Introduction
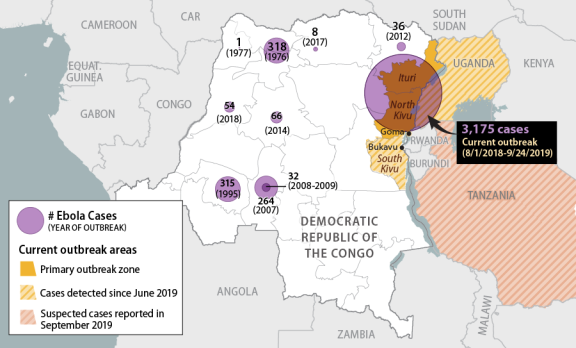
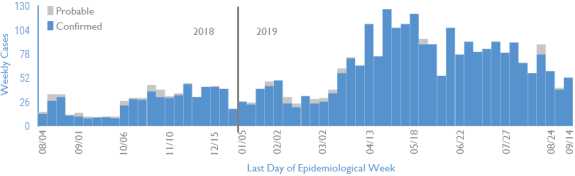
On August 1, 2018, the World Health Organization (WHO) reported a new Ebola outbreak in eastern DRC, about a week after having declared the end of a separate outbreak in the west of the country. As of September 24, 2019, the WHO had reported 3,175 cases in the current outbreak, including 2,119 deaths. About 58% of all cases have been women and 28% children.1 The current outbreak is the 10th on record in DRC, the largest to have occurred in the country, and the second largest ever, after the 2014-2016 Ebola outbreak in West Africa.2 Cases have been concentrated in North Kivu and Ituri provinces (Figure 1), where long-running conflicts had already caused a protracted humanitarian crisis and are complicating Ebola control efforts.3 The number of new Ebola cases identified per week has fluctuated since the start of the outbreak (Figure 2), but has generally trended downward slowly since peaking in April 2019.
 |
|
Sources: CRS graphic. Base map drawn from Esri (2016); data from the WHO, as of September 24, 2019. |
The current outbreak has coincided with a fraught political transition process in DRC. A new president, parliament, provincial-level assemblies, and governors were elected between late 2018 and mid-2019, after years of delays, gridlock, political violence, and repression of opposition voices. Election delays in the Ebola-affected areas, an opposition stronghold, heightened tensions and spurred conspiracy theories, arguably hindering Ebola response. President Felix Tshisekedi, inaugurated in January 2019, was previously an opposition figure, but the coalition of his predecessor Joseph Kabila won supermajorities in parliament and at the provincial level. Observers questioned the legitimacy of the election results, and tense negotiations between the two political blocs (Tshisekedi's and Kabila's) delayed the naming of a new cabinet until late August 2019, while complicating relations between the national and provincial/local officials.4
Several factors have foiled outbreak control efforts, including low Ebola awareness (early symptoms are similar to other common ailments like malaria), community distrust of health interventions, belated visits to health facilities (at which point survival prospects decline rapidly), and infection prevention control lapses in health facilities. Attacks by militia and criminal groups, political protests, health worker strikes, and security force abuses have also disrupted and impeded the response. In mid-September, for example, violent attacks in a new hotspot (Lwemba, Ituri Province) after the death of a local healthcare worker from Ebola prompted the indefinite suspension of Ebola control activities in the area.5 As a result, new cases continue to stem from unknown chains of transmission, and deaths continue to occur outside Ebola treatment centers.
|
Figure 2. Confirmed and Probable Ebola Cases in Eastern DRC, by Week of Onset As of September 14, 2019 |
 |
|
Source: Adapted by CRS from WHO, RD Congo-Ituri et Nord-Kivu: Tableau de bord de l'état de la riposte de la MVE (Semaine 37: du 09 au 15 Septembre 2019), September 20, 2019. Note: Figures in later weeks are subject to delays in case confirmation and reporting, as well as data cleaning. |
U.S. officials and other health experts have repeatedly raised concerns about broader challenges in DRC related to its health care system, political tensions, local grievances, and instability.6 USAID Administrator Mark Green testified to Congress in April 2019 that in DRC, "You have a failed democracy in many, many ways…. It will take more than simply a medical approach. It will take a development approach to try to tackle this terrible disease and to contain its outbreak."7 After traveling to DRC in August 2019, Administrator Green wrote, "Decades of corrupt, authoritarian rule during which communities were denied any meaningful voice in their government have undermined the Congolese people's trust in institutions."8
Health experts have been troubled by reports of Ebola cases in major DRC cities (including the capital of North Kivu, Goma) and outside of DRC. Between June and August 2019, a total of four cross-border cases were detected in Uganda. Observers expressed optimism about the rapid detection and containment of these cases, but new concerns have arisen about subsequent suspected cases in Tanzania. In mid-September, WHO was informed by unofficial sources of a number of suspected Ebola cases in that country, including in the capital city of Dar es Salaam, while Tanzanian authorities asserted that there were no confirmed or suspected Ebola cases in the country.9 WHO has reportedly since sent personal protective equipment (PPE) and vaccination supplies to Tanzania, and recommended that the sickened patients (one of whom reportedly died) receive secondary confirmation testing at a WHO facility. As of September 21, none of the cases had received secondary confirmation. Ebola control in other neighboring countries such as South Sudan, Burundi, or Central Africa Republic, which have minimal state capacity and are affected by protracted conflicts and political crises, could be highly challenging if required.
The International Response
Outbreak control, treatment, and disease surveillance activities are being carried out primarily by DRC government employees (including health workers and frontline workers, who provide routine and essential services), as well as by international nongovernmental organizations, with U.N. agencies (including the WHO), other multilateral entities (including the World Bank), and foreign governments providing funding, expertise, coordination, and logistical assistance.
Classic Ebola outbreak control protocol entails
- infection prevention control (IPC) in health care facilities;
- management and isolation of patients in Ebola Treatment Centers (ETCs);
- fever surveillance with rapid diagnosis;
- tracing of Ebola cases and their contacts; and
- community awareness and adherence to IPC protocols, safe patient and body transport, safe burials, and household and environmental decontamination.
The extraordinary conditions on the ground in affected areas of eastern DRC have limited the effectiveness of conventional control measures, however, and are requiring ever-evolving strategies for containment, including aggressive vaccination campaigns (see text box below). Since the WHO declared the outbreak to be a Public Health Emergency of International Concern (PHEIC) in July 2019, it has sought to garner additional donor funds, as well as international support for addressing the political and security issues affecting Ebola control.
In July 2019, the WHO and the DRC Ministry of Health (MoH) released a fourth strategic response plan to "definitively defeat" the Ebola epidemic (Table 1). The strategic plan is expected to cost over $462 million, including about $288 million for the public health response portion (Table 1). In July 2019, the World Bank announced that it would provide $300 million toward the plan, about half of which would support the public health response, on top of prior funding commitments (discussed below).10
The public health portion of the strategic plan, covering July 1 through December 31, 2019, purportedly takes into account lessons learned from the third strategic response plan (February through July 2019). This portion of the plan is based on
- strengthening political commitment, security, and operational support to improve acceptance of the response and access to insecure areas;
- deepening support for addressing the varied needs of communities affected by Ebola (beyond a single-minded focus on containment efforts), as a means toward fostering community ownership and involvement in Ebola responses;
- improving financial planning, monitoring and reporting; and
- bolstering preparedness of neighboring provinces and countries.
|
Activity |
Cost |
Lead |
Co-Lead |
|
Risk Communication and Community Engagement |
38.3 |
MOH |
UNICEF |
|
Surveillance, Contact Tracing and Vaccination |
42.7 |
MOH |
WHO |
|
Laboratory and Research |
3.2 |
MOH |
WHO |
|
Patient Care, Isolation and Survivors Follow-Up |
54.7 |
MOH |
WHO |
|
Infection, Prevention and Control |
41.6 |
MOH |
WHO & UNICEF |
|
Safe and Dignified Burials |
18.8 |
MOH |
IFRC |
|
Psychosocial Care |
10.4 |
MOH |
UNICEF |
|
Operational Preparedness |
6.1 |
MOH |
WHO |
|
Coordination + Support to Coordination |
71.9 |
MOH |
WB, UNOCHA, and WHO |
|
Public Health Response Total |
287.7 |
||
|
Security, Political Engagement, Operations Support |
11.5 |
||
|
Strengthened Support to Communities |
97.1 |
||
|
Strengthened Preparedness for Surrounding Countries |
66.0 |
||
|
Total Ebola Strategic Response Plan |
462.3 |
||
Sources: DRC Ministry of Health, Strategic Response Plan for the Ebola Virus Disease Outbreak in the Provinces of North Kivu and Ituri, Democratic Republic of Congo, July-December 2019, July 2019; and WHO Health Emergencies Program, Funding Requirements – SRP 4 – Jul to Dec 2019, September 3, 2019.
The World Bank has urged other countries to provide additional support, and the WHO Director-General has urged donors to address disbursement delays. As of September 11, 2019, the WHO had received less than $60 million of the $288 million it sought for the current phase of the public health response.11 The United States is the top country donor for the public health response and has provided almost $158 million for the Ebola humanitarian response, largely supporting activities by nongovernmental organizations (NGOs), as discussed below.
|
Vaccination Strategy During the 2014-2016 West Africa outbreak, Ebola responders deployed an experimental vaccine, rVSV-ZEBOV-GP (produced by Merck). Responders are now using that vaccine to control the DRC outbreak, and the WHO announced on September 23, 2019, that Congolese officials had approved deploying a second vaccine candidate (Ad26.ZEBOV/MVA-BN), developed by Janssen Pharmaceuticals (a subsidiary of Johnson & Johnson) and Bavarian Nordic. The announcement followed a period of controversy in which DRC's then-Minister of Health refused to authorize the Janssen candidate, citing concerns about safety and the potential to undermine community acceptance of Ebola control efforts.12 (The Janssen vaccine requires two doses, while the Merck vaccine requires a single dose.) The DRC Health Minister has since resigned. Both vaccine candidates have been submitted for approval to the U.S. Food and Drug Administration (FDA).13 Two other vaccine candidates are licensed solely in their respective countries of origin: Ad5-EBOV, in China, and GamEvac-Combi, in Russia. During the 2014-2016 West Africa Ebola outbreak, health workers deployed a "ring vaccination" strategy for the first time. This entails vaccinating those who have come in contact with a known Ebola case, as well as their contacts. Health workers have used this strategy in the current outbreak, with some success, but population mobility, suboptimal infection prevention and control practices in local health clinics, gaps in rapid diagnosis and isolation of infected individuals, and resistance by some communities have limited its effectiveness. In February 2019, the WHO Strategic Advisory Group of Experts (SAGE) noted the "exceptional circumstances" of the DRC outbreak and recommended adding geographic-targeted vaccination, entailing vaccinating residents in the area immediately surrounding an Ebola case, such as a village or neighborhood. The SAGE also recommended that "consideration is given to the use of any of [the three] new vaccines to vaccinate health care workers and frontline workers in the neighboring areas where there is a possibility of spread." If a confirmed Ebola case is observed, however, guidance indicates the rVSV-ZEBOV-GP vaccine must be used for a ring or geographic-targeted vaccination in preference to the new vaccine candidates. In May 2019, the WHO SAGE recommended additional adjustments to the vaccine strategy, including
On September 23, 2019—the same day the WHO asserted that "[t]here are enough vaccine doses on the ground to meet the current needs"—Doctors Without Borders called for an independent Ebola vaccination committee to oversee vaccination activities.14 Among other things, the organization asserted that the WHO was limiting the use of vaccines in the field and that at least twice as many people should have been vaccinated to date. As of that date, more than 220,000 people had been vaccinated, including almost 45,000 health workers (HWs) and frontline workers (FLWs).15 Thousands of HWs and FLWs in neighboring countries have also been vaccinated, including 580 in Burundi; 3,000 in Rwanda; 2,974 in South Sudan; and 4,915 in Uganda as of August 24, 2019. |
DRC Government Role
DRC government employees and other Congolese nationals are the primary responders to the Ebola epidemic on the ground. As WHO Executive Director for Health Emergencies Dr. Michael Ryan noted in June 2019, "If you go into the treatment facilities now it is Congolese doctors and nurses in the front line. There may be NGO or WHO badges on the tents but the doctors and nurses are Congolese; surveillance officers are Congolese; 80% of the vaccinators in this response are Congolese."16 The DRC government has provided health workers and administrative personnel, hired local frontline workers, organized volunteers, and conducted information awareness campaigns. The government has also offered certain health services free of charge in selected government health facilities, with donor support (discussed below).
From the start of the current outbreak, the DRC government's health responses were coordinated by the MoH, as in past Ebola outbreaks in DRC. In July 2019, however, President Tshisekedi transferred coordination responsibilities to an expert committee headed by the director of DRC's biomedical research institute, Dr. Jean-Jacques Muyembe, who reports directly to the president. Dr. Muyembe is a recognized expert on Ebola who helped investigate the first known outbreak of the disease, in DRC in 1976. Then-Health Minister Dr. Oly Ilunga resigned following Dr. Muyembe's appointment, citing a dilution of his authority as well as confusion about the coordination of DRC government Ebola responses, an insufficient focus on the health system, and opposition to utilizing the Johnson & Johnson experimental vaccine (see text box above). Ilunga was subsequently the target of scathing criticism in the leaked report of a DRC government investigative commission, which indicated, among other things, that Ilunga and his team had displayed an "aggressive and ostentatious attitude" when visiting the outbreak area and had squandered Ebola response funds on fancy cars and hotel rooms.17 These developments have suggested an internal power struggle over policy and control of funds for Ebola response.
U.N. and Other Multilateral Organizations
Humanitarian experts, including U.S. officials, have repeatedly asserted that broader humanitarian access and security issues have stymied outbreak control efforts, and that international response efforts require increased coordination and transparency.18 In response to such concerns, in May 2019 U.N. Secretary-General António Guterres appointed MONUSCO Deputy Special Representative David Gressly, a U.S. citizen, to serve as a new U.N. Emergency Ebola Response Coordinator charged with establishing a "strengthened coordination and support mechanism" for Ebola response.19 While the WHO is to continue to lead "all health operations and technical support activities to the government," Gressly is leading a broader U.N.-wide effort to strengthen political engagement, financial tracking, humanitarian coordination, and "preparedness and readiness planning" for Goma and surrounding countries.20 Gressly, who continues to report to the head of MONUSCO, portrayed his new role as a reflection of the need for "more than just a public health response."21
The WHO has deployed some 700 personnel to DRC since the current outbreak began. These personnel are coordinating the public health response and providing operational and technical support to DRC government personnel and other actors. Particular areas of focus include detection and rapid isolation of Ebola cases, intensification of rapid multidisciplinary public health actions for Ebola cases, community engagement, and health system strengthening. In addition, the WHO is coordinating regional readiness exercises and assessments in adjacent areas of DRC and neighboring countries. Vaccination and disease surveillance efforts have been bolstered in Uganda, Rwanda, and Burundi.
The World Bank has stepped up its role in supporting the Ebola response effort since mid-2019.22 On July 24, the World Bank Group announced it was mobilizing up to $300 million—to be financed through the Bank's International Development Association and its Crisis Response Window—on top of $100 million disbursed previously through the International Development Association and the Bank's Pandemic Emergency Financing Facility (PEF).23 The PEF announced a further $30 million disbursement for DRC on August 23, 2019.24 World Bank resources have financed free health care and essential medicines in clinics in all affected areas, hazard pay for frontline health workers, handwashing stations, mobile laboratories, decontamination teams, psychosocial support teams, community engagement campaigns, and vaccination efforts. The injection of new resources aims to build on existing World Bank support to strengthen the DRC health system.
The African Union (AU) Africa Centers for Disease Control and Prevention (Africa CDC) has supported international response efforts by deploying members of its voluntary response corps to DRC and neighboring countries. Africa CDC voluntary responders include epidemiologists and anthropologists, as well as communication, laboratory, and logistics experts from various African countries who are "on standby for emergency deployment."25 To date, these responders have trained local health workers and community volunteers, set up laboratories, supplied personal protective equipment, and trained people in port-of-entry screening.
The U.S. Government Response
USAID and the U.S. Centers for Disease Control and Prevention (CDC) deployed staff to DRC and the region when the outbreak was first detected in August 2018. The United States is also the top country donor to the Ebola response effort, as noted above. As of September 10, USAID had announced more than $148 million for direct support to the Ebola response within DRC and another $9.8 million to support preparedness and prevention activities in neighboring countries.26 Those funds were drawn primarily ($156.1 million) from unobligated FY2015 International Disaster Assistance (IDA) funds that Congress appropriated on an emergency basis for Ebola response during the West Africa outbreak (P.L. 113-235). According to USAID, the available balance of FY2015 emergency IDA Ebola funds stood at $105.5 million as of September 9.27
More broadly, the United States is the top bilateral humanitarian donor to DRC and the top financial contributor to MONUSCO, which is providing logistical and security support to Ebola response efforts. USAID Administrator Green testified before Congress in April 2019 that "there is sufficient money for fighting Ebola in DRC," asserting that nonfinancial challenges posed the primary constraint to containment efforts.28 U.S. funding commitments have continued to grow since then, however, as the outbreak has persisted and broadened.
U.S. personnel are providing technical support from Kinshasa, Goma, and neighboring Rwanda and Uganda, while implementing partners (U.N. agencies and NGOs) are administering Ebola response efforts within the outbreak zone with U.S. resources. The Administration has placed strict constraints on the movement of U.S. personnel to and within affected areas, due to security threats. In September 2018, USAID and CDC withdrew personnel from the immediate outbreak zone due to security concerns, despite CDC's stated preference to maintain staff in the field.29
U.S. support for outbreak control has included the following:
USAID has provided grant funding to NGOs and U.N. entities carrying out Ebola response and preparedness activities, drawing primarily on IDA funds (as noted above). In October 2018, USAID deployed a Disaster Assistance Response Team (DART) to coordinate the U.S. response in support of the DRC government, the WHO, and other partners. USAID Ebola response funds have supported disease surveillance, infection prevention and control, safe and dignified burials, water and sanitation aid, prepositioning of medical supplies, humanitarian coordination, and logistics.30 U.S. bilateral economic and health aid funding for DRC has also supported programs that may ease humanitarian access or otherwise complement Ebola response activities.
CDC personnel have provided direct technical support to the DRC government, the WHO, and USAID's DART for disease surveillance, contact tracing, data management, infection protection and control, risk communication and community engagement, laboratory strengthening, emergency management, and surveillance at points of entry. CDC staff also have supported Ebola preparedness efforts in neighboring countries.
The Department of Defense has supplied laboratory training to Ugandan researchers and has partnered with them to conduct clinical Ebola vaccine trials.
Challenges
Security Threats and Political Tensions
Security threats have periodically forced the temporary cessation of Ebola case management in some areas, interrupted contact tracing, and frustrated surveillance efforts in high-transmission areas. Dozens of armed groups are active in the areas most affected by the outbreak. These include an array of local militias, along with the Allied Democratic Forces (ADF), a relatively large and opaque group implicated in attacks on U.N. peacekeepers, local military forces, and civilians.31 Road travel is often dangerous, with frequent reports of militia attacks, armed robbery, and kidnappings.32 In April 2019, the Islamic State claimed responsibility for an attack on local soldiers previously attributed to the ADF, the latest in a series of signs of emerging ties between the two. State security force personnel reportedly maintain ties with armed groups and have been implicated in atrocities, including civilian massacres in Beni territory since 2014.33
Local mistrust of government officials and outsiders (including Congolese who are not from the immediate area)—sometimes rooted in conflict dynamics, ethnic tensions, and political friction—has prompted some community resistance to Ebola control efforts and led to attacks on health workers and facilities, including Ebola treatment centers. Some communities in Beni and Butembo have long opposed DRC's central government and complained of neglect and persecution. WHO officials have urged broader international support for "political mediation, engagement with opposition, and negotiated solutions," asserting that "[j]ust purely focusing on community engagement and participation will not fix what are deep seated political issues that need to be addressed at a higher level."34
Perceptions that outsiders are profiting financially from the outbreak, or that international intervention is driven more by fear of contagion than concern for locals' wellbeing, appear to have fueled conspiracy theories and community resistance. At a July 15 donors event on Ebola response in Geneva, WHO Director-General Dr. Tedros Adhanom Ghabreyesusi said that Congolese in the outbreak zone had asked him, "Are you here to help us, or to prevent this thing from coming to you? Are you doing this for us, or for yourself?" He added, "It embarrasses me.… We should not appear to be seen as if we are parachuting in and out because of Ebola."35 DRC's then-Health Minister argued in the same meeting that local perceptions that the response was bringing cash into the region had fueled threats to health workers, including kidnappings.
Health System Constraints
Local perceptions that donors are more concerned with preventing the spread of Ebola to their countries than with helping Congolese communities are rooted, in part, in enduring health challenges. Maternal and infant deaths, for example, have for years regularly exceeded the current count of Ebola deaths but have received comparatively little attention. Authorities have redirected health resources in some areas for Ebola control, deepening local frustrations. Vaccination campaigns have also been interrupted in some Ebola hotspots. In Ituri province, for example, inadequate supply of measles vaccine has limited containment of a measles outbreak that began in January and has infected over 161,000 people, claiming over 3,000 lives.36 Health workers also are fighting a cholera outbreak that has infected over 15,000 people and killed at least 287.37
The WHO has reported that Ebola transmission is likely occurring in ill-equipped and understaffed health facilities. Inconsistent adherence to infection prevention and control, periodic disruptions in supply chain systems, and limited access to water for handwashing in some health facilities have complicated Ebola control efforts. In addition, some health workers have refused to wear personal protective equipment in health facilities or perform rudimentary infection prevention and control measures due to threats of violence by some members of the community.38 As of August 27, 2019, 156 health workers had contracted Ebola, at least 34 of whom had died.39 The MoH, WHO, and other partners have identified health facilities of concern and are addressing lapses in triage, case detection, and infection prevention and control.
Reported Progress
Community Engagement. The WHO and implementing partners have worked to deepen local engagement, with some reported positive results. Local Ebola committees in Butembo and Katwa (at the center of the outbreak zone in North Kivu), for example, are chaired and managed by community members who plan Ebola awareness and sensitization campaigns.40 Improved community engagement has reportedly contributed to increased participation in vaccine campaigns and safe and dignified burial practices. For example, the WHO reported in July 2019 that a high-risk contact in Katwa had sought vaccination and offered to bring other contacts.41 In an effort to reduce the risk of transmission and broaden access to Ebola treatment and case finding, the WHO also plans to establish smaller patient transit centers closer to communities. Replicating engagement activities in emergent hot spots remains a challenge, however.42
Ebola Therapeutics Advance. In August 2019, a clinical trial of four investigational Ebola treatments in DRC identified two "strong performers," leading the WHO to state that "these are the only drugs that future patients will be treated with."43 The trial, launched in late 2018, was co-sponsored by DRC's national biomedical research institute and the U.S. National Institutes of Health, and was carried out by an international research consortium coordinated by the WHO.44
Issues for Congress
U.S. Funding for DRC Ebola Response
In FY2015, in the context of the West Africa outbreak, Congress appropriated $5.1 billion for Ebola response and preparedness on an emergency basis, including $1.436 billion in multiyear International Disaster Assistance (IDA) funds (Title IX of Division J, P.L. 113-235). U.S. funding for responding to the current outbreak has drawn primarily on the unobligated balance of these IDA funds. According to USAID, $105.5 million of these funds remained available for expenditure as of September 9, 2019.45 Should the outbreak continue or expand in new ways, Congress may consider what funding mechanisms, if any, the United States might use to support Ebola control. At the same time, the United States remains the lead country donor to the current Ebola response effort. Members may examine the U.S. role, vis-à-vis other actors (including other countries, multilateral entities, and private sources), in financing Ebola response activities, and may debate strategies for securing additional contributions from other donors.
U.S. Aid Restrictions Related to Trafficking in Persons
DRC is ranked as "Tier III" (worst) under the Trafficking Victims Protection Act (TVPA, P.L. 106-386, as amended), which triggers prohibitions on certain types of U.S. aid absent a full or partial presidential waiver. In FY2019, in a departure from previous practice, President Trump did not partially waive the restrictions for DRC.46 Thus, pursuant to the TVPA, no "nonhumanitarian, nontrade-related" assistance may be provided "to the government" of DRC.47
IDA funds, the core source of funding for U.S. Ebola response support to date, are exempt from the TVPA restrictions (22 U.S.C. §7102[10]). The TVPA further exempts economic and development assistance "in support of programs of nongovernmental organizations." In practice, the Administration has interpreted the TVPA restrictions to apply broadly to various programs funded through the Development Assistance (DA) and Economic Support Fund (ESF) accounts, including some that would be implemented by NGOs, though it has not publicly provided a full account of affected activities. Some Members of Congress have expressed concern that some U.S. assistance that could help promote humanitarian access in Ebola-affected areas has been held up as a result.48 Testifying before the Senate in July 2019, a senior USAID official affirmed that some FY2018 aid resources that could help with Ebola control remained restricted in connection with the TVPA, but he and other Administration witnesses did not provide further details.49
Two bills introduced in the 116th Congress (S. 1340, the Ebola Eradication Act of 2019, and H.R. 3085, a House companion bill) would authorize assistance for a range of activities that could help lower community resistance or otherwise support Ebola control efforts in DRC and neighboring states, "notwithstanding" the TVPA restrictions. S. 1340 passed the Senate on September 23, 2019. Similar language was included in a draft FY2020 State, Foreign Operations Appropriations bill circulated by the Senate Appropriations Committee on September 18, 2019. That bill would also broadly provide at least $298.3 million in U.S. bilateral assistance for "stabilization, global health, and bilateral economic assistance" to DRC—slightly higher than the U.S. allocation for DRC in recent years, not counting food aid—"including in areas affected by, and at risk from, the Ebola virus disease."
Global Health Security
The current Ebola outbreak has prompted resumption of discussions about strengthening health systems worldwide, particularly with regard to pandemic preparedness. In 2014, during the Obama Administration, the United States and the WHO co-launched the Global Health Security Agenda (GHSA) to improve countries' ability to prevent, detect, and respond to infectious disease threats.50 The United States, the largest donor to this multilateral effort, pledged to support it with $1 billion from FY2015 through FY2019. The Trump Administration has built on these efforts. In May 2019, the White House released the United States Government Global Health Security Strategy, which outlined the U.S. role in extending the Global Health Security Agenda and improving global health security worldwide.51 Although the Trump Administration, through the strategy and public statements, has supported extending the GHSA through 2024, officials have not provided comprehensive information on what that support would entail.
Members of Congress may continue to debate what role, if any, the United States should play in supporting global health system strengthening efforts to bolster global health security, and whether to adjust funding levels to meet ongoing and future infectious disease threats. Through regular appropriations, disease outbreak prevention and global health security efforts are funded through USAID pandemic influenza and CDC global health protection line items (Table 2).
|
FY2015 Enacted |
FY2016 Enacted |
FY2017 Enacted |
FY2018 Enacted |
FY2019 Enacted |
FY2020 Request |
|
|
CDC |
55.1 |
55.1 |
55.1 |
108.2 |
108.2 |
100.0 |
|
USAID |
72.5 |
72.5 |
72.5 |
72.5 |
100.0 |
90.0 |
Source: Created by CRS from appropriations legislation and congressional budget justifications.
Note: Excludes emergency Ebola appropriations.
On September 19, 2019, the House passed the Continuing Appropriations Act, 2020, and Health Extenders Act of 2019 (H.R. 4378), which would authorize the transfer to the CDC of up to $20 million for Ebola preparedness and response activities from the Infectious Disease Rapid Response Reserve Fund.52 Other relevant bills introduced in the 116th Congress include H.R. 2166, which would codify U.S. engagement in the GHSA as specified in an executive order issued by the Obama Administration,53 and H.R. 826, which seeks to facilitate research and treatment of neglected tropical diseases, including Ebola.