Introduction
The Veterans Health Administration (VHA) of the Department of Veterans Affairs (VA) operates one of the nation's largest integrated direct health care delivery systems. The VHA estimates that in FY2020 it would provide care to about 6.33 million unique veteran patients.1 In the same year, VHA estimates that it would employ a staff of about 347,000 full-time equivalent employees2 at approximately, 1,456 VA sites of care,3 with an appropriation of approximately $80.6 billion.4
For other health care programs that are publicly funded—for example, Medicare, Medicaid, and the Children's Health Insurance Program (CHIP)—private providers in private facilities deliver most of the health care services. In contrast, the VA health care system could be categorized as a veteran-specific national health care system, in the sense that the federal government owns a majority of its health care delivery sites, employs the health care providers, and directly provides the majority of health care services to veterans.5
It should be noted that VA health care is not a health insurance plan similar to what many individuals or employers purchase in the private health insurance market, nor does it have the same health insurance plan characteristics, such as coinsurances, deductibles, and premiums.6
This report provides responses to frequently asked questions about health care provided to veterans through the VHA. It is intended to serve as a quick reference for easy access to information. Where applicable, it provides the legislative background pertaining to the question. Throughout this report, VA and VHA are used interchangeably to refer to the VA health care system.
The report discusses three broad topics: (1) eligibility and enrollment (including how they differ), (2) medical benefits, and (3) the cost of care and the VA's authorities to bill and collect from third-parties when veterans have other health insurance or other sources of payment.
Eligibility
Are All Veterans Eligible for VA Health Care?
In general, not all veterans are eligible to receive VA health care services. To be eligible, veterans must meet both basic and more specific criteria.
Generally, a veteran has to meet three basic criteria to be eligible for VA health care.7 A veteran must (1) meet the statutory definition of a "veteran," meaning an "individual who served in the active military, naval, or air service and who was discharged or released under conditions other than dishonorable"8 (see text box for definitions of military discharges); (2) meet the statutory definition of "active duty," meaning full-time duty in the Armed Forces, other than active duty for training;9 and (3) have served a minimum period of 24 months of continuous active duty.10
Some veterans may meet the eligibility requirements listed above but, due to the discretionary nature of VA health system funding, may not be allowed to enroll in the system.11 (See the "Enrollment in the VA Health Care System" section below.)
|
Descriptions of Military Character of Discharge
Source: CRS, adapted from the Department of Defense, Enlisted Administrative Separations, DOD Instruction 1332.14, effective April 12, 2019 and the Manual for Courts-Martial United States (2019 edition). |
In addition to the general eligibility criteria above, Congress has enacted several measures to grant limited eligibility to certain categories of veterans for specific conditions or specific services under special treatment authorities. For example, the Honoring America's Veterans and Caring for Camp Lejeune Families Act of 2012 (P.L. 112-154) authorized the VHA to provide hospital care and medical services, for certain specified conditions, to certain veterans who served at the Marine Corps base at Camp Lejeune, North Carolina, during a specific period of time. Moreover, the Military Construction, Veterans Affairs, and Related Agencies Appropriations Act, 2018 (P.L. 115-141, as amended), provided eligibility for mental health care and behavioral health services to certain veterans with other-than-honorable (OTH) discharges. These specific eligibilities, among others, are discussed in the questions and answers below.
Is Eligibility Different for Members of the Reserves?
When not activated to full-time federal service, members of the Reserve components have limited eligibility for VA health care services.
Members of the Reserve components may be eligible for VA health care based on veteran status (i.e., previous military service) or service-connected disability (see text box on service-connected disability). Reservists achieve veteran status and are exempt from the 24-month minimum duty requirement (described above) if they (1) were called to active duty, (2) completed the term for which they were called, and (3) were granted a discharge under conditions that were other than dishonorable.
|
What Is a Service-Connected Disability? In general, a service-connected disability means that a disease or injury resulting in a disability, based on all the evidence, was incurred in the line of duty during military service. If the disabling condition was preexisting, then such disability was aggravated during such service.12 A veteran's military service need not have been during combat or a period of war. Currently, there are five ways to establish that a disability is service-connected:
The VA evaluates a disability based on a schedule (VA Schedule for Rating Disabilities, VASRD) of ratings (based on average impairment of earning capacity) and assigns ratings from 0% to 100% based on the severity of the disability. Ratings are assigned in 10% increments.18 When a veteran has more than one service-connected disability, the VA uses a formula to determine the combined rating of disability.19 |
Members of the Reserve components may be granted service connection for any injury they incurred or aggravated in the line of duty while participating in inactive duty training sessions, annual required training sessions, or active duty for training.
Injuries incurred during transfer from or to any of the above training sessions may also be granted as service-connected disabilities.20 In addition, Reserve component members who experience a heart attack, cardiac arrest, or stroke during training may have those medical events established as service-connected conditions.21
Is Eligibility Different for Members of the National Guard?
When not activated to full-time federal service, members of the National Guard have limited eligibility for VA health care services.
Similar to regular active duty servicemembers, members of the National Guard may be eligible for VA health care based on veteran status (i.e., previous military service) or service-connected disability.22
National Guard members achieve veteran status and are exempt from the 24-month minimum duty requirement (described above) if they (1) were called to active duty by federal executive order, (2) completed the term for which they were called, and (3) were granted a discharge under conditions that were other than dishonorable.
In contrast to when called to active duty by a federal executive order, National Guard members are not granted service connection for any injury, heart attack, cardiac arrest, or stroke that occurs while performing duty ordered by a governor for state emergencies or activities.23
Is Eligibility Different for Veterans Who Served on Active Duty at Camp Lejeune?
Certain veterans who served on active duty for a period of no fewer than 30 days between August 1, 1953, and December 31, 1987, and who worked or lived at Camp Lejeune are eligible to receive health care for certain medical conditions.
The Honoring America's Veterans and Caring for Camp Lejeune Families Act of 2012 (P.L. 112-154), as amended by the Consolidated and Further Continuing Appropriations Act, 2015 (P.L. 113-235, Division I, Title II, Section 243), established a presumptive service connection for veterans' health care for one or more of 15 diseases and health conditions that may be associated with exposure to trichloroethylene (TCE), tetrachloroethylene (PCE), vinyl chloride, and other contaminants discovered in drinking water supplies at Camp Lejeune, North Carolina. Veterans and their family members who worked or lived at Camp Lejeune for no less than 30 days (consecutive or nonconsecutive) from August 1, 1953, to December 31, 1987, generally are eligible for VA health care services under this law.24 Eligible veterans and family members can receive free care for any of the 15 covered illnesses or conditions.25 To be eligible, a veteran or former reservist or member of the National Guard (1) must have been stationed at Camp Lejeune, or traveled to Camp Lejeune as part of his or her professional duties, and (2) must have served on active duty26 for at least 30 (consecutive or nonconsecutive) days during the period beginning on August 1, 1953, and ending on December 31, 1987.27
Are Former Servicemembers with Discharges Characterized as Under Other–Than-Honorable (OTH) Conditions Eligible for VA Health Care?
Under certain circumstances, a former servicemember found to be dishonorably discharged for VA purposes may be eligible for VA health care services.
To be eligible for VA health care, a veteran generally has to meet certain criteria, including a discharge or release from active service under conditions other than dishonorable.28 A discharge that is characterized by the Department of Defense (DOD) as an honorable discharge or general under honorable conditions, with some exceptions, qualifies veterans for VA health care services.29 If the discharge is under OTH conditions, administrative discharge, or is a punitive bad conduct discharge (BCD), the VA is required to make a character of discharge (COD) determination on a case-by-case basis to determine eligibility.30 Generally, when a former servicemember with an OTH or BCD discharge applies for health care services, the VHA forwards the request for an eligibility determination by submitting VA Form 20-0986 to a Veterans Benefits Administration (VBA) Regional Office (RO).31 COD determinations result in one of three potential outcomes:
- 1. Honorable for VA purposes, meaning that the veteran qualifies for all veterans benefits, including health care benefits, provided that other eligibility criteria (such as minimum active duty service requirements) are met.
- 2. Dishonorable for VA purposes, but eligible to receive health care services, meaning that the veteran is eligible to receive health care only for service-connected or service-aggravated disabilities or conditions.32
- 3. Dishonorable for VA purposes due to a statutory bar to VA benefits, meaning that the veteran is not eligible for service-connected disability compensation or health care services. In essence, the VA is barred from providing any benefit or service to the former servicemember.33
Are There Special Eligibility Rules for Those Seeking Mental Health Care Services from the VA?
Certain former servicemembers with mental or behavioral health care needs, including risk of suicide or harming others, are eligible for an initial mental health assessment and subsequent mental health services, even if they were discharged from the military service under other-than-honorable (OTH) conditions. In addition, former servicemembers may qualify for emergency mental health care services.
Section 258 of the Military Construction, Veterans Affairs, and Related Agencies Appropriations Act, 2018 (P.L. 115-141, as amended by P.L. 115-182 and P.L. 115-251), authorized the VA to provide an initial mental health care assessment and subsequent mental or behavioral health care services to certain former servicemembers, including those who served in the Reserve components and who meet each of the following criteria:
- Conditions of discharge: the veteran served on active duty and was discharged or released under a condition that is not honorable (but not a dishonorable discharge), or was discharged by court-martial (i.e., those with a dishonorable discharge or a discharge by court-martial would not be eligible for mental health care services from the VA).
- Duration of service: the veteran served for a period of more than 100 cumulative days.
- Conditions of service: the veteran (1) was deployed in a theater of combat operations, in support of a contingency operation, or in an area at a time during which hostilities occurred, including by controlling an unmanned aerial vehicle (UAV) from a location other than such theater or area; or (2) was the victim of a physical assault of a sexual nature, a battery of a sexual nature, or sexual harassment.
- Not currently enrolled in VA's health care system.34
Those veterans with an OTH administrative discharge and who meet the above criteria are not required to enroll in VA's health care system, to meet the minimum active duty service requirements, or to pay any copayments for mental and behavioral health care services included under VA's standard medical benefits package.35
Emergency Mental Health Care Under Humanitarian Care Provisions
The Department of Veterans Affairs Health Care Programs Enhancement Act of 2001 (P.L. 107-135) provided the VA Secretary broad authority to furnish hospital care or medical services in emergency situations to any individual regardless of veteran status. This authority is generally referred to as the humanitarian care authority. Furthermore, the Jeff Miller and Richard Blumenthal Veterans Health Care and Benefits Improvement Act of 2016 (P.L. 114-315) requires VA emergency departments to, at a minimum, screen an individual for a medical emergency. If the facility determines that a medical emergency exists, the facility will provide care to stabilize the individual's emergency condition.36 The individual is generally billed for any emergency services provided.37
A former servicemember with a bad conduct or dishonorable discharge who is in distress and in need of emergency mental health services may be provided services under humanitarian care provisions.38 Former servicemembers can access the VA system by calling the Veterans Crisis Line39 or by visiting a VA emergency room, urgent care center, or VA medical center.
On March 7, 2017, during a hearing before the House Veterans' Affairs Committee, VA Secretary David Shulkin announced his intention to expand urgent mental health care services to former servicemembers with OTH administrative discharges. Under this initiative, effective July 5, 2017, a former servicemember with an OTH administrative discharge with an urgent mental health need would qualify for a 90-day episode of care, including inpatient, residential, or outpatient care.40 This initiative provides care beyond the requirement to stabilize the patient under humanitarian care provisions. During this 90-day period, the VBA may have time to complete a character of discharge determination and notify the VHA of the former servicemember's discharge status. The initiative also allows an additional 90 days of treatment to be authorized upon request to the Chief Medical Officer for the Veterans Integrated Service Network (VISN).41
Eligibility Based on Presumption of Mental Illness or Psychosis
Certain veterans, including those with an OTH administrative discharge, may qualify for free care under presumptions of eligibility for psychosis42 or mental illness other than psychosis to treat those conditions. Former servicemembers who meet either of the two presumptive criteria do not have to meet the minimum active duty service requirements, and they are not required to pay any copayments for the treatment of covered conditions.
Under the presumptive eligibility for psychosis, a former servicemember must have served on active duty during World War II, the Korean conflict, the Vietnam era, or the Persian Gulf War and developed an active psychosis (1) within two years after discharge from active duty and (2) before specific statutory dates associated with the war or conflict in which the servicemember served, as follows:
- World War II: before July 26, 1949.
- Korean conflict: before February 1, 1957.
- Vietnam era: before May 8, 1977.
- Persian Gulf War: before the end of the two-year period beginning on the last day of the Persian Gulf War.43
Under the presumptive eligibility for mental illness other than psychosis, a former servicemember must have served on active duty in the Persian Gulf War and developed an active mental illness other than psychosis (1) within two years after discharge and (2) before the end of the two-year period beginning on the last day of the Persian Gulf War.44
Are Veterans' Family Members Eligible for VA Health Care?45
Veterans' family members are not eligible for VA health care services. However, certain dependents and survivors may receive reimbursement from the VA for some medical expenses.
The Civilian Health and Medical Program of the Department of Veterans Affairs (CHAMPVA) pays for health care services to dependents and survivors of certain veterans. It is primarily a fee-for-service program that reimburses the cost of medical care provided by non-VA providers or facilities. On May 5, 2010, President Barack Obama signed into law the Caregivers and Veterans Omnibus Health Services Act of 2010 (P.L. 111-163), which expanded the CHAMPVA program to include the primary family caregiver of a post-9/11 veteran who has no other form of health insurance, including Medicare and Medicaid.46 Health care services covered by the act include counseling, training, and mental health services for the primary family caregiver.
The VA Maintaining Internal Systems and Strengthening Integrated Outside Networks Act of 2018 (VA MISSION Act; P.L. 115-182, as amended) further expanded eligibility for the CHAMPVA program to include the primary family caregiver of a pre-9/11 veteran.47 This expansion is currently being implemented in two phases, each of which requires the implementation of new information technology. Under the first phase, veterans with serious service-connected injuries incurred on or before May 7, 1975, will qualify for benefits over a two-year period beginning on the date when the VA certifies to Congress that it has fully implemented the information technology system required for the program. Under the second phase, those with serious service-connected injuries incurred between May 7, 1975, and September 11, 2001, will qualify for benefits two years after the implementation of the first phase.
Enrollment in the VA Health Care System
Once a Veteran Meets the Basic Eligibility Criteria, Is Enrollment in the VA Health Care System Guaranteed?
Generally, after a veteran meets the basic eligibility criteria of veteran status and minimum active duty requirements (as described in the preceding section), the veteran must qualify for enrollment based upon service-connected disability, income, and other factors, such as being a former prisoner of war (POW) or being awarded the Medal of Honor or Purple Heart.
Eligibility for and enrollment in VA health care has evolved over time. Various eligibility laws enacted since the 1920s created a complex structure of eligibility criteria that ultimately led to the Veterans' Health Care Eligibility Reform Act of 1996 ("Eligibility Reform Act," P.L. 104-262), which created the modern enrollment system in use today.
Prior to the 1996 reform, veterans with service-connected conditions or lower incomes generally had access to VA health care.48 Furthermore, eligibility criteria had been designed to limit access to care, because the provision of care was based on available budgetary resources. A National Academy of Sciences report from 1977 stated that
[t]he public policy rationale for the VA hospital system assumes two broad categories of eligible veterans: those who have a service-connected disabilities and those who do not. The VA hospital system was initially justified (and the substantial continuing investment in VA facilities and resources has been provided by the Congress) on the grounds that the facilities were (and continue to be) necessary to provide health care to veterans with service-connected disabilities. Eligible veterans without service-connected disabilities were to be treated only if spare capacity were available after the needs of veterans in the highest-priority eligibility category were met. The elaborate structure of eligibility rules enacted by the Congress was designed to control access to facilities. That structure rests on the implicit assumption that VA facilities have insufficient capacity to meet the needs of all eligible veterans who may apply for care.49
According to the General Accounting Office (GAO, now known as the Government Accountability Office):
The complex eligibility provisions that have developed over many decades are often ill-defined and confusing—which ultimately creates frustration for veterans and VA staff. Veterans are often uncertain about which services they are eligible to receive and what right they have to require VA to provide them. VA physicians are likewise frustrated by requirements that they determine, before treatment can be provided, whether a condition is related to a service-connected disability or whether, if left untreated, the condition would require immediate hospitalization.
Unlike public and private health insurance, VA cannot offer well-defined benefits or guarantee the availability of covered services. Further, because provision of VA care is contingent upon available resources, whether a veteran receives care can depend on where and when the veteran seeks care. To add to veterans' confusion, VA medical centers use different methods to ration care when funds are not sufficient to meet demand. Because of these problems, veterans may be unable to obtain needed health care services from VA facilities.50
Although the Eligibility Reform Act refers to "eligibility reform" in both its title and legal provisions, in practice, the legislation did not significantly alter the eligibility criteria described in the preceding section of this report.51 However, the act did require the VHA to manage the provision of hospital care and medical services through an enrollment system based on prioritization and available resources.52 As stated in the report language accompanying the act,
[t]he Act would direct the Secretary, in providing for the care of 'core' veterans, to establish and operate a system of annual patient enrollment and require that veterans be enrolled in a manner giving relative degrees of preference in accordance with specified priorities. At the same time, it would vest discretion in the Secretary to determine the manner in which such enrollment system would operate.53
Taking these issues into consideration, the Eligibility Reform Act established two broad mutually exclusive categories of eligibility:54
- 1. Veterans who meet one or more of the following criteria:
- veterans with service-connected disabilities;55
- veterans who are former prisoners of war;
- veterans exposed to certain toxic substances and environmental hazards, such as Agent Orange;
- veterans whose attributable income and net worth are not greater than an established "means test"; or
- veterans of World War I.
- 2. Veterans who do not meet any of the above criteria (i.e., veterans with no service-connected disabilities, who are not former prisoners of war, who were not exposed to certain toxic substances and environmental hazards, or with attributable incomes above an established "means test," and were not veterans of World War I).
Since the law's enactment, the enrollment categories have been amended through both statutory and regulatory changes.56 (For the current priority enrollment categories, see the Appendix.)
The Eligibility Reform Act provided clear intent that the provision of health care to veterans depends on available resources. The committee report accompanying it states that the provision of hospital care and medical services would be provided, "to the extent and in the amount provided in advance in appropriations Acts for these purposes. Such language is intended to clarify that these services would continue to depend upon discretionary appropriations."57
Beginning on October 1, 1998, the VA started enrolling eligible veterans in the VA health care system. Unless otherwise exempt, veterans are required to enroll in the VA health care system to receive inpatient hospital and outpatient medical care.58
Are Some Veterans Unable to Enroll Despite Meeting Basic Eligibility Criteria?
Under current regulations, veterans who do not have a compensable service-connected disability or meet other eligibility factors, and whose household incomes exceed both the VA national means test and a geographically based means test, are currently not allowed to enroll in the VA health care system.59
Generally, veterans with no service-connected conditions or other eligibility factors (as described above) may only qualify based on their gross household income (income of the veteran, spouse, and dependent children) and deductible expenses income for the previous calendar year. If a veteran's household income is above the VA National Means Test (NMT; see Table A-2) and the geographical income limits established by the U.S. Department of Housing and Urban Development (HUD) for the fiscal year that ended on September 30 of the previous calendar year (known as the Geographic Means Test [GMT]), based on the area that the veteran resides, then the veteran is not eligible to enroll.
One of the provisions of the 1996 Eligibility Reform Act stipulated that medical care to veterans be furnished to the extent that appropriations are made available by Congress on an annual basis. Based on this statutory authority, the Secretary of Veterans Affairs announced on January 17, 2003, that the VA would suspend enrolling veterans without service-connected disabilities and with incomes above the GMT.60 Those who had enrolled in the VA health care system prior to January 17, 2003, were not affected by this suspension.
The Consolidated Security, Disaster Assistance, and Continuing Appropriations Act, 2009 (P.L. 110-329), which was enacted on September 30, 2008, amended this enrollment suspension. The accompanying report language stated that funding "has been provided ... to support increased enrollment for Priority Group 8 veterans whose income exceeds the current veterans means test and geographic means test income thresholds by 10% or less."61 The act provided $375 million for FY2009 to fund increased enrollment. On January 21, 2009, the VA issued regulations indicating its plans to enroll new veterans who met the expanded means-test thresholds.62 The VA began enrolling new veterans on June 15, 2009.63 Since then, the VA has amended the Priority Group 8 income threshold annually.
Are There Different Enrollment Criteria for Returning Combat Veterans?
Veterans returning from a current combat theater of operations are allowed to enroll in VA health care for five years from the date of their most recent discharge or release without having to demonstrate a service-connected disability64or satisfy a means-test requirement. Veterans who enroll under this extended enrollment authority continue receiving health services after the five-year eligibility period ends.
Combat zones are designated by executive orders from the President, which generally set specific dates to establish the beginning and ending periods for each combat zone. Eligiblity for this enhanced enrollment provision can be established through one of three means:
- 1. a certificate of release of discharge from active duty (DD Form 214) containing notations of service in a designated theater of combat operations;
- 2. receipt of a combat-related medal; or
- 3. proof of receipt of hostile fire, imminent danger pay (IDP), or combat tax exemption.65
Generally, returning combat veterans are assigned to Priority Category 6, unless they are eligible for a higher priority category, and are not charged copays for medication or treatment of conditions that are potentially related to their combat service. At the end of the five-year period, veterans enrolled in Priority Category 6 may be reenrolled in Priority Category 7 or 8, depending on their service-connected disability status and income level, and may be required to make copayments for nonservice-connected conditions. The above criteria also apply to National Guard and Reserve personnel who were called to active duty by federal executive order and who served in a theater of combat operations after November 11, 1998.
In 2007, the National Defense Authorization Act (NDAA), FY2008 (P.L. 110-181), created the current five-year period of enrollment eligibility for veterans who served in a theater of combat operations after November 11, 1998. Prior to, enactment of this law, returning combat veterans were granted a two-year period of enrollment eligibility.66 The most recent discharge date is used for those servicemembers who are called to duty multiple times.
If returning veterans do not enroll during the five-year window (from the most recent date of discharge), future enrollment applications will be evaluated according to the priority category classifications described in the Appendix. For this reason, the VA encourages veterans to take advantage of the enhanced enrollment period.
How Do Veterans Enroll in VA Health Care?
A veteran may apply for enrollment at any time by submitting an enrollment application (online, in person, by mail, or by telephone) to a VA health care facility.67
Veterans must enroll in VA health care by completing and submitting the VA's application for health benefits (VA Form 10-10EZ).68 The application form requests information about the veteran's military service, demographics, and (as applicable) financial status. Veterans can apply for enrollment through the following avenues:
Online. Veterans may fill out and submit their benefit application electronically through the VA website.69 After completing the application online, the veteran will receive a message confirming that the application has been submitted. If the veteran has been recently discharged, the VA will gather the required service information.
In person. Veterans may apply for health care services at their local VA health facility. State departments of veterans affairs can assist veterans with in-person applications. Veterans typically receive their enrollment notification letters in the mail in less than one week.
By mail.70 Veterans who choose to mail their enrollment forms may download the form from the VA's website or pick one up at their local VA health facility.
By telephone. At present, veterans can complete and submit their enrollment application over the telephone. Beginning March 15, 2016, all veterans who served in a theater of combat operations after November 11, 1998, and who were discharged or released from active service on or after January 28, 2003, could apply for enrollment over the telephone.71 For other veterans, applications for enrollment over the telephone began on July 15, 2016.72
How Does the VA Process Applications?
The VA processes health benefits applications through either a VA medical facility or Health Eligibility Center (HEC).
Veterans designate which VA medical center or outpatient clinic they prefer to have their applications processed through, with the exception of four medical facilities.73 If veterans choose to have their applications processed through their local VA health facility, the staff will process the applications using the Veterans Health Information Systems and Technology Architecture (VistA). VistA is an integrated electronic health record system that the VA uses to record the care it provides; it also includes administrative tools.
If veterans choose to have the Health Eligibility Center (HEC) process their applications, the center staff will do so using the Workload Reporting and Productivity (WRAP) tool. HEC staff uses the WRAP tool to maintain and distribute health applications to reviewers, along with supporting documentation.74 The flowchart in Figure 1 depicts how the VA processes health care applications.
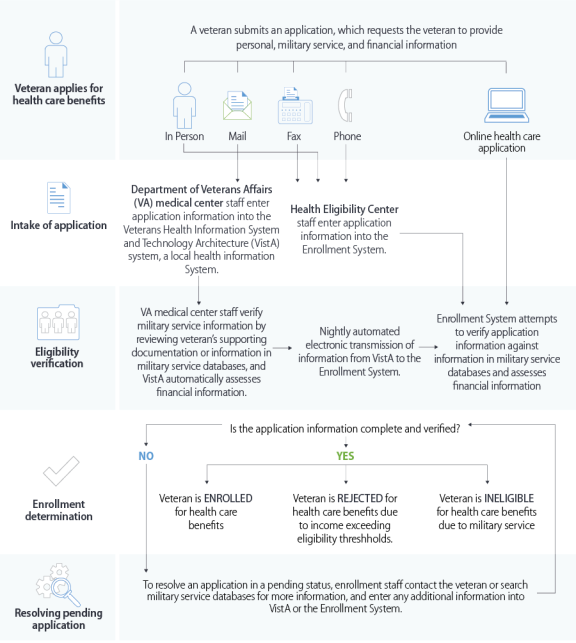 |
|
Source: Figure prepared by CRS based on figure titled "Key Steps for Veterans Health Administration's (VHA) Enrollment Processes, as of June 2017" in U.S. Government Accountability Office, VA Health Care: Opportunities Exist for Improving Implementation and Oversight of Enrollment Processes for Veterans, GAO-17-709 VA, September 2017, p. 7. |
What Happens After Veterans Receive Their Enrollment Notification Letters?
Veterans who are accepted into the VA health care system and placed into a priority category are considered enrolled.75
Veterans who are approved to receive medical benefits may schedule their first VA health care appointment after receiving their approved enrollment notification letter. Once approved, veterans will receive a personalized Veterans Health Benefits Handbook through the mail.76 This handbook details each veteran's individual medical benefits, copay status, and Enrollment Priority Category assignment. Veterans found by the VA to be ineligible for medical benefits may appeal the decision. Unenrolled veterans will receive letters explaining why they are unable to receive medical benefits; the letters provide instructions for appealing the VA's decision.
Once enrolled in the VA health care system, veterans retain that status unless they formally request to disenroll.77 "Enrolled veterans may seek care at any VA facility without being required or requested to reestablish eligibility for VA health care enrollment purposes."78
Veterans may cancel their health care enrollment with the VA at any time. Applications for reenrollment are accepted at any time by the VA. "Acceptance for future VA health care enrollment will be based on eligibility factors at the time of application, which may result in a denial of enrollment."79
Are There Categories of Veterans Who Are Not Required to Enroll in the VA Health Care System?
Although most eligible veterans must be enrolled in the VA health care system to receive VA health care, some categories of eligible veterans are exempt from this requirement.80
Any veteran who falls into one of the following categories is not required to apply for enrollment in the VA's health care system but is entitled to full health care benefits:
- A veteran with a service-connected disability rated at 50% or more. (Percentages of disability are based on severity; those with a rating of 50% or more are placed in Priority Category 1.)
- A veteran with a service-connected disability seeking care for that service-connected disability only.
- A veteran who has been discharged from military service for less than one year with a disability that the military determined was incurred or aggravated in the line of duty, but that has not yet been rated by the VA.
- A veteran who is disenrolled, but has a compelling medical need to complete a course of VA treatment that started when the veteran was still enrolled in the VA health care system.
- A veteran participating in VA's vocational rehabilitation program under certain criteria.
- A veteran who seeks care for psychosis or mental illness other than psychosis based on a diagnosis.
- A Commonwealth Army veteran or a new Philippine Scout.
Medical Benefits
What Are the Standard Medical Benefits?
The VA offers all enrolled veterans a standard medical benefits package that includes (among other things) inpatient care, outpatient care, and prescription drugs.
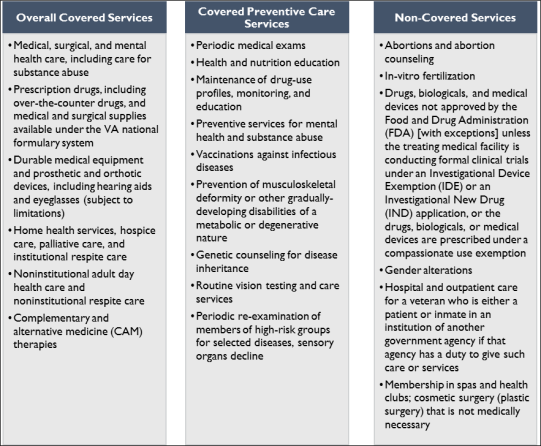
The VA's standard medical benefits package promotes preventive and primary care and offers a broad spectrum of inpatient, outpatient, surgical, and preventive health services. (See Figure 2.)
Does the VA Provide Gender-Specific Services for Women?81
The VA's standard medical benefits package addresses the health care needs of enrolled female veterans by providing (directly or through access to non-VA community providers) gynecological care, maternity care, infertility care, breast and reproductive oncology, and care for conditions related to military sexual trauma (MST), among other services.
The Caregivers and Veterans Omnibus Health Services Act of 2010 (P.L. 111-163) authorized the VA to provide certain health care services to a newborn child of a female veteran receiving maternity care furnished by the VA. Health care for the newborn is authorized for a maximum of seven days after the birth of the child if the veteran delivered the child in a VA facility or in another facility pursuant to a VA contract for maternity services.82
Under current regulations, the VHA does not provide abortions, abortion counseling, or medication to induce an abortion (e.g., mifepristone, also known as RU-486).83
|
Figure 2. Standard VA Medical Benefits: Covered and Not Covered |
 |
|
Source: Prepared by CRS based on 38 C.F.R. §17.38. |
Does the VA Provide Infertility Services to Veterans?
The VA does provide infertility services to veterans.
The VA provides infertility services to both service- and nonservice-connected veterans. Covered infertility services for both female and male veterans are illustrated in Table 1. The VA is not authorized to provide or cover the cost of in vitro fertilization (IVF) or other assistive reproductive technologies (ART). A narrow exception to this policy allows the VA to provide IVF services to veterans and their spouses if a service-connected disability results in the inability of the veteran to procreate without the treatment.84 This exception is authorized on an annual basis through appropriations acts.85 Such services and benefits may be provided in a manner similar to those described in a memorandum issued by the Assistant Secretary of Defense for Health Affairs ("Policy for Assisted Reproductive Services for the Benefit of Seriously or Severely Ill/Injured (Category II or III) Active Duty Service Members," dated April 3, 2013), along with guidance issued by the Department of Defense (DOD). The VA is exempt from DOD requirements applicable to the duration of embryo cryopreservation and storage.86 The VA is not authorized to cover gestational surrogacy treatment or costs associated with sperm or oocyte donation.87
Additionally, appropriations acts have authorized the VA to use funds to reimburse veterans for adoption expenses incurred by veterans with service-connected disabilities that results in the inability of the veteran to procreate without the use of fertility treatments.88 Reimbursement is capped at $2,000 per adopted child for an eligible veteran or for two eligible veterans who are spouses. No more than $5,000 can be paid to an eligible veteran in any calendar year regardless of the number of children adopted.89
|
Diagnosis and Treatment for Female Veterans |
Diagnosis and Treatment for Male Veterans |
|
Diagnostic Tests:
|
Diagnostic Tests:
|
|
Treatments:
|
Treatments:
|
Source: Prepared by CRS based on U.S. Department of Veterans Affairs, Veterans Health Administration, Infertility Evaluation and Treatment, VHA Directive 1332, June 2017.
Does the VA Provide Dental Care?
Eligibility for dental care differs significantly from eligibility requirements for medical care. The scope of dental services is generally narrow except in cases where a veteran has a service-connected dental condition, is a former prisoner of war (POW), or has a service-connected disability rated 100%.
The VA outpatient dental program categorizes enrolled veterans into classes that are distinct from the priority categories that enrolled veterans are placed in for medical care. The classes form the basis for the scope of dental treatment provided. Table 2 describes the eligibility criteria and scope of treatment for VA-provided dental care.
|
Classification |
Eligibility Criteria |
Scope of Treatment Provided |
|
Class I |
Veteran has a service-connected compensable (i.e., disability compensation is paid) dental condition. |
Any dental care and service needed regardless of relation to service-connected condition. |
|
Class II |
Veteran has a service-connected noncompensable dental condition (i.e., not subject to disability compensation) shown to have been in existence at the time of discharge or release from active duty service, which took place after September 30, 1981, ifa
|
A one-time course of dental treatment of the service-connected noncompensable dental condition. |
|
Class II(a) |
Veteran has a service-connected noncompensable dental condition or disability determined as resulting from combat wounds or service trauma. |
"Any dental care necessary to provide and maintain a functioning dentition. A Dental Trauma Rating (VA Form 10-564-D) or VA Regional Office Rating Decision letter (VA Form 10-7131) identifies the tooth/teeth/condition(s) that are trauma rated." |
|
Class II(b) |
Veteran is enrolled and may be homeless and receiving care for a period of 60 consecutive days in specified settings stipulated at 38 U.S.C. §2062. |
A one-time course of dental care that is determined clinically necessary to relieve pain, to help the veteran gain employment, or to "treat moderate, severe, or severe and complicated gingival and periodontal pathology." |
|
Class II(c) |
Veteran is a former prisoner of war (POW). |
Any dental care and service needed regardless of relation to service-connected condition. |
|
Class III |
Veteran has a dental condition clinically determined by VA to be aggravating a disability or condition from an associated service-connected condition or disability.c |
Dental care and services to treat such dental condition. |
|
Class IV |
Veteran whose service-connected disabilities have been rated at 100% or who is receiving the 100% rating by reason of individual unemployability. |
Any dental care and service needed regardless of relation to service-connected condition.d |
|
Class V |
Veteran is actively engaged in a vocational rehabilitation program (38 U.S.C. Chapter 31). |
Dental treatment clinically determined to achieve specific objectives.e |
|
Class VI |
Veteran is receiving VA care or is scheduled for inpatient care and requires dental services for "a dental condition complicating a medical condition currently under treatment." |
Outpatient dental care that is clinically necessary to treat "a dental condition complicating a medical condition currently under treatment." |
Source: Table prepared by CRS based on 38 C.F.R. §§17.160 – 17.166; Department of Veterans Affairs, Veterans Health Administration, Eligibility Determination, VHA Directive 1601A.02, November 2018; and Department of Veterans Affairs, Veterans Health Administration, Veterans Health Administration Dental Program, VHA Handbook 1130.01, February 2013.
a. P.L. 84-83, enacted on June 16, 1955, amends veterans' eligibility for outpatient dental services. This amendment makes veterans who have noncompensable dental conditions determined by the Veterans Benefits Administration (VBA) before 1955 ineligible for Class II outpatient dental treatment.
b. When servicemembers separate from active military service, they receive a certificate of release or discharge from active duty, known as a DD-214. The DD-214 provides the member and the service with a concise record of a period of service with the Armed Forces at the time of the member's separation, discharge, or change in military status (reserve/active duty). In addition, the form serves as an authoritative source of information for both governmental agencies and the Armed Forces for purposes of employment, benefits, and reenlistment eligibility, respectively.
c. A dental condition that may be caused by a mental condition (e.g., bruxism caused by post-traumatic stress disorder) is not eligible under Class III.
d. Veterans who receive disability compensation based on a 100% temporary rating, such as extended hospitalization for a service-connected disability, convalescence, or prestabilization, are not eligible for comprehensive outpatient dental services based on this temporary rating.
e. The objectives consist of "(1) making possible [veteran's] entrance into a rehabilitation program; (2) achieving the goals of [the veteran's] vocational rehabilitation program; (3) preventing interruption of [the veteran's] rehabilitation program; (4) hastening the return to a rehabilitation program if [the veteran is] in interrupted or leave status; (5) hastening the return to a rehabilitation program of a veteran placed in discontinued status because of illness, injury, or a dental condition; (6) securing and adjusting to employment during the period of employment assistance; or (7) enabling [the veteran] to achieve maximum independence in daily living." (Source: Appendix B, VHA Directive 1601A.02, November 2018.)
What Is the VA Dental Insurance Program for Veterans and Survivors and Dependents of Veterans (VADIP)?
The VA Dental Insurance Program (VADIP) is a pilot program that provides premium-based dental insurance coverage through which eligible individuals may choose to obtain dental insurance from a participating private insurer.90
The Caregivers and Veterans Omnibus Health Services Act of 2010 (P.L. 111-163) authorized the VHA to conduct a three-year pilot program to assess the feasibility and advisability of providing private, premium-based dental insurance coverage to eligible veterans and certain survivors and dependents.91 The three-year pilot program ended in January 2017. The Department of Veterans Affairs Dental Insurance Reauthorization Act of 2016 (P.L. 114-218) extended the VADIP until December 31, 2021. The VHA contracts with qualified dental insurance carriers to provide dental insurance and administer all aspects of the dental insurance plan. Dental insurance plans generally cover diagnostic services, preventive services, endodontic and other restorative services, surgical services, and emergency dental care.92
The VADIP is available to CHAMPVA beneficiaries and veterans enrolled in VA health care. Dependents of veterans who are not eligible under CHAMPVA are not eligible for VADIP. Participation in VADIP does not affect veterans' eligibility for other VA dental services.93
What Is the Pilot Program for Dental Health Care Access?
In December 2019, the VA Innovation Center proposed to establish a new pilot program that would provide a pathway for veterans who are enrolled in the VA health care system but are not eligible for dental care through the VA, to obtain pro bono or discounted dental care in the community.94
The VA MISSION Act of 2018 established a new Center for Innovation for Care and Payment to develop and conduct innovative pilot programs.95 The center is required to test payment and health care delivery models to reduce expenditures while preserving or enhancing the quality of care provided by the VA.96 As its first pilot program, the VA Innovation Center proposed creating a pilot program to provide care coordination to certain veterans who are not currently eligible for VA dental care. Under this program, VHA staff at selected pilot sites will provide care coordination services either through a call center or an automated self-service portal and connect veterans to dental care providers who are offering pro bono or discounted dental services and who have agreed to participate in the pilot. As an initial first step on December 6, 2019, VA submitted to Congress a waiver request to implement the pilot program as required by the VA MISSION Act of 2018.97 The request (H.J.Res. 80) was approved by Congress; however, it has not become law as of the date of this report. The VHA has indicated that it would announce the start date of the pilot program when all needed actions to commence the pilot program are complete.98
Does the VA Provide Hearing Aids and Eyeglasses?
Generally, the VA provides audiology and eye care services (including preventive care services and routine vision testing) for all enrolled veterans. The VA does not provide hearing aids or eyeglasses for normally occurring visual or hearing impairments.99
The VA provides hearing aids and eyeglasses to any veteran who meets one or more of the following circumstances:100
- has any compensable service-connected disability;
- is a former prisoner of war (POW);
- was awarded a Purple Heart;
- is receiving compensation for an injury, or an aggravation of an injury, that occurred as the result of VA treatment;
- is receiving an increased pension based on being permanently housebound and in need of regular aid and attendance;
- has hearing or vision impairment resulting from diseases or the existence of another medical condition for which the veteran is receiving VA care or services, or which resulted from treatment of that medical condition (e.g., stroke, polytrauma, traumatic brain injury, diabetes, multiple sclerosis, vascular disease, geriatric chronic illnesses, toxicity from drugs, ocular photosensitivity from drugs, cataract surgery, and/or other surgeries performed on the eye, ear, or brain resulting in a vision or hearing impairment);
- has significant functional or cognitive impairment evidenced by deficiencies in the ability to perform activities of daily living;101 or
- has hearing and/or vision impairment severe enough that it interferes with his or her ability to participate actively in medical treatment and to reduce the impact of dual sensory impairment (combined hearing and vision loss).
Does the VA Provide Long-Term Care?102
The VA provides long-term care services (including residential, home-based, and community-based care) for veterans meeting specified criteria, which may include service-connected conditions and the need for such care.
The Veterans Millennium Healthcare and Benefits Act (P.L. 106-117) requires the VA to provide nursing home services to all enrolled veterans who are 70% or more service-connected disabled, or 60% or more service-connected disabled and unemployable and in need of such care, or who are service-connected for a condition that makes such care necessary.103 The VA provides short- and long-term nursing care, respite, and end-of-life care through three different settings: (1) Community Living Centers (CLCs) located on VA medical campuses, (2) contracted care in Community Nursing Homes (CNHs), and (3) the State Veterans Nursing Home (SVNH) program.
Does the VA Provide Support to Caregivers of Disabled Veterans?
The VA provides extensive caregiver support and assistance through the Program of General Caregiver Support Services and the Program of Comprehensive Assistance for Family Caregivers.104 The VA is in the process of expanding eligibility for caregiver assistance.
The Caregivers and Veterans Omnibus Health Services Act of 2010 (P.L. 111-163) required the VA to establish caregiver support services to veterans. The VA established two programs: the Program of General Caregiver Support Services and the Program of Comprehensive Assistance for Family Caregivers. In addition, the VA maintains a caregiver support phone line and staffs each VA medical center with at least one caregiver support coordinator.105
The Program of General Caregiver Support Services (PGCSS) is available to caregivers of enrolled veterans of all eras. The program provides education, training, and technical support; telehealth services; respite care; and counseling. To be eligible for these services, a veteran must be enrolled in the VA health system and need personal care services because the veteran is either
- unable to perform one or more activities of daily living; or
- needs supervision or protection based on symptoms or residuals of neurological or other impairment or injury.
There is no application or clinical evaluation required to obtain benefits under the PGCSS. Individuals receiving services and benefits under this program are referred to as "general caregivers."
The Program of Comprehensive Assistance for Family Caregivers (PCAFC) is available to family caregivers of veterans and certain servicemembers who were seriously injured in the line of duty on or after September 11, 2001. These veterans or servicemembers are commonly referred to as "post-9/11 veterans." Eligibility for the program requires, at a minimum, six months of continuous and approved caregiver support that is in the best interests of the veteran or servicemember based on either of the same criteria listed above for the PGCSS program or a 100% service-connected disability rating with special monthly compensation that includes an aid and attendance allowance.
The PCAFC requires an extensive application process and clinical evaluation. Individuals granted services and benefits under this program are referred to as "family caregivers." A family caregiver may be designated as either a primary or secondary family caregiver for purposes of the program. This designation confers different services and benefits. Primary family caregivers are eligible for additional services and benefits not available to secondary family caregivers.
Table 3 lists the services and benefits available under the two caregiver support programs (i.e., the Program of General Caregiver Support Services and the Program of Comprehensive Assistance for Family Caregivers) and designates which of the three categories of caregiver status (i.e., general caregiver, secondary family caregiver, or primary family caregiver) are eligible for the specific service or benefit. The table is organized from the general caregiver category, which confers the least amount of services and benefits, to the primary family caregiver category, which confers the most amount of services and benefits.
|
Benefit |
Explanation of Service or Benefit |
General Caregiver |
Secondary Family Caregiver |
Primary Family Caregiver |
|
Program of General Caregiver Support Services (PGCSS) |
||||
|
Caregiver Support Line |
Licensed professionals staff the support line to connect caregivers with VA services. The support line also offers monthly telephone education groups. |
X |
X |
X |
|
Caregiver Support Coordinator |
A licensed professional who administers the VA caregiver programs and provides support to caregivers by matching them with services. There is a coordinator at each VA medical center. |
X |
X |
X |
|
Peer Support Mentoring |
Caregivers can participate in peer support as both mentors and mentees. This is usually a six-month program, but one-time support is also available. |
X |
X |
X |
|
Education, Training, and Technical Support |
The VA provides online and in-person education and training offerings to caregivers. The VA will also make referrals to non-VA community services. |
X |
X |
X |
|
Telehealth |
Telehealth enables physicians and nurses to monitor a veteran's medical condition remotely using home monitoring equipment. This is an indirect benefit to caregivers. |
X |
X |
X |
|
Counseling |
Counseling services are provided to a caregiver if the VA medical professional caring for the veteran determines that the services would further the objectives of the veteran's medical treatment. |
X |
X |
X |
|
Respite Care |
Allows a home health aide to go to a veteran's home to provide personal care services or take a veteran to a program while the caregiver takes a break. The respite care must be medically and age appropriate. |
X |
X |
X |
|
Program of Comprehensive Assistance for Family Caregivers (PCAFC) |
||||
|
Primary Care Team Support and Monitoring |
Ongoing monitoring of a veteran's overall health and well-being and adequacy of care and supervision being provided. |
NE |
X |
X |
|
Mental Health Services |
These services include individual and group therapy, individual counseling, and peer support groups. These services are limited to outpatient care only. |
NE |
X |
X |
|
Beneficiary Travel |
Travel reimbursement during the period in which a veteran is traveling to and from medical examination, treatment or care, and for the duration of such examination. |
NE |
X |
X |
|
Stipend |
A monthly stipend paid directly to the primary family caregiver. |
NE |
NE |
X |
|
Civilian Health and Medical Program (CHAMPVA) |
Health insurance program where primary family caregivers obtain medical care from private health care providers. |
NE |
NE |
X |
Source: Prepared by Congressional Research Service based on Title 38 C.F.R. §§71.40 and 71.50 as well as VHA Directive 1152(1).
Notes: X = Eligible. NE = Not eligible. VA = Department of Veterans Affairs. The statutory authority for all services and benefits under the PGCSS and PCAFC is 38 U.S.C. §1720G.
The VA Maintaining Internal Systems and Strengthening Integrated Outside Networks Act of 2018 (VA MISSION Act; P.L. 115-182 as amended by P.L. 115-251) expanded eligibility for the Program of Comprehensive Support for Family Caregivers to include pre-9/11 veterans. The expansion is contingent on the implementation and certification of a new information technology system for the program. Once the system is certified, the VA is authorized to enroll pre-9/11 veterans in two phases: first, veterans with service-connected injuries incurred on or before May 7, 1975, then, veterans with service-connected injuries incurred between May 7, 1975, and September 11, 2001.
Does the VA Pay for Medical Care in the Community?
Under certain circumstances, the VA pays for care in the community to eligible veterans.
The VA MISSION Act established the permanent Veterans Community Care Program (VCCP), replacing the Veteran's Choice Program (VCP) and the traditional community care program.106 The VCCP program was launched on June 6, 2019. To be eligible for care under VCCP, a veteran must be enrolled in the VA health care system, or not enrolled in the VA health care system but entitled to hospital care, medical services, and extended care services. Once these criteria are met, the veteran has to meet one of the following six criteria:107
- 1. The veteran needs a service that is not available at the veteran's regular VA medical facility.
- 2. The veteran resides in a U.S. state or territory that does not have a full-service VA medical facility (i.e., Alaska, Hawaii, New Hampshire, and the U.S. territories of Guam, American Samoa, the Northern Mariana Islands, and the U.S. Virgin Islands).
- 3. The veteran was eligible under the distance criteria mandated by the Veterans Choice Program (VCP) on the day before the VA MISSION Act was enacted into law (June 6, 2018), continues to meet the distance criteria, and either lives in one of the five states with the lowest population (i.e., North Dakota, South Dakota, Montana, Alaska, and Wyoming) or received care between June 6, 2017, and June 6, 2018, and requires care before June 6, 2020.
- 4. The veteran meets specific access standards for average drive time or appointment wait times, as follows.
- Average drive time to a specific VA medical facility:
- 30-minute average drive time for primary care, mental health care, and noninstitutional extended care services (including adult day health care).
- 60-minute average drive time for specialty care.
- Appointment wait time at a specific VA medical facility:
- 20 days for primary care, mental health care, and noninstitutional extended care services, unless the veteran agrees to a later date in consultation with a VA health care provider.
- 28 days for specialty care from the date of request, unless the veteran agrees to later date in consultation with a VA health care provider.
- 5. The clinician agrees that it is in the veteran's best medical interest to be referred to a community provider.
- 6. The veteran needs care from a VA medical service line that VA determines is not provider care that complies with VA's quality standards.108
If a veteran meets one of the six criteria, the VA authorizes care through the VA Community Care Network (CCN) of health care facilities and providers or at Department of Defense medical facilities, Indian Health Service medical facilities, any Federally Qualified Health Center (FQHC), or any other health care provider that meets criteria established by the VA Secretary.
Does the VA Pay for Health Care for Veterans Abroad?
The VA may pay for hospital care and outpatient services related to a service-connected disability or rehabilitation to any eligible veteran outside of the United States, without regard to the veteran's citizenship.109
The VA provides limited health care benefits to veterans residing or traveling outside the United States through the Foreign Medical Program (FMP). Under current law, the VA is authorized to provide hospital care and medical services to an eligible veteran outside the United States only if the VA "determines that such care and services are needed for the treatment of a service-connected disability of the veteran or as part of a rehabilitation program under chapter 31 [Vocational Rehabilitation and Employment (VR&E) program] of this title [38 U.S.C.]."110
Under the FMP, the VA pays the allowable amount for hospital and outpatient care. Veterans may generally select any health care provider. Claims for payment or reimbursement of services under the FMP must be submitted to the FMP office in Denver, CO. For care provided in Canada, claims must be submitted to Veterans Affairs Canada, Foreign Countries Operations Unit.111
Does the VA Pay for Emergency Care at Non-VA Facilities?
The VA may pay for emergency112 care provided to enrolled veterans by non-VA providers based on several factors, such as whether the care is for a service-connected condition or not.
Prior to the passage of the Veterans' Emergency Care Fairness Act (P.L. 111-137), the VA did not reimburse for emergency treatment for nonservice-connected conditions if the veteran had third-party insurance that paid any portion of the costs associated with that treatment.113 This included minimal insurance coverage, such as health coverage through an automobile insurance policy. The act required the VA to reimburse a veteran for the portion of the emergency care expenses not covered by a health plan contract, such as private health insurance. Following passage of the act, the VA interpreted it in such a way that it continued to deny reimbursement for nonservice-connected emergency care when the veteran had partial coverage under a health plan contract.
In response to this statutory interpretation by the VA, Richard W. Staab filed a lawsuit against the VA. In Staab v. McDonald, the U.S. Court of Appeals for Veterans Claims (CAVC) found that the act does require reimbursement in cases where a veteran has partial coverage under a health plan contract. In response to this CAVC ruling, the VA issued new regulations to implement the Staab decision pertaining to emergency care reimbursement for nonservice-connected care.114 However, under this new regulation, the VA stated that it "will not reimburse a veteran…for any copayment, deductible, coinsurance, or similar payment that the veteran owes the third party or is obligated to pay under a health-plan contract."115
In response to this new regulation, a lawsuit was filed against the VA by Amanda Jane Wolfe and Peter E. Boerschinger stating that, in general, the new regulation is inconsistent with congressional intent in passing the Veterans' Emergency Care Fairness Act. On September 9, 2019, CAVC ruled that VA's new regulations were contrary to the Veterans' Emergency Care Fairness Act and that the VA should reimburse deductible or coinsurance payments for which the veteran is responsible under a health plan contract.116 As of the date of this report, the VA has not publicly indicated whether it will appeal this ruling or promulgate new regulations.
Table 4 lists certain criteria that veterans must meet to be reimbursed for emergency services received from non-VA health facilities. (It should be noted that this table is based on regulations issued prior to the Wolfe and Boerschinger v. Wilkie ruling.)
|
The VA is required to pay or reimburse veterans for medical expenses incurred at non-VA facilities when the following conditions apply: |
|
|
Emergency Care for a Service-Connected Condition |
Emergency Care for a Nonservice-Connected Condition |
|
To be reimbursed under 38 U.S.C. §1728, a veteran must meet each of the following criteria:
|
To be reimbursed under 38 U.S.C. §1725, a veteran must meet each of the following criteria:a
|
Does the VA Pay for Urgent Care?
The VA MISSION Act authorized a new benefit for eligible veterans to obtain urgent care through certain community providers.
The VA MISSION Act of 2018, as amended, required the VA to implement a new benefit for covered veterans to obtain urgent care through eligible entities and providers.117 The benefit went into effect on June 6, 2019. Under the program, a veteran is eligible to receive limited, nonemergent (nonlife-threatening) health care services at qualified urgent care facilities and walk-in retail health clinics. To be eligible, a veteran must be enrolled in the VA health care system and must have received VA care in the past 24 months preceding the episode of urgent or walk-in care.118 Eligible veterans needing urgent care must obtain care through facilities that are part of the VA's contracted network of community providers.119 These facilities typically post information indicating that they are part of VA's contracted network. It is important to note that if an eligible veteran receives urgent care from a noncontracted provider or receives services that are not covered under the urgent care benefit, the veteran may be required to pay the full cost of such care.120 Certain veterans are required to pay copayments for care obtained at a VA-contracted urgent care facility or walk-in retail health clinic. Contracted clinics cannot bill a veteran for any copayment amount at the time of service (see Table 5). Veterans required to pay copayments under this benefit are separately billed by the VA.
|
Priority Category |
Copayment Amount |
|
Priority Categories 1-8 |
if the visit is only for immunization against influenza (flu shots): $0 copay |
|
Priority Categories 1-5 |
First three visits per calendar year: $0 copay |
|
Fourth and subsequent visits per calendar year: $30 per visit |
|
|
Priority Category 6 |
Care related to special treatment authorities:
|
|
Care not related to special treatment authorities:a $30 per visit |
|
|
Priority Categories 7-8 |
$30 per visit |
Source: 38 C.F.R. §17.4600 and Department of Veterans Affairs, Veteran Community Care – Urgent Care, Fact Sheet, May 2019, and Department of Veterans Affairs, VA health care copay rates, https://www.va.gov/health-care/copay-rates/.
a. Special treatment authorities include care related to Agent Orange exposure, service in Camp Lejeune, ionizing radiation, and Project 112/SHAD and Military Sexual Trauma (MST), among others.
Costs to Veterans and Private Health Insurance
Do Veterans Have to Pay for Their Care?
Whether a veteran is required to pay for VA health care services or not depends primarily on (1) whether the condition being treated is service-connected, and (2) the veteran's enrollment priority category.121
Veterans who are enrolled in the VA health care system do not pay any premiums. However, some veterans are required to pay copayments for medical services related to the treatment of a nonservice-connected condition. Table 6 summarizes which priority categories are charged copayments for inpatient care, outpatient care, outpatient medication, and long-term care services. Only veterans in Priority Category 1 (those who have been rated 50% or more service-connected disabled or awarded the Medal of Honor) and veterans who are deemed catastrophically disabled by a VA provider are never charged a copayment, even for treatment of a nonservice-connected condition.122
For veterans in other priority categories, the VHA has four types of nonservice-connected copayments for which veterans may be charged: outpatient, inpatient, extended care services, and medication copayments.123 (The cost of outpatient medication is discussed in the subsequent section.) Veterans in all priority categories are not charged copayments for a number of outpatient services, including publicly announced VA health fairs, screenings and immunizations, smoking and weight loss counseling, telephone care, laboratory services, flat film radiology, and electrocardiograms.
For primary care outpatient visits, there is a $15 copayment charge; for specialty care outpatient visits, there is a $50 copayment charge. Veterans do not receive more than one outpatient copayment charge per day. That is, if the veteran has a primary care visit and a specialty care visit on the same day, the veteran pays only for the specialty care visit. Veterans in Priority Categories 1 through 5 are not required to pay inpatient or outpatient copayments. Veterans in Priority Category 6 may be exempt due to a special eligibility for the treatment of certain conditions. Veterans enrolled in Priority Category 7 and certain other veterans are responsible for paying 20% of the VA's inpatient copayment. Veterans enrolled in Priority Category 8 and certain other veterans are responsible for the VA's full inpatient copayment.
Veterans in some priority categories are required to pay long-term care copayments. For these veterans, such charges are based on three levels of nonservice-connected care, including inpatient, noninstitutional, and adult day health care. Actual copayments vary, depending on the veteran's financial situation.
The VHA bills private health insurers for medical care, supplies, and prescriptions provided to veterans for their nonservice-connected conditions. Although the VA cannot bill Medicare, it can bill Medicare supplemental health insurance carriers for covered services.124 Veterans are not responsible for paying any remaining balance of the VA's insurance claim that is not paid or covered by their health insurance carrier. Any payment received by the VA is used to offset ''dollar for dollar'' a veteran's VA copayment responsibility.125
|
Priority Category |
Outpatient Services |
Inpatient Services |
Long-Term Care Services (Daily Max) |
|||||||||||||||
|
Basic Care |
Specialty Care |
First 90 days of care during a 365-day period |
Each additional 90 days during a 365-day period |
Daily Per Diem Charge |
Nursing Home Care/ Inpatient Respite Care/ Geriatric Evaluation |
Adult Day Health Care/ Outpatient Geriatric Evaluation/ Outpatient Respite Care |
Domiciliary Care |
Spousal Resource Protection Amount |
||||||||||
|
SC |
NSC |
SC |
NSC |
SC |
NSC |
SC |
NSC |
SC |
NSC |
SC |
NSC |
SC |
NSC |
SC |
NSC |
SC |
NSC |
|
|
1 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
|
2 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
|
3 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
|
4a |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
up to 97 |
0 |
0 |
0 |
up to 5 |
0 |
128,640 |
|
5 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
up to 97 |
0 |
up to 15 |
0 |
up to 5 |
0 |
128,640 |
|
6b |
0 |
15 |
0 |
50 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
up to 97 |
0 |
up to 15 |
0 |
up to 5 |
0 |
128,640 |
|
7 |
0 |
15 |
0 |
50 |
0 |
281.60 |
0 |
140.80 |
0 |
2 |
0 |
up to 97 |
0 |
up to 15 |
0 |
up to 5 |
0 |
128,640 |
|
8 |
0 |
15 |
0 |
50 |
0 |
1,408 |
0 |
704 |
0 |
10 |
0 |
up to 97 |
0 |
up to 15 |
0 |
up to 5 |
0 |
128,640 |
Source: CRS summary based on Department of Veterans Affairs, VA health care copay rates, https://www.va.gov/health-care/copay-rates/.
Notes: SC = service-connected; NSC = nonservice-connected.
a. The Caregivers and Veterans Omnibus Health Services Act of 2010 (P.L. 111-163) exempted veterans determined by the VA to be catastrophically disabled from inpatient, outpatient, medication, and noninstitutional extended care services copayments.
b. Priority Category 6 are veterans claiming exposure to Agent Orange; veterans claiming exposure to environmental contaminants; veterans exposed to ionizing radiation; combat veterans within five years of discharge from the military; veterans who participated in Project 112/SHAD (Shipboard Hazard and Defense); veterans claiming military sexual trauma; Camp Lejeune veterans receiving VA-provided health care for one of the 15 identified illnesses or conditions; and veterans with head and neck cancer who received nasopharyngeal radium treatment while in the military. Such veterans are subject to copayments when their treatment or medication is not related to their exposure or experience. The initial registry examination and follow-up visits to receive examination results are not billed to the health insurance carrier and are not subject to copayments. However, care provided that is not related to exposure (i.e., if it is nonservice-connected) will be billed to the insurance carrier and copayments can apply.
Do Veterans Have to Pay for Their Medications?
Some veterans are required to pay copayments for each 30-day supply of medication provided on an outpatient basis. Veterans do not pay copayments if they have a service-connected disability rating of 50% or higher, have a Medal of Honor, are former POWs, are catastrophically disabled, or if the medication is for a service-connected disability.126
The Omnibus Budget Reconciliation Act of 1990 (P.L. 101-508) authorized the VA to charge most veterans $2 for each 30-day supply of medication furnished on an outpatient basis for treatment of a nonservice-connected condition. The Veterans Millennium Health Care and Benefits Act of 1999 (P.L. 106-117) authorized the VA to increase the medication copayment amount by prescribing regulations, and to establish annual caps on the total amount paid by veterans enrolled in Priority Categories 2 through 6 in order to protect them from financial hardship.
For many years since then, the VA gradually increased the copayment amount through rulemaking by tying it to any increase in the prescription drug component of the Medical Consumer Price Index (CPI-P). In January 2006, the copayment amount increased to $8 and the annual cap on Priority Categories 2 through 6 increased to $960. The VA generally charged a flat copayment amount of $8 for all medications provided on an outpatient basis. As the prices based on the drug component of the CPI-P began to increase beyond $8, the VA, through a series of rulemakings, froze the copayment amount at $8 and the cap at $960 to alleviate any financial hardships for certain veterans. Starting on July 1, 2010, the VA allowed the copayment amount to increase to $9 for veterans in Priority Categories 7 and 8. On January 1, 2013, the VA froze the copayment amount at this rate for veterans in these priority categories. No copayment cap was established for these veterans.
In January 2016, the VA proposed regulations to change the flat rate medication structure and institute a new tiered copayment structure that would vary depending upon the class of medication.127 These new regulations went into effect on February 27, 2017.128
Veterans are charged copays for each medication per supply up to 30 days. Veterans pay a $5 copay for tier 1 or preferred generics, an $8 copay for tier 2 or nonpreferred generics, and an $11 copay for tier 3 or brand-name medications (see Table 7).
Veterans enrolled in Priority Categories 2 through 8 have a $700 calendar-year cap on the amount that they can be charged for these copayments.129 After reaching the $700 cap during the calendar year, a veteran may continue to receive medications without paying any additional copayments. Veterans who are unable to pay the VA's copayment charges may submit requests for assistance, including waivers, hardships, compromises, and repayment plans.130
The VA has developed criteria for determining tier 1 medications, and each year it identifies a subset of multisource medications as tier 1 medications.131 In addition to being FDA-approved and available from multiple sources, tier 1 medications must:
- cost the VA $10 or less for a 30-day supply;
- be available on the VA national formulary;
- be among the top 75 most commonly prescribed medications; and
- be primarily used to either treat or manage a chronic condition, or to reduce the risk of adverse health outcomes secondary to the chronic condition.
Topical creams, treatments for musculoskeletal conditions, antihistamines, steroid-containing medications, and antibiotics primarily used for short periods to treat infections cannot be considered for tier 1 status.
|
Priority Category |
Medication Tier |
Up to a 30 day supply per medication |
|
2 through 8a |
Tier 1 medications (preferred generics)b |
$5 |
|
Tier 2 medications (nonpreferred generics and some over-the-counter medications)c |
$8 |
|
|
Tier 3 medications (brand-name) |
$11 |
Source: Department of Veterans Affairs, VA health care copay rates, https://www.va.gov/health-care/copay-rates/. Also available at https://www.va.gov/COMMUNITYCARE/revenue_ops/copays.asp.
Note: For veterans in Priority Categories 2-8, the annual outpatient prescription medication copayment is capped at $700.
a. Veterans enrolled in Priority Category 1 do not pay copayments for outpatient medication.
b. A list of tier 1 medications is available at https://www.pbm.va.gov/PBM/Tiered_Copay/Tier_1_CO-PAY_MEDICATION_LIST.pdf.
c. A list of tier 2 and 3 medications is available at https://www.pbm.va.gov/PBM/Tiered_Copay/TierCopayExcelPPSN.xlsx.
Can Veterans Who Receive Health Care from the VA for Service-Connected Conditions Contribute Toward Health Savings Accounts (HSAs)?132
Provided veterans meet certain eligibility criteria, they may contribute toward health savings accounts.
The Surface Transportation and Veterans Health Care Choice Improvement Act of 2015 (P.L. 114-41) expanded the ability of veterans who receive care from the VA for service-connected disabilities to contribute toward health savings accounts (HSAs). This change went into effect January 1, 2016.
HSAs are one way individuals can pay for unreimbursed medical expenses (deductibles, copayments, and services not covered by health insurance) on a tax-advantaged basis.133 Only eligible individuals can establish and fund HSAs. To be eligible, one must be covered under an HSA-qualified high-deductible health plan (HDHP),134 cannot have disqualifying coverage,135 and cannot be claimed as a dependent on a different taxpayer's return. In general, an individual's eligibility to contribute to an HSA is determined on a monthly basis.
Prior to 2016, receiving care from the VA limited veterans' ability to contribute to HSAs. Veterans who were otherwise eligible to contribute to an HSA would not be considered eligible to contribute to their HSA in any month in which they had received care from the VA during the preceding three months.136
But under P.L. 114-41, individuals who were otherwise eligible to contribute to an HSA are no longer prohibited from contributing to an HSA merely because they receive medical care from the VA for a service-connected disability.
Can the VA Bill Private Health Insurance?
The VA has the authority to bill most health insurers for nonservice-connected care provided to veterans enrolled in the VA health care system.
To help defray the cost of delivering medical services to veterans, the Consolidated Omnibus Budget Reconciliation Act of 1985 (P.L. 99-272), enacted into law in 1986, gave the VHA the authority to bill some veterans and most health care insurers for nonservice-connected care provided to veterans enrolled in the VA health care system.137 This law also established means-testing for veterans seeking care for nonservice-connected conditions.138 Congress authorized the VHA to collect reasonable charges for medical care or services (including the provision of prescription drugs) from a third party to the extent that the veteran or the provider of the care or services would be eligible to receive payment from the third party for (1) a nonservice-connected disability for which the veteran is entitled to care (or the payment of expenses of care) under a health plan contract;139 (2) a nonservice-connected disability incurred as a result of the veteran's employment and covered under a worker's compensation law or plan that provides reimbursement or indemnification for such care and services;140 or (3) a nonservice-connected disability incurred as a result of a motor vehicle accident in a state that requires automobile accident reparations (no fault) insurance.141 Similarly, the VHA can receive payments from Medicare supplemental coverage plans (also known as medigap policies, which are private insurance plans that may pay medical expenses not paid by Medicare) for nonservice-connected conditions for which the veteran receives care at VHA facilities.
The VHA will not recover or collect charges from third-party private health insurers or the veterans for care or services provided to veterans who receive care under special statutory treatment authorities (e.g., exposure to tactical herbicides during the Vietnam era, ionizing radiation, and certain chemical and biological weapons testing; for conditions attributable to service in the Southwest Asia theater during the Persian Gulf War; and for certain veterans at Camp Lejeune during specified periods of time).142 In other words, the VA provides full coverage in these cases without cost sharing.
Veterans are not responsible for paying any remaining balance of the VA's insurance claim not paid or covered by their health insurance plan. This means that the VA does not "balance bill" the veteran143 Moreover, any payment received by the VA is used to offset ''dollar for dollar'' a veteran's VA copayment responsibility.144
Can the VA Bill Medicare?
The VA is statutorily prohibited from billing Medicare145 in most situations. In addition, veterans are responsible for paying all Medicare premiums, deductibles, and co-insurance. The VA has no authority to reimburse VA-enrolled Medicare beneficiaries for expenses they incur to obtain care under Medicare.146
In general, Medicare is prohibited from reimbursing the VA for any services unless:
- the provider is determined by the Secretary of Health and Human Services (HHS) to be providing services to the public as a community institution or agency;
- the provider is providing services through facilities operated by the Indian Health Service (IHS);147 or
- the services were provided in an emergency (in a hospital setting).
In addition, Medicare is prohibited from making payments to any federal health care provider who is obligated by law or contract to render services at public expense.148 Therefore, the VHA is statutorily prohibited from receiving Medicare payments for services provided to Medicare-covered veterans.149 This statutory prohibition applies to Medicare Part C (Medicare Advantage Plans) as well.
Although the legislative history does not indicate congressional intent for this, in United States v. Blue Cross & Blue Shield of Maryland, Inc., the majority opinion stated that "a safe assumption to be drawn from the exclusion of Medicare [from paying for health care services provided through other federal entities] is that Congress wanted to avoid the unnecessary transfer of federal funds from Medicare to the VA when the money is all coming out of the same coffer."150
It should be noted that there is a narrow exception to this statutory prohibition of Medicare reimbursing the VHA. Under current law, the VHA can be reimbursed by Medicare (notwithstanding any condition, limitation, or other provision in title XVIII of the Social Security Act) when the VA provides services to Medicare-covered individuals who are not eligible for care under Title 38, U.S. Code (U.S.C.), Chapter 17,151 and who are afforded VA care or services under a "sharing" agreement.152 A sharing agreement is a written contract that allows the VHA to buy, sell, or exchange health care resources and services with non-VA facilities. The VHA may enter into noncompetitive sharing agreements with affiliated institutions (e.g., affiliated medical schools—affiliated with VHA under 38 U.S.C. §7302) and other entities associated with these affiliated institutions (e.g., university hospitals).
Appendix. VA Priority Categories and Their Eligibility Criteria
The VA classifies veterans into eight enrollment priority categories based on an array of factors, including (but not limited to) service-connected disabilities or exposures,153 prisoner of war (POW) status, receipt of a Purple Heart or a Medal of Honor, and income. The criteria for each priority category are summarized in Table A-1.
The eight priority categories fall into two broad groups. The first group is composed of veterans with service-connected disabilities or with attributable incomes below the VA's National Means Test (NMT) threshold. These veterans are regarded by the VA as "high-priority" veterans, and they are enrolled in Priority Categories 1-6. Veterans enrolled in Priority Categories 1-6 include the following:
- veterans in need of care for a service-connected disability;
- veterans awarded the Purple Heart or the Medal of Honor;
- veterans who have a compensable service-connected condition;
- veterans whose discharge or release from active military, naval, or air service was for a compensable disability that was incurred or aggravated in the line of duty;
- veterans who are former POWs;
- veterans who have been determined by the VA to be catastrophically disabled;
- veterans of World War I;
- veterans who were exposed to hazardous agents (such as Agent Orange in Vietnam) while on active duty; and
- veterans who have an annual income below the VA's National Means Test (NMT) threshold (see Table A-2).
The VA considers applicants' gross household income (earned and unearned) and deductible medical expenses for the previous year to determine their specific priority categories and whether they have to pay copayments for nonservice-connected care.154 In addition, veterans are asked to provide the VA with information on any health insurance coverage they have, including coverage through employment or through a spouse. The VA may bill these payers for treatment of conditions that are not a result of injuries or illnesses incurred or aggravated during military service (i.e., not service-connected).
The second group of veterans is composed of those who do not fall into one of the first six priority categories—primarily veterans with nonservice-connected medical conditions and with incomes above the VA-established means test threshold (see Table A-2). These veterans are enrolled in Priority Categories 7 or 8.155
Table A-1. VA Priority Categories and Placement Criteria
A veteran is placed in the highest priority category for which the veteran meets at least one criterion
|
Priority Category |
Enrolled Veteran Placement Criteria |
|
1 |
|
|
2 |
|
|
3 |
|
|
4 |
|
|
5 |
|
|
6 |
|
|
7 |
|
|
8 |
|
Source: Prepared by CRS based on information from Department of Veterans Affairs, Veterans Health Administration, Eligibility Determination, VHA Directive1601A.02, November 21, 2018.
Notes: Service-connected disability means a disability that was incurred or aggravated in the line of duty in the active military, naval, or air service.
a. Veterans in receipt of the Medal of Honor are in Priority Category 1. This change occurred with the enactment of the Jeff Miller and Richard Blumenthal Veterans Health Care and Benefits Improvement Act of 2016 (P.L. 114-315) on December 16, 2016.
b. Veterans who are former POWs are placed in Priority Category 3. This change occurred with the enactment of the Former Prisoner of War Benefits Act of 1981 (P.L. 97-37) on August 14, 1981.
c. Veterans in receipt of a Purple Heart are in Priority Category 3. This change occurred with the enactment of the Veterans Millennium Health Care and Benefits Act (P.L. 106-117) on November 30, 1999.
d. Project 112 and Project SHAD were chemical and biological weapon experimentation projects conducted by the Department of Defense (DOD) between 1962 and 1973.
|
Veterans with— |
Free VA prescriptions and travel benefits for veterans with incomes (annual VA pension rate) of— |
Free VA prescriptions and travel benefits for veterans with VA pension with aid and attendance incomes of— |
Free VA prescriptions and travel benefits for veterans with VA pension with housebound benefit incomes of— |
Free VA health care for veterans with incomes of— |
Enrollment in Priority Category 8 for veterans with incomes of—a |
|
No dependents |
$13,752 or less |
$22,939 or less |
$16,805 or less |
$34,171 or less |
$37,588 or less |
|
1 dependent |
$18,008 or less |
$27,195 or less |
$21,063 or less |
$41,005 or less |
$45,106 or less |
|
2 dependents |
$20,359 or less |
$29,546 or less |
$23,414 or less |
$43,356 or less |
$47,692 or less |
|
3 dependents |
$22,710 or less |
$31,897 or less |
$25,765 or less |
$45,707 or less |
$50,278 or less |
|
4 dependents |
$25,061 or less |
$34,248 or less |
$28,116 or less |
$48,058 or less |
$52,864 or less |
|
For each additional dependent, add: |
$2,351 |
$2,351 |
$2,351 |
$2,351 |
$2,351 |
Source: Table prepared by CRS based on information from the Department of Veterans Affairs, https://www.va.gov/healthbenefits/apps/explorer/AnnualIncomeLimits/LegacyVAThresholds?FiscalYear=2020.
Notes: For geographic means test (GMT) variations, see https://www.va.gov/healthbenefits/resources/gmt.
a. The Consolidated Security, Disaster Assistance, and Continuing Appropriations Act, 2009 (P .L. 110–329), provided funding within the medical services account to increase the enrollment of Priority Category 8 veterans whose incomes exceeded the current VA's National Means Test (NMT) and Geographic Means Test (GMT) thresholds by 10% or less. The VA issued regulations and began enrolling these veterans effective June 15, 2009. (Department of Veterans Affairs, "Expansion of Enrollment in the VA Health Care System," 74 Federal Register 22832, May 15, 2009.) Each calendar year, the VA increases the income threshold limit.