Measles Outbreaks, Vaccine Hesitancy, and Federal Policy Options
Changes from May 28, 2019 to June 3, 2019
This page shows textual changes in the document between the two versions indicated in the dates above. Textual matter removed in the later version is indicated with red strikethrough and textual matter added in the later version is indicated with blue.
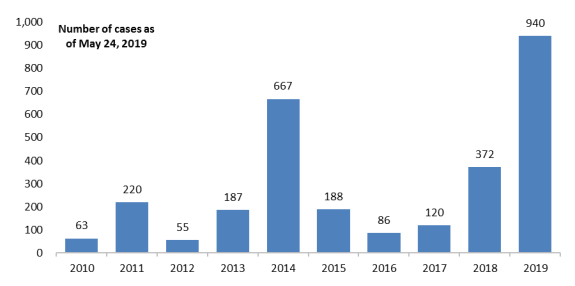
In 2019 to date, 940As of May 31, 2019, 981 cases of measles across 26 U.S. states have been reported to the Centers for Disease Control and Prevention (CDC)—the highest annual number of measles cases in 25 yearssince 1992 (with no deaths reported). Figure 1 shows annual measles cases in the lastpast 10 years.
Measles is a highly contagious viral illness that can lead to pneumonia, encephalitis (infection of the brain), and, rarely, death. Certain groups are at greater risk for complications (e.g., children under 5 and adults over 20 years of age). No specific treatment exists, but it can be prevented with a vaccine.
According to CDC, before a vaccine became available in 1963, there were an estimated 3 million to 4 million annual U.S. measles cases, with an annual average of approximately 48,000 hospitalizations and 400-500 hundred deaths. Widespread vaccination has curtailed ongoing measles transmission. Accordingly, measles was declared eliminated (i.e., no ongoing disease transmission for at least 12 months) in the United States in 2000, and efforts to eliminate measles transmission worldwide (called eradication) continue. Nonetheless, U.S. measles outbreaks are occurring occurring again, principally due to repeated reintroduction from international travelers and an increase in communities with low vaccination rates.
|
Figure 1. Annual U.S. Measles Cases Reported to CDC by States, 2010 |
 |
|
Source: Developed by CRS from CDC, "Measles Cases and Outbreaks," https://www.cdc.gov/measles/cases-outbreaks.html. |
Vaccine Use and Hesitancy
Immunization to measles is provided by a trivalent vaccine that protects against measles, mumps, and rubella using live attenuated (weakened) virus. It is commonly called the "MMR" vaccine. Two formulations are currently licensed (i.e., authorized for marketing) by the U.S. Food and Drug Administration (FDA). Each contains attenuated measles virus along with one or more additional virus types.
The federal Advisory Committee on Immunization Practices (ACIP) makes recommendations for the clinical use of licensed vaccines. In general, the ACIP and CDC recommend two doses of MMR or comparable vaccine for children: the first dose between 12 and 15 months of age, and another between 4 and 6 years of age. The vaccine is not recommended for some children with chronic illnesses, including illnesses that compromise their immune systems.
CDC reports that in 2017, about 91.5% of children aged 19-35 months had received at least one dose of MMR vaccine. Although this coverage seems high, measles is so highly contagious that it may not be sufficient to prevent spread of the disease. A recent model determined that 93%-95% of the population must be vaccinated to prevent measles transmission. This level of immunization in the population would be needed to protect those who cannot be vaccinated (i.e., herd immunity).
To control vaccine-preventable diseases, all states require specified vaccination for students. This exercise of states' police power has been upheld since the Supreme Court decision in Jacobson v. Massachusetts in 1905. All states allow exemptions for medical reasons; 47 states allow them for religious beliefs; and 16 states allow so-called philosophical or "personal belief" exemptions. Implementation of these exemptions varies; some states require a parental affidavit for exemption, or impose movement restrictions on unvaccinated children during outbreaks, for example. Even though state vaccination requirements have long withstood various constitutional challenges, there is a portion of people who consider vaccine mandates to infringe on personal liberty. In addition, a long-standing bioethics principle holds that governments should use the least restrictive means necessary to achieve a public health objective.
Nonmedical exemptions (NME) from vaccine mandates tend to occur in geographic clusters and are associated with higher rates of vaccine preventable disease. High use of NMEs has been linked to vaccine hesitancy—the delay or refusal of vaccines despite their availability. Pediatricians report a rise in vaccine refusals in recent years and added time spent addressing parental concerns. Surveys of parents show the following drivers of vaccine hesitancy: the large number of injections; moral or religious objections; cost or other access problem; lack of information; and concerns about side effects, particularly autism.
Concern that vaccines cause autism is often attributed to a 1998 study suggesting an association of autism with MMR vaccination. The study was later deemed flawed and retracted. Subsequent studies and reviews (such as a meta-analysis involving over one 1 million children and a recent nationwide study in Denmark) have not supported such an association.
Federal Policy Options
The federal government supports immunization in numerous ways, among others, by licensing vaccines shown to be safe and effective; by purchasing or paying for vaccines for low-income children and state immunization programs; by supporting ongoing research and the work of several advisory committees to help guide policy and immunization practices; and by tracking and administering a compensation program for vaccine-associated adverse events.
The federal government currently addresses vaccine hesitancy in several ways. CDC, the Department of Health and Human Services (HHS), and other federal agencies provide educational material for parents, providers, and others. Several federal grants may be used to support multi-component interventions—education combined with incentives, home visits, and reminders—which have proven effective at increasing vaccination rates. Also, CDC supports research into the nature of vaccine hesitancy and the means to overcome it.
The current measles outbreaks have prompted discussions and recent congressional hearings on additional ways that the federal government could address vaccine hesitancy and bolster public trust in vaccines. Among them:
- Conditioning the receipt of federal immunization assistance upon a state's prohibition of NME. Whether such an intervention could be crafted so as to not be overly coercive is not clear.
- Supporting additional counseling time spent by
healthcarehealth care providers, whom parents say are a trusted source of information, through payment policy or other interventions. - Doubling the number of special masters who adjudicate claims for the National Vaccine Injury Compensation Program (VICP), in order to address a claims backlog.
- Continuing/expanding research on vaccine safety and post-market surveillance of vaccine-associated adverse events.
- Strengthening Immunization Information Systems (IIS)—population-based electronic health record (EHR) databases—through enhancing interoperability, standardization, and data sharing. Through IIS, states and CDC can collect real-time data on vaccination coverage, monitor for safety, and implement reminder systems.