal workers first hired into federal service on or after January 1984 participate in the Federal Employees' Retirement System (FERS), which includes Social Security coverage. However, the Tax Equity and Fiscal Responsibility Act (P.L. 97-248) enabled federal workers to be eligible for Medicare based on their federal employment. See CRS Report R42741, Laws Affecting the Federal Employees Health Benefits (FEHB) Program. |
||||
|
Payment may be made by check, money order, or credit card; alternatively, one may schedule a payment to be automatically deducted from one's bank account. Premium billing form and information may be found at https://www.medicare.gov/forms-help-and-resources/mail-about-medicare/medicare-premium-bill.html. |
||||
|
Social Security Administration, Program Operations Manual, Section HI 01001.225, "When Premium Notices May Be Sent to an Individual Other Than an Enrollee," at https://secure.ssa.gov/apps10/poms.nsf/lnx/0601001225. |
||||
| 63.
|
|
64.
Social Security Administration, Program Operations Manual, Section HI 01001.230, "Group Collection-General," at https://secure.ssa.gov/poms.nsf/lnx/0601001230. |
Social Security Administration, Program Operations Manual, HI 01001.041: Collection from Beneficiaries When the Amount of the Benefit Payment is Less than the Amount of the Premium, https://secure.ssa.gov/apps10/poms.nsf/lnx/0601001041. |
|
| 65. |
This grace period may be extended for up to an additional three months if the enrollee can establish that nonpayment was due to circumstances beyond his or her control, such as being physically or mentally incapable of making premium payments or due to an administrative error. There is no financial hardship exemption, although those with sufficiently low income may qualify for premium assistance from a state Medicaid program. |
|||
| 66. |
Part B premium announcements are generally made in the fall prior to the effective year. |
|||
| 67. |
SSA §1839(a). |
|||
| 68. |
The actuarial rate for the disabled is defined as one-half of the expected average monthly cost per disabled enrollee. Average per capita costs for the disabled are generally higher than those for the aged; therefore, were these average costs included in the premium determination, all Part B enrollees could pay higher premiums. As general revenue funding is determined using both the average costs of the aged and the disabled, this funding is sufficient to compensate for the reduction in premium revenues due to not including the costs of the disabled in determining the premium amount. |
|||
| 69. |
The $9 billion consists of about $7.4 billion in increased federal spending due to the reduced standard premiums and about $1.6 billion in lost revenues due to the reduction in high-income adjustments. The $3.00 standard premium surcharge "pays for" the increased general revenue transfers in 2016, while the additional high-income surcharge adjustments are used to offset the reduction in the income-related adjustment amounts. CMS, "Medicare Program: Medicare Part B Monthly Actuarial Rates, Premium Rate, and Annual Deductible Beginning January 1, 2016," 80 Federal Register 70811, November 16, 2015. |
|||
| 70. |
2018 Medicare Trustees Report, p. 86. In the final year of the repayment adjustments, the surcharge may be set at less than $3.00 to avoid overpayment. |
|||
| 71. |
CMS, "Medicare Program: Medicare Part B Monthly Actuarial Rates, Premium Rate, and Annual Deductible Beginning January 1, |
|||
| 72. |
Rounded to the nearest dime. |
|||
| 73. |
The Medicare Prescription Drug, Improvement, and Modernization Act of 2003 (MMA; P.L. 108-173) would have phased in the increase over five years; however, the Deficit Reduction Act of 2005 (DRA; P.L. 109-171) shortened the phase-in period to three years. |
|||
| 74. |
At the time of enactment of the MMA, CBO estimated that 1.2 million persons (3% of beneficiaries) would pay higher premiums in 2007 and that 2.8 million persons (6% of beneficiaries) would pay higher premiums in 2013. CBO further estimated that the MMA provision would reduce federal outlays by $13.3 billion over the 2007-2013 period. CBO estimated that the DRA provision accelerating the phase-in would increase premium collections by $1.6 billion over the 2007-2010 period. The MMA estimate and the DRA estimate were made by CBO at the time of enactment of each law. Both estimates were based on the CBO budget baseline in effect at the time. As is the case for all CBO estimates, the earlier estimates are incorporated into subsequent CBO baselines. Therefore, the two savings estimates cannot be added together. |
|||
| 75. |
Estimate provided by CMS, |
|||
| 76. |
For additional information see Social Security Administration Publication, "Medicare Premiums: Rules for Higher-Income Beneficiaries," at https://www.ssa.gov/pubs/EN-05-10536.pdf. |
|||
| 77. |
If an enrollee amended his or her tax return and doing so changed the income used to determine the high-income adjustments, the updated information may be provided to the Social Security Administration so that the administration may correct or remove the income-related monthly adjustment amounts. |
|||
| 78. |
Defined at SSA §1839(i)(4). See also Social Security Administration, Program Operations Manual, Section HI 01101.010, "Modified Adjusted Gross Income (MAGI)," at https://secure.ssa.gov/poms.nsf/lnx/0601101010. |
|||
| 79. |
Internal Revenue Code §61. |
|||
| 80. |
Internal Revenue Code §62. |
|||
| 81. |
The definition of MAGI for the income-related monthly adjustment amount (IRMAA) in Medicare is different from the MAGI definition in certain ACA Medicaid provisions. See CRS Report R43861, The Use of Modified Adjusted Gross Income (MAGI) in Federal Health Programs. |
|||
| 82. |
Social Security Form SSA-44, at http://www.ssa.gov/online/ssa-44.pdf. |
|||
| 83. |
20 C.F.R. §418.1205. |
|||
| 84. |
20 C.F.R. §418.1210. |
|||
| 85. |
Social Security Form SSA-561-U2, at http://www.ssa.gov/online/ssa-561.pdf. |
|||
| 86. |
SSA §1839(i). |
|||
| 87. |
In 2018, approximately 3. |
|||
| 88. |
ACA §3402. Because more beneficiaries are expected to pay this higher premium over time and therefore reduce the amount of general revenues needed to fund Part B, CBO scored this provision as saving the federal government $25 billion over 10 years (FY2010-FY2019), at http://www.cbo.gov/sites/default/files/cbofiles/ftpdocs/113xx/doc11379/amendreconprop.pdf. |
|||
| 89. |
MACRA §402. See CRS Report R43962, The Medicare Access and CHIP Reauthorization Act of 2015 (MACRA; P.L. 114-10). |
|||
| 90. |
Under prior law (ACA §3402), in 2020 and subsequent years, the income thresholds were to be indexed to inflation as if they had not been frozen between 2011 and 2019. In other words, the income thresholds would have reverted to the levels they would have reached had they been indexed for inflation since 2007, thereby reducing the proportion of beneficiaries who would be subject to higher premiums. CBO estimated that MACRA §402 would save $34.3 billion over 10 years. CBO, Cost Estimate of H.R. 2, Medicare Access and CHIP Reauthorization Act of 2015, March 25, 2015, https://www.cbo.gov/publication/50053. |
|||
| 91. |
These threshold changes |
|||
| 92. |
See Medicare.gov, "Medicare Savings Programs," at http://www.medicare.gov/your-medicare-costs/help-paying-costs/medicare-savings-program/medicare-savings-programs.html and Medicare Publication, "Get Help with Your Medicare Costs," at https://www.medicare.gov/ |
|||
| 93. |
See CRS Report R43357, Medicaid: An Overview. In those states that have extended Medicaid coverage to individuals 64 years of age and under with incomes of up to 138% of FPL, certain individuals at the higher income levels may no longer qualify for Medicaid when they turn 65. In other words, traditional Medicaid categorical and income eligibility (i.e., income and asset) rules will apply when an individual becomes eligible for Medicare. |
|||
| 94. |
Income and asset requirements may vary by state and change each year. These amounts do not include a burial-fund allowance of $1,500 per person. |
|||
| 95. |
For additional information about these programs and to learn whether a beneficiary might qualify for Medicare premium assistance, contact the applicable State Medical Assistance (Medicaid) office. (As the names of these programs may vary by state, one should specifically inquire about Medicare Savings Programs.) The contact information for state Medicaid offices may be obtained by calling 1-800-MEDICARE (1-800-633-4227) or by visiting the Medicare "contacts" website at http://www.medicare.gov/contacts. |
|||
| 96. |
The federal poverty levels for |
|||
| 97. |
The qualifying levels are slightly higher than the monthly federal poverty level because, by law, $20 per month of unearned income is disregarded in the calculation. See Social Security Administration, Program Operations Manual, Section HI 00815.023, "Medicare Savings Programs Income Limits," effective date February |
|||
| 98. |
The Qualified Medicare Beneficiary (QMB) program does not provide assistance with drug costs. Low-income beneficiaries who qualify for a Medicare Savings Program are automatically enrolled in Medicare Part D; their premiums and most cost sharing are paid for by the Part D low-income subsidy, which is financed through Medicare. States pay some of the costs for Part D low-income assistance through state transfer payments. |
|||
| 99. |
The qualifying levels are calculated the same way as for the QMB program. |
|||
| 100. |
In general, Medicaid payments are shared between the federal government and the states according to matching formulas. |
|||
| 101. |
§4732(c) of BBA 97 added §1933(c) of the SSA. |
|||
| 102. |
See CRS Report R43958, Health Care-Related Expiring Provisions, First Session of the 114th Congress. |
|||
| 103. |
MACRA appropriated $535 million for the remainder of CY2015 (April 1, 2015, through December 31, 2015) and $980 million for CY2016. The amount of funding for CY2017 and subsequent calendar years is based on the product of the following: (1) the previous year's Qualifying Individuals (QI) allocation; (2) the increase from the previous year in Medicare Part B premium; and (3) the estimated increase from the previous year in Part B enrollment. See CRS Report R43962, The Medicare Access and CHIP Reauthorization Act of 2015 (MACRA; P.L. 114-10). |
|||
| 104. |
For more information, see CRS Report R42035, Social Security Primer. |
|||
| 105. |
The Consumer Price Index-Urban Wage Earners and Clerical Workers (CPI-W) tracks the prices of a fixed market basket of goods and services over time. Social Security's cost-of-living adjustment (COLA) is calculated as the change in the CPI-W from the third quarter of the prior calendar year to the third quarter of the current calendar year. If the CPI-W increases during this period, Social Security benefits for the next year increase proportionately. |
|||
| 106. |
SSA §1839(f). This provision was originally created by the Deficit Reduction Act of 1984 (P.L. 98-369, Section 2302), extended by subsequent legislation, and made permanent by the Catastrophic Coverage Act of 1988 (P.L. 100-360, Section 211(b)) (this provision was not repealed when that law was repealed in 1989). Those who receive RRB benefits are also protected by this provision. The hold-harmless provision was first implemented in January 1987. |
|||
| 107. |
For more information on the hold-harmless provision, see CRS Report R44224, Potential Impact of No Social Security COLA on Medicare Part B Premiums in 2016, Potential Impact of No Social Security COLA on Medicare Part. |
|||
| 108. |
Note that Social Security benefit checks reflect benefit entitlements for the previous month, whereas Part B premiums are deducted in advance. For example, a November Social Security benefit check is not received until December, but it has December's Part B premium deducted from it. |
|||
| 109. |
Social Security Administration, Program Operations Manual, Section HI 01001.004, "The Variable Supplementary Medical Insurance Premium," at https://secure.ssa.gov/poms.nsf/lnx/0601001004. |
|||
| 110. |
The hold-harmless provision is applied on a case-by-case basis. For example, in a given year a Social Security COLA applied to most benefit levels may be sufficient to cover the dollar amount of a Part B premium increase for most beneficiaries; however, it may not be sufficient to fully cover the increase for someone who receives a smaller benefit amount, (i.e., the COLA percentage is applied to a smaller number, and the resulting dollar increase may not be sufficient to fully cover the Part B premium increase). In such a case, the hold-harmless provision would apply to that individual, and his or her Part B premiums may be lower than those paid by most beneficiaries in a given year. Thus, the hold-harmless provision may apply to a small number of beneficiaries each year. |
|||
| 111. |
See CRS Report |
|||
| 112. |
See CRS Report R41934, Ticket to Work and Self-Sufficiency Program: Overview and Current Issues; Social Security Administration, The Redbook at https://www.ssa.gov/redbook/documents/TheRedBook2017.pdf; and Social Security Administration, Disability Benefits For Wounded Warriors, pp. 13-14, at http://www.ssa.gov/pubs/EN-05-10030.pdf. Disabled military personnel may be required to enroll in Part B to maintain coverage under the Department of Defense health insurance, |
|||
| 113. |
A person who is entitled to Social Security spousal benefits, based on a spouse's work record instead of his or her own work record, may or may not be covered by the hold-harmless provision. If the government pension offset (GPO) were to reduce spousal benefits to zero, then the individual would not meet the hold-harmless provision's requirement of having benefit checks for December of the previous year and January of the current year. Therefore, this person would not be held harmless. If the person were to receive a Social Security spousal benefit for a positive dollar amount, then he or she would be covered by the hold-harmless provision. For more on the GPO, see CRS Report RL32453, Social Security: The Government Pension Offset (GPO). |
|||
| 114. |
Federal employees who exclusively worked under the Civil Service Retirement System (CSRS) are not eligible for Social Security benefits based on their own work record. See CRS Report 98-810, Federal Employees' Retirement System: Benefits and Financing. This program uses the same measuring period and formula for determining its COLAs as Social Security. See CRS Report 94-834, Cost-of-Living Adjustments for Federal Civil Service Annuities. |
|||
| 115. |
Social Security Administration, "How State and Local Government Employees Are Covered by Social Security and Medicare," at http://www.ssa.gov/pubs/EN-05-10051.pdf, and Social Security Administration, "State and Local Government Employers – Information," at http://www.ssa.gov/slge/. |
|||
| 116. |
See CRS Report RS22195, Social Security Disability Insurance (SSDI) and Medicare: The 24-Month Waiting Period for SSDI Beneficiaries Under Age 65. |
|||
| 117. |
For additional information, see Actuarial Note No. 147, by Jacqueline A. Walsh and Burt M. Kestenbaum, March 2006, at http://www.ssa.gov/OACT/NOTES/pdf_notes/note147.pdf. |
|||
| 118. |
The standard Part B premium in 2009 was also the same as that in 2008, $96.40; however, the lack of change in those years was not a result of the hold-harmless provision. At the end of 2008, it was determined that Part B premiums and general revenue financing in recent years had been set at somewhat higher levels than otherwise would be required to maintain an adequate contingency reserve, and that the level of assets in the Part B account of the SMI Trust Fund were more than adequate. Therefore, it was estimated that an adequate level of assets could be maintained throughout the next year, 2009, without an increase in premiums. |
|||
| 119. |
Most new enrollees in 2010 were eligible to be held harmless in the second year of no COLA (i.e., 2011); these individuals continued to pay the 2010 standard premium of $110.50 in 2011. |
|||
| 120. |
Social Security Administration, "Cost-of-Living Adjustment (COLA)," at http://www.socialsecurity.gov/cola/ and Social Security Administration Fact Sheet, "2015 Social Security Changes," at http://www.ssa.gov/news/press/factsheets/colafacts2015.html. |
|||
| 121. |
Boards of Trustees, Federal Hospital Insurance and Federal Supplementary Medical Insurance Trust Funds, 2015 Annual Report of the Boards of Trustees of the Federal Hospital Insurance and Federal Supplementary Medical Insurance Trust Funds, July 22, 2015, p. 32, at https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/ReportsTrustFunds/index.html. |
|||
| 122. |
As there is some overlap in categories—for example, some individuals may pay the high-income premiums and not yet receive Social Security benefits—these figures sum to more than 30%. |
|||
| 123. |
In the absence of BBA 15, the standard premiums of those not held harmless would have increased by about 52%, compared to an increase of about 16% that would have been paid by all enrollees had the hold-harmless rule not been in effect. For additional detail on how premiums would have been set for those not held harmless absent the enactment of BBA 15, see CRS Report R44224, Potential Impact of No Social Security COLA on Medicare Part B Premiums in 2016. |
|||
| 124. |
The CMS actuaries determined a 2016 standard premium of $118.80 per month. After the addition of the $3 per month surcharge added by the BBA 15, total 2016 standard premiums were $121.80 per month. CMS, "Medicare Program: Medicare Part B Monthly Actuarial Rates, Premium Rate, and Annual Deductible Beginning January 1, 2016," 80 Federal Register 70811, November 16, 2015. |
|||
| 125. |
For example, for an average retired worker with a benefit of $1,370 per month, a 0.3% increase would have been about $4.00. That person, therefore, would have seen a $4.00 increase in his or her Medicare Part B premium—from $104.90 in 2016 to about $109.00 in 2017. Someone with a $6.00 Social Security benefit increase, by contrast, would have seen a $6.00 increase in his or her 2017 premium (for a total premium of about $111.00). |
|||
| 126. |
The distribution of the types of enrollees not held harmless in 2017 was similar to that in 2016. See "Application of the Hold-Harmless Rule in 2016." |
|||
| 127. |
Boards of Trustees, Federal Hospital Insurance and Federal Supplementary Medical Insurance Trust Funds, 2016 Annual Report of the Boards of Trustees of the Federal Hospital Insurance and Federal Supplementary Medical Insurance Trust Funds, June 22, 2016, Table V.E2, at https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/ReportsTrustFunds/index.html. |
|||
| 128. |
CMS, "2017 Medicare Parts A & B Premiums and Deductibles Announced," press release, November 10, 2016, at https://www.cms.gov/ |
|||
| 129. |
Contingency reserve ratios are normally set at an amount between 15% and 20% of end-of-year assets compared to the following year's expenditures, with a usual target of 17%. In 2017, the reserve ratio was set at 13%. |
|||
| 130. |
Social Security Administration, "Social Security Announces 2.0 Percent Benefit Increase for 2018," press release, October 13, 2017, at https://www.ssa.gov/news/press/releases/2017/#10-2017-1; 2018 Medicare Trustees Report, Table V.E2. |
|||
| 131. |
|
|||
| 132. |
CMS, "2018 Medicare Parts A & B Premiums and Deductibles," fact sheet, November 17, 2017, at https://www.cms.gov/Newsroom/MediaReleaseDatabase/Fact-sheets/2017-Fact-Sheet-items/2017-11-17.html. |
|||
| 133. |
2018 Medicare Trustees Report, Table III.C5. For data on recent growth in specific Part B services, see the 2018 Medicare Trustees Report, pp. 126-137. |
|||
| 134. |
Ibid.
2018 Medicare Trustees Report, p. 8. |
|||
|
Other sources of income may include earnings from employment, employer-sponsored pension benefits, and investment earnings. In addition, retirees may draw down on their accumulated assets to supplement their income. |
||||
|
Social Security Basic Facts, as of |
||||
|
The COLA increases the benefits paid to current beneficiaries. In contrast, average Social Security benefits (those paid to new and current beneficiaries) have risen at a faster rate than the annual COLA, because the formula for calculating initial Social Security benefits is linked to wage growth, whereas the COLA is based on price growth. Generally, wages rise faster than prices. |
||||
|
In 2000, the ratio of Part A expenditures to Part B expenditures was 59:41. This ratio decreased to 50:50 in 2014 and is expected to drop to 45:55 in 2026. This means that over time, the proportion of Medicare expenditures covered under Part B is expected to increase. While providing more services on an outpatient basis may be more cost-effective for the program as a whole, it also means that beneficiaries will be expected to bear a larger portion of program costs over time. See CRS Report R43122, Medicare Financial Status: In Brief. |
||||
|
The hold-harmless provision caps the annual Part B premium increase (but not the Part D increase) at the dollar amount of a beneficiary's COLA. |
||||
|
Similarly, average Medicare cost sharing |
||||
|
The law does not specify that this method be used, but it also does not prohibit it. |
||||
|
Boards of Trustees, Federal Hospital Insurance and Federal Supplementary Medical Insurance Trust Funds, 2010 Annual Report of the Boards of Trustees of the Federal Hospital Insurance and Federal Supplemental Medical Insurance Trust Funds, August 5, 2010, pp. 97-98, at https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/ReportsTrustFunds/downloads/tr2010.pdf. |
||||
|
For example, the annual increase in the CSRS benefits is tied to the same inflation measure as Social Security; therefore, those under this system also received a 2. |
||||
|
For example, S. 2148, the Protecting Medicare Beneficiaries Act of 2015, and H.R. 3696, the Medicare Premium Fairness Act, both introduced on October 7, 2015, would have kept the 2016 Part B premiums at the 2015 level for all beneficiaries, including those with high incomes. Late-enrollment surcharges also would have been based on the 2015 standard premium. The loss of income from holding premiums flat in 2016 would have been offset by increased general revenue contributions. Note that these bills would have affected only premium determinations for 2016 and would not have made permanent changes to the hold-harmless |
||||
|
Charles Blahous, "How Social Security's COLA Politics Lead to Bad Policy," Economic Policies for the 21st Century at the Manhattan Institute, November 22, 2015, at |
||||
|
The CPI-E grows faster than the CPI-W, on average, because a larger portion of spending by the elderly goes toward health care expenditures and other items whose prices tend to rise more rapidly. As a result, switching to such a measure is projected to result in larger COLAs and higher Social Security benefits. |
||||
|
For example, in the 115th Congress, H.R. 991, the Guaranteed 3 Percent COLA for Seniors Act of 2017, would |
||||
|
Medicare Rights Center, "Medicare Trends and Recommendations: An Analysis of 2015 Call Data from the Medicare Rights Center's National Helpline," March 2017, at https://www.medicarerights.org/pdf/2015-helpline-trends-report.pdf. (Their March 2018 analysis of 2016 call data may be found at http://medicarerights.org/pdf/2016-helpline-trends-report.pdf.) The Medicare Rights Center also issued a related report entitled "A Costly Mistake: Missing Part B Enrollment," April 2015, at http://www.medicarerights.org/pdf/medicare-snapshot-040915.pdf. |
||||
|
See Medicare publication "Your Guide to Medicare Prescription Drug Coverage," p.20, at https://www.medicare.gov/Pubs/pdf/11109-Your-Guide-to-Medicare-Prescrip-Drug-Cov.pdf. |
||||
|
42 CFR §423.56. Employers or unions may also qualify for a federal subsidy to maintain prescription drug coverage for their retirees. Such subsidies are generally less expensive to the federal government than providing full coverage to such enrollees under Part D. 2018 Medicare Trustees Report, Table IV.B9. |
||||
|
The federal spending amount is net of beneficiary premiums. |
||||
|
See Department of Health and Human Services, Fiscal Year 2017 Budget in Brief, p. 76, at http://www.hhs.gov/sites/default/files/fy2017-budget-in-brief.pdf. |
||||
|
A Bipartisan Plan to Save Medicare and Reduce Debt, June 28, 2011. |
||||
|
America's Health Insurance Plans (AHIP), |
||||
|
AHIP, Trends in Medigap Enrollment and Coverage Options 2015, April 2017, at https://www.ahip.org/wp-content/uploads/2017/05/Medigap_Report_5.1.17.pdf. |
||||
|
See CRS Report R43934, President's FY2016 Budget: Centers for Medicare & Medicaid Services (CMS) Legislative Proposals. Subsequent Presidents' budgets did not contain this proposal. |
||||
|
The proposed FY2019 House Budget Resolution may be found at https:// |
||||
|
Most premium support models combine Parts A and B benefits; the premium subsidy and beneficiary premiums would apply to both of these parts of Medicare. |
||||
|
The Balanced Budget Act of 1997 (BBA 97; P.L. 105-33) made a change that had the effect of increasing the Part B premium over time. Prior to BBA 97, both Parts A and B of Medicare covered home health services. Payments were made under Part A, except for those few persons who had no Part A coverage. To extend the solvency of the Part A (Hospital Insurance) Trust Fund, BBA 97 gradually transferred coverage of some home health visits from Part A to Part B. Beginning January 1, 2003, Part A covers only post-institutional home health services for up to 100 visits, except for those persons with Part A coverage only who are covered without regard to the post-institutional limitation. Part B covers other home health services. |
||||
|
The Medicare Prescription Drug, Improvement, and Modernization Act of 2003 (MMA; P.L. 108-173) increased the Part B premium percentage for high-income enrollees; the Deficit Reduction Act of 2005 (DRA; P.L. 109-171) accelerated the phase-in period for such premiums. |
||||
|
SSA §1839(i)(5). |
||||
|
2015 Medicare Trustees Report, p. 32. |
||||
|
See CRS Report R44224, Potential Impact of No Social Security COLA on Medicare Part B Premiums in 2016. |
||||
|
The $9 billion consists of about $7.4 billion in increased federal spending due to the reduced standard premiums and about $1.6 billion in lost revenues due to the reduction in high-income adjustments. The $3.00 standard premium surcharge "pays for" the increased general revenue transfers in 2016, while the additional high-income surcharge adjustments are used to offset the reduction in the income-related adjustment amounts. CMS, "Medicare Program: Medicare Part B Monthly Actuarial Rates, Premium Rate, and Annual Deductible Beginning January 1, 2016," 80 Federal Register 70811, November 16, 2015. |
||||
|
2018 Medicare Trustees Report, p. 86. In the final year of the repayment adjustments, the surcharge may be set at less than $3.00 to avoid overpayment. |
||||
|
An individual eligible to enroll must be a resident of the United States. Further, the individual must either be a citizen or an alien lawfully admitted for permanent residence who has resided in the United States continuously for the immediately preceding five years. Section 1818A of the SSA provides for voluntary enrollment in Medicare Part A for certain disabled individuals who were entitled to coverage due to their receipt of disability benefits, but who have lost those benefits because they have returned to work and their incomes exceed the level of "substantial gainful activity." For additional information on Part A benefits for the disabled returning to work, see Social Security website "Working While Disabled," at http://www.socialsecurity.gov/pubs/10095.html. |
||||
|
The hold-harmless provision does not apply to Part A premiums. |
||||
|
"Medicare Program; CY |
||||
|
The Consolidated Appropriations Act of 2001 (P.L. 106-554) exempts certain state and local retirees, retiring prior to January 1, 2002, from the Part A late-enrollment penalty. These are groups of persons for whom the state or local government elects to pay the Part A late-enrollment penalty for life. The amount of the penalty which would otherwise be assessed is to be reduced by an amount equal to the total amount of Medicare payroll taxes paid by the employee and the employer on behalf of the employee. The provision applies to premiums beginning January 2002. |
||||
|
Similar to Part B, if one qualifies for and signs up during a special enrollment period, e.g., within 8 months of retiring, one may not be subject to a penalty. |
||||
|
Prior to enactment of the Consolidated Omnibus Budget Reconciliation Act of 1985 (COBRA; P.L. 99-272), there was no upper limit on the amount of the Part A surcharge or duration of the surcharge. COBRA limited the amount of the Part A surcharge to 10% and the duration to twice the period of delayed enrollment. |