Introduction
End-stage renal disease (ESRD) is the final stage of chronic kidney disease (CKD), which is the gradual decrease of kidney function over time. Individuals with ESRD have substantial and permanent loss of kidney function and require a regular course of dialysis (a process that removes harmful waste products from an individual's bloodstream) or a kidney transplant to survive.
In 1972, Congress enacted legislation allowing qualified individuals with ESRD under the age of 65 to enroll in the federal Medicare health care program (Social Security Amendments of 1972; P.L. 92-603).1 The legislation marked the first time that individuals were allowed to enroll in Medicare based on a specific medical condition rather than on the basis of age. In the years since the legislation was enacted, Medicare has become the main source of health care coverage for individuals with ESRD.
Medicare benefits for ESRD beneficiaries, including those under the age of 65 who qualify based on the disease, include thrice-weekly dialysis treatments and coverage for kidney transplant. There is an initial waiting period for coverage for ESRD patients under the age of 65, and coverage for such enrollees terminates 12 months after a patient ends dialysis or after 36 months of follow-up care (including immunosuppressive medications) after a kidney transplant.2 Many Medicare beneficiaries with ESRD also require Medicare services to treat related, chronic health conditions, such as diabetes and heart disease. Because Medicare beneficiaries with ESRD have higher-than-average health care costs, they account for about 7% of Medicare fee-for-service (FFS) spending, while making up about 1% of program enrollment (FFS and managed care combined). In total, FFS Medicare covers three-fourths of U.S. annual medical spending to treat ESRD.3
Over the years, Congress has enacted a number of changes to Medicare ESRD benefits in an effort to improve the quality of services and control program costs. For example, the Medicare Improvements for Patients and Providers Act of 2008 (MIPPA; P.L. 110-275) imposed a "bundled" payment system for dialysis providers, which took effect in 2011. (See "Medicare Reimbursement for ESRD Services.") The 21st Century Cures Act (CURES Act; P.L. 114-255), enacted in 2016, will allow Medicare-eligible individuals with ESRD to enroll in Medicare Part C private managed care plans, beginning in 2021. (See "Medicare Advantage Enrollment.")
This report provides background on the ESRD Medicare benefit, including information about the disease, Medicare enrollment criteria, other health care coverage for ESRD, and Medicare reimbursement policy. The report concludes with a discussion of outstanding payment and coverage issues in ESRD care.
ESRD Progression and Treatment
As noted above, ESRD is the final stage of CKD and is defined as a substantial and irreversible failure of kidney function. Individuals with ESRD suffer from a buildup of fluid and waste products in their bodies because their kidneys can no longer filter blood and perform other essential functions.4 The condition is fatal without treatment. (See "Main Treatments for ESRD.") The two leading medical conditions that can affect kidney function and contribute to ESRD are diabetes and high blood pressure. Other illnesses that can contribute to kidney failure include heart disease, autoimmune conditions, genetic diseases, and kidney disorders.5
ESRD differs from acute kidney injury (AKI), where the kidneys cease to function over a short period, such as a matter of days. AKI can be caused by a heart attack or drug abuse, for example, and can be temporary. Medicare covers some services for AKI patients through its ESRD provider payment system.6 (See "Acute Kidney Injury.")
ESRD Prevalence and Incidence
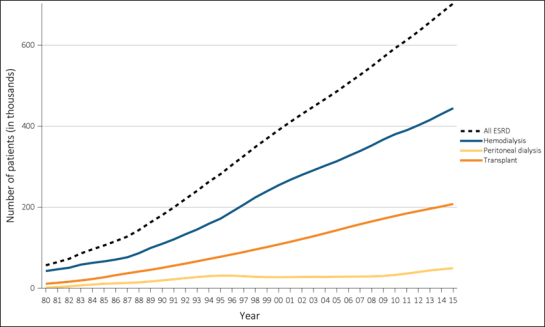
According to the United States Renal Data System, 703,243 Americans were receiving treatment for ESRD in 2015, compared to 56,434 receiving treatment in 1980.7 Those figures refer to the prevalence of ESRD, which is the total number of people receiving treatment for the disease. (See Figure 1.) In 2015, 124,114 patients were being newly treated for ESRD, which is known as the incidence of ESRD; in 1980, 17,903 patients were being newly treated.8
The ESRD incidence rate—the number of people being newly treated for ESRD within a set population—is higher among certain racial and ethnic groups, including Native Hawaiians/Pacific Islanders, African Americans, and Hispanics, than among whites. However, since 2000, there has been a significant reduction in the excess risk of developing ESRD among minority populations.9 Researchers have identified socioeconomic and biological factors that may contribute to the racial disparities in development and treatment of ESRD.10
|
Figure 1. End-Stage Renal Disease (ESRD) Patients in the United States Number of new ESRD patients and total ESRD patients, 1980-2015 |
 |
|
Source: United States Renal Data System, Tables 1.1 and 1.3 in Annual Data Report 2017, vol. 2, at https://www.usrds.org/2017/view/v2_09.aspx. Hereinafter United States Renal Data System, Annual Data Report 2017. Notes: Figure is based on unadjusted incidence and prevalence data. Incidence refers to the number of people being newly treated for ESRD each year; prevalence refers to the total number of people receiving ESRD treatment. Because prevalence reflects both the incidence and the course of the disease, the continued increase in ESRD prevalence trends could reflect not only newly incident cases but also longer survival of ESRD patients, according to the United States Renal Data System. |
Main Treatments for ESRD
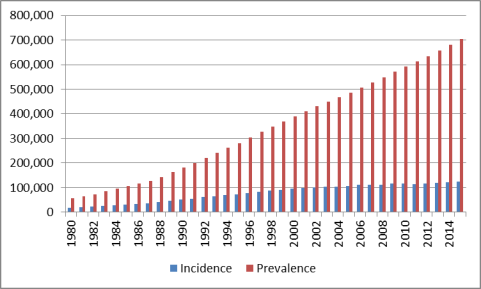
The main treatments for ESRD are kidney transplant and dialysis. At the close of 2015, 63% of prevalent ESRD patients were receiving hemodialysis, 7% were being treated with peritoneal dialysis, and 30% had been treated with a functioning kidney transplant.11 (See Figure 2.)
Kidney Transplant
In a transplant, an individual receives a healthy donor kidney from a living volunteer or a deceased person. The donor kidney usually is positioned in a patient's lower abdomen, and the failed kidneys may be left in place unless they pose a threat of infection or other complications.12 Individuals who undergo successful transplants usually must take immunosuppressive drugs for the rest of their lives to minimize the risk that their bodies will reject the donor kidneys. (See "Medicare Coverage of Immunosuppressive Drugs.")
Although a kidney transplant is the preferred treatment for ESRD, it is not the most common treatment. Some individuals may not meet medical qualifications for a transplant.13 Even people who are prime candidates for a transplant may have difficulty obtaining one due to a severe shortage of donor kidneys. As of June 2018, there were 95,091 people on the waiting list for a kidney transplant. The waiting list is maintained by the United Network for Organ Sharing.14
Dialysis
Dialysis refers to the process of filtering an individual's blood with a solution known as a dialysate to remove harmful wastes, salt, and water—a process that otherwise would be performed by functioning kidneys.15 Dialysis also helps to control blood pressure and the levels of other chemicals in the blood. Dialysis does not cure ESRD, and it carries other health risks. However, many people undergoing dialysis are able to carry on a range of normal activities. Dialysis usually is started when an individual has lost 85%-90% of kidney function. Average life expectancy for an individual requiring dialysis is 5-10 years, although people can live far longer.16
There are two main types of dialysis, as described below.
Hemodialysis
Hemodialysis is the most common form of dialysis.17 In hemodialysis, an external machine acts as an artificial kidney (dialyzer). Blood is removed from the body through a system of tubes, with access usually through a vein in an arm, and is filtered and replaced. Hemodialysis typically lasts four hours at a time and is performed three times a week at a dialysis center. A form of hemodialysis can be carried out by a patient in his or her home. Home hemodialysis may involve more frequent and longer sessions and can include nocturnal treatments.
Peritoneal Dialysis
In peritoneal dialysis, a patient's blood is cleaned inside his or her body, using a catheter inserted into the abdominal cavity.18 Dialysis solution flows through the catheter into a patient's belly to absorb wastes and other fluids. After a few hours, the solution and wastes are drained. This type of dialysis may be performed at home or other clean, private locations outside of a dialysis center. Peritoneal dialysis may work better for certain populations that may not be able to tolerate hemodialysis, such as children or elderly patients with heart disease.19
Other Treatments
Medicare covers other ESRD treatments, including hemofiltration, which uses hollow artificial membranes to remove fluid and toxic substances from the blood. According to CMS, the procedure may be covered three times a week. Another Medicare-covered treatment is ultrafiltration, which removes excess fluid from the blood by exerting pressure on a dialysis membrane. Ultrafiltration does not substitute for dialysis and is used when excess fluid cannot be removed easily during regular hemodialysis.20
Medicare Coverage of ESRD
Social Security Amendments of 1972
Modern dialysis was developed in the 1940s, and the first successful kidney transplants took place during the 1950s.21 ESRD patients initially had difficulty obtaining the new treatments because of cost and limited availability. In one example, Seattle's King County Medical Society in the early 1960s appointed a special panel of laypersons to allocate the limited number of dialysis slots in that area.22
In 1965, Congress established the Medicare program under Title XVIII of the Social Security Act to provide health coverage to citizens or permanent residents of the United States who are at least 65 years of age and who have met certain work requirements.23 In the Social Security Amendments of 1972, Congress expanded Medicare eligibility to include (1) individuals receiving Social Security Disability Insurance benefits and (2) qualified individuals diagnosed with ESRD.24
Under the 1972 legislation, as amended, an individual under 65 years of age who is medically determined to have ESRD and who is undergoing treatment is eligible to enroll in Medicare if he or she has worked in Social Security-covered employment for a minimum number of quarters or is entitled to an annuity under the Railroad Retirement Act.25 Beneficiaries who qualify for Medicare on the basis of ESRD are eligible for premium-free Medicare Part A and may enroll in Part B.26 For these beneficiaries, there is a waiting period for Medicare services. (See "Waiting Periods and Time Limits for Medicare Based on ESRD.") If an individual has an insufficient work history, he or she may be able to qualify for Medicare based on the work history of a spouse, parent, or guardian, which makes ESRD coverage available to people of all ages. The 1972 law was the first time individuals of all ages were made eligible for Medicare based on a categorical disease.27
|
Medicare Benefit Structure The Social Security Amendments of 1972 did not create a new end-stage renal disease (ESRD) program; rather, they allowed qualified ESRD patients to enroll in Medicare. Medicare currently has four distinct parts: Medicare Part A (Hospital Insurance), Part B (Supplementary Medical Insurance), Part C (Medicare Advantage, or MA), and Part D (outpatient prescription drugs). In general, under Medicare
Source: For updated annual figures on deductibles, premiums, and other cost sharing, see CRS Report R40425, Medicare Primer and CRS Report R40611, Medicare Part D Prescription Drug Benefit. Notes: For Medicare Part A, a spell of illness, also referred to as the benefit period, begins when a beneficiary is admitted for inpatient hospital services and ends after 60 consecutive days in which the beneficiary was neither an inpatient of a hospital nor a resident of a skilled nursing facility. See SSA §1861(a). |
Medicare ESRD Enrollment Statistics
Figure 3 illustrates the Medicare status of the ESRD point-prevalent population (the total number of patients in active treatment for ESRD at set date in the year) from 2004 to 2015. Of the ESRD prevalent patients in the United States as of December 31, 2015, about 59% had Medicare as their primary payer (including individuals dually eligible for Medicare and Medicaid), 8% had Medicare as a secondary payer, 14% were in Part C MA plans, and 19% had non-Medicare coverage (including those pre- and post-Medicare coverage).28 Required enrollee cost sharing for ESRD-related services, and the scope of the covered services, vary depending on the specific health plan and the type of services required. Likewise, reimbursement to Medicare and private providers varies among health plans.
|
Figure 3. Types of Coverage for Individuals with ESRD in 2015 |
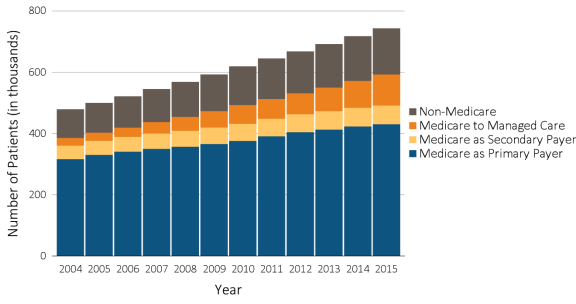 |
|
Sources: United States Renal Data System, Annual Data Report 2017, Table 9.3. Data from the Medicare Enrollment Database (EDB) and dialysis claims information were used to categorize payer status as Medicare as primary payer, Medicare as secondary payer, Medicare Advantage managed care plans, or non-Medicare. Notes: Data are based on ESRD point-prevalance figures as of December 31, 2015. Beneficiaries enrolled in Medicare may have secondary sources of coverage, such as Medigap or Medicaid. Medicare Secondary Payer refers to individuals who qualify for Medicare based on ESRD, but are covered by employer-sponsored insurance, which acts as the primary payer for ESRD services for a set period of time (see "Employer-Sponsored Health Plans"). Non-Medicare patients include patients who were pre- or post-Medicare entitlement, including patients in the three-month waiting period for ESRD services. |
Medicare spends far more on medical services for beneficiaries with ESRD than for other beneficiaries. In 2013, Medicare spent $61,996 per ESRD beneficiary, compared to $9,889 per non-ESRD beneficiary.29 Medicare per-capita spending for all beneficiaries was $10,478 in 2013, the most recent data available.
Medicare-Covered Services for Treatment of ESRD
Individuals who become eligible for Medicare on the basis of ESRD are eligible for all Medicare-covered items and services, not just those related to ESRD. Medicare enrollees incur routine out-of-pocket costs, including co-payments and deductibles, if they do not have supplemental coverage that wraps around Medicare.
In addition to other Medicare-covered health care, ESRD-related services include the following:
- Medicare Part A coverage of inpatient services in an approved hospital for covered kidney transplants, as well as the cost of care for a kidney donor. Part A also will cover inpatient dialysis for patients admitted to a hospital or skilled nursing facility for special care.30 (See "Kidney Transplant.")
- Medicare Part B coverage for doctors' services during a kidney transplant; dialysis treatments in Medicare-certified outpatient facilities, such as freestanding dialysis centers or outpatient centers in hospitals; and related services, such as patient training in a certified dialysis facility or a beneficiary's home. Part B also provides coverage of immunosuppressive drugs for individuals who have had a Medicare-covered kidney transplant and of specified drugs, such as erythropoiesis-stimulating agents used to treat anemia. In addition, Part B covers other drugs administered by a physician.31 Individuals who qualify for Medicare on the basis of ESRD but delay enrolling in Part B must pay a late-enrollment penalty. 32 However, individuals who initially qualified for Medicare based on age or disability but delayed enrolling in Part B or stopped Part B payments may enroll if they are later diagnosed with ESRD and have any late-enrollment penalty removed.33
- Medicare Part C is available to ESRD patients only in limited circumstances, such as when an individual already was enrolled in a MA plan at the time of an ESRD diagnosis. The CURES Act (P.L. 114-255) will allow people already diagnosed with ESRD to enroll in Medicare Part C plans, beginning in 2021. (See "Medicare Advantage Enrollment.")
- Medicare Part D provides coverage for outpatient prescription drugs filled at a pharmacy, including many oral medications used by ESRD patients and prescription medications for related conditions, such as high blood pressure. In 2016, about 90% of ESRD patients undergoing dialysis in fee-for-service Medicare had Part D or other sources of drug coverage that were at least as comprehensive as Part D.34
Waiting Periods and Time Limits for Medicare Based on ESRD
The exact point at which an individual who qualifies for Medicare based on ESRD becomes eligible for covered services varies depending on the type of treatment needed and whether the person has other health care coverage. As noted, Medicare also imposes time limits on coverage for individuals under the age of 65 who end dialysis or who undergo a successful kidney transplant.
Waiting Periods
Medicare waiting periods for coverage of services begin at the point of an individual's ESRD treatment or diagnosis—whether or not an individual has qualified for Medicare already.35 If an individual under the age of 65 is eligible for Medicare based on ESRD but does not enroll immediately, the individual may qualify for up to 12 months of retroactive coverage, once he or she enrolls.36
In general, beneficiaries who qualify for Medicare based on ESRD
- Are eligible for Medicare coverage beginning on the first day of the fourth month of dialysis treatment if they are receiving dialysis treatments in a certified outpatient facility.37
- May be eligible for benefits as early as their first month of eligibility if they take part in a home dialysis training program in a Medicare-approved training facility, begin home dialysis training before the third month of dialysis, and expect to finish home dialysis training and give self-dialysis treatments.38
- Are eligible for coverage during their first month of Medicare eligibility if they are admitted to a Medicare-approved hospital to undergo a kidney transplant. Patients may be eligible for Medicare two months prior to a kidney transplant provided they are hospitalized in a Medicare-approved hospital in preparation for the transplant.
Time Limits
Medicare entitlement for an enrollee that is based solely on ESRD ends when the enrollee is no longer considered in the "end stage" of kidney disease. A beneficiary is no longer end stage when dialysis has been stopped for 12 months or a kidney transplant has been successful for 36 months. If a patient's kidney transplant later fails, the individual is entitled to Part A and eligible to enroll in Part B in the month that he or she starts a new course of dialysis. Likewise, if an ESRD patient ends a course of dialysis but later needs to resume dialysis treatments, he or she would be entitled to Part A and eligible to enroll under Part B in the month when a regular course of dialysis is resumed.39
Other Health Coverage for ESRD Patients
Medicare beneficiaries with ESRD have comprehensive coverage but still can face significant out-of-pocket costs for such things as prescription drug co-payments, annual deductibles, and cost sharing for dialysis visits and hospital care. Some ESRD beneficiaries may purchase supplemental health care coverage, such as Medigap policies, to help cover some of these costs. Other patients may have been covered by an employer-sponsored health plan prior to their ESRD diagnosis or may qualify for other federal health benefits, such as Medicaid. In addition, ESRD patients under the age of 65 may choose to enroll in individual health care plans rather than in Medicare. Medicare may limit or prohibit ESRD-related benefits for individuals who have other health care coverage. This section will outline sources of supplemental or alternative coverage for ESRD patients and associated regulations that affect Medicare payments.
Employer-Sponsored Health Plans
Individuals who are diagnosed with ESRD may already have health care coverage through an employer-sponsored health insurance plan, including a retiree health plan. If an individual is not already enrolled in Medicare on the basis of age or disability at the time of his or her ESRD diagnosis, and is covered through a commercial group health plan, the individual continues to receive primary ESRD and other health coverage through the commercial health plan for 30 months after qualifying for Medicare.40 During the coordination period, if an individual enrolls in Medicare, the program acts as the secondary payer, meaning that Medicare may be billed for covered ESRD services and other health care services that are not fully reimbursed by the group health plan. After 30 months, Medicare becomes the primary payer. Group health plans may not impose higher costs or place limits on services to ESRD patients during the coordination period that differ from those provided to other enrollees.41
Individuals with ESRD who have group health coverage may delay enrolling in Medicare Parts A and B during the 30-month coordination in order to avoid paying Part B premiums. Under Medicare rules, individuals with ESRD who delay signing up for Medicare Parts A and B until the end of the 30-month coordination period will not face a Part B late enrollment penalty. However, the individuals would not have secondary Medicare coverage for out-of-pocket expenses related to their medical care.42 In addition, if an ESRD patient signs up for Part A, but not for Part B prior to the end of the coordination period, the individual subsequently will be allowed to enroll in Part B only during the annual Medicare open enrollment period (January 1-March 31), with coverage effective the following July. Depending on timing, the delay in signup could result in a Part B late enrollment surcharge for some ESRD beneficiaries.43
Further, an ESRD patient who does not enroll in Medicare Parts A and B before the end of the 30-month coordination period could face a gap in coverage. When Medicare becomes the primary payer at the end of the 30-month coordination period, a group health plan may reduce ESRD-related coverage for the Medicare-eligible enrollee (but otherwise may not differentiate between the ESRD enrollees and other group health plan enrollees).44
If an ESRD beneficiary with group health coverage was enrolled in Medicare based on ESRD and Medicare enrollment lapsed due to termination of dialysis or a successful kidney transplant, the individual could re-enroll in Medicare and would be subject to another 30-month coordination period.45
Medicaid ESRD Coverage
According to a recent report, 42% of Medicare ESRD patients also are enrolled in Medicaid. Medicaid is a joint federal-state program that finances the delivery of primary and acute medical services, as well as long-term services and supports (LTSS), to a diverse, low-income population, including children, pregnant women, adults, individuals with disabilities, and people aged 65 and older.46
Individuals who qualify for both Medicare and Medicaid are known as dual-eligible individuals. In total, ESRD beneficiaries make up about 1% of total Medicare enrollment and 2.4% of dual-eligible enrollment.47
For dual eligibles, Medicare is the primary payer and Medicaid is the payer of last resort. For example, dual eligibles with ESRD receive hospital care, physician services, dialysis treatments, prescription drugs, and other health care services through Medicare. Medicaid provides assistance with some or all Medicare premiums and cost sharing, and it covers services such as long-term care not provided by Medicare. The exact level of Medicaid benefits provided to dual eligibles varies based on beneficiary income and other criteria.48 Dual eligibles who qualify for both Medicare and Medicaid and are already enrolled in Medicaid (but not Medicare) at the time of an ESRD diagnosis have Medicaid as their primary payer during any three-month Medicare waiting period.
The per person Medicare annual cost for treating a dual eligible with ESRD was $77,785 in 2013, compared to the $16,636 cost of treating a dual eligible who did not have ESRD.49
Medicare Supplemental Health Insurance (Medigap)
Medicare beneficiaries aged 65 and older have the opportunity to buy private Medigap policies to cover expenses not paid by Medicare, such as deductibles, coinsurance, and co-payments.50 Medigap products are regulated jointly by the states and the federal government. Federal law establishes a six-month Medigap open enrollment period, beginning on the first day of the first month that an individual is both at least aged 65 and enrolled in Medicare Part B. During this open enrollment period, insurers cannot (1) refuse to sell qualified individuals any Medigap policy the insurer offers; (2) base an individual's policy premiums on his or her health conditions; or (3) impose a waiting period, among other protections. 51
There is no general federal requirement that insurers sell Medigap plans to Medicare beneficiaries under the age of 65 who qualify for Medicare based on disability, including those with ESRD. However, more than 30 states require insurers to offer at least one type of Medigap policy to individuals under the age of 65.52 Some insurers voluntarily sell Medigap plans to younger Medicare enrollees, even when there is no state requirement to do so. If permitted by state law, insurers may use medical underwriting and charge higher premiums for Medigap plans when selling to those under the age of 65, which could make the plans very expensive for younger ESRD patients.
Commercial Health Insurance Plans in the Individual Market
The Patient Protection and Affordable Care Act (ACA; P.L. 111-148, as amended) imposed a number of federal requirements on health plans offered in the private insurance market—particularly the individual market (also known as the non-group market).53 These requirements made private insurance in the individual market more accessible for individuals with preexisting conditions.
Following are the main ACA provisions that affect the scope and cost of private health care coverage for ESRD patients in the individual market:
- Plans are prohibited from basing eligibility and premiums on health-related factors or denying benefits based on health conditions.54
- Health insurance exchanges must be in operation in every state, providing a marketplace where individuals can shop for private insurance coverage.55 Individuals purchasing coverage through the individual exchanges may be eligible to receive financial assistance. Eligibility for such assistance is based on income and provided in the form of premium tax credits and cost-sharing subsidies.56
- Most plans offered in the individual market (both inside and outside the individual exchanges) must offer a core package of health services, known as the essential health benefits (EHB).57 Each state's EHB package is based on a single reference insurance plan (i.e., the EHB benchmark plan) sold in the state, and there is considerable variation among states in the specific benefits that are included. EHBs also may change over time.58 For the 2018 coverage year, 49 states and the District of Columbia include dialysis as an EHB.59
- Consumer cost sharing is capped for services included in the EHB package. The cap, adjusted annually, applies to providers that participate in a health plan's contracted network, which can include dialysis facilities. For 2018, the cost-sharing limit is $7,350 for an individual plan and $14,700 for a family plan.60
- Plans generally are prohibited from setting limits on how much they spend for covered EHBs either during the entire period an individual is enrolled in the plan (lifetime limits) or during a plan year (annual limits). Plans are permitted to place lifetime and annual limits on covered benefits that are not considered EHBs, to the extent that such limits are permitted by federal and state law.67
Insurers may not sell individual market policies to individuals who are entitled to benefits under Medicare Part A or who are enrolled under Part B, knowing that the policies would duplicate their Medicare benefits.61 At the same time, however, there is no requirement that ESRD patients who qualify for Medicare enroll in the Medicare program. Individuals with ESRD who are eligible for Medicare but who have not enrolled may choose to buy an individual market plan instead (either on or off the exchanges). Further, individuals with ESRD may sign up for coverage through the individual exchanges and may be eligible for financial assistance (i.e., premium tax credits and cost-sharing subsidies) available through the individual exchanges.62
Eligibility for financial assistance through the individual exchanges ends if an ESRD patient enrolled in an individual market exchange plan subsequently secures Medicare coverage.63 An individual who is eligible for Medicare but who delays enrolling in the program in order to buy an individual market plan could be subject to a Part B late-enrollment penalty if he or she later ends exchange coverage and signs up for Medicare.
CMS Proposed Regulations Regarding Premium Subsidies
Since the ACA market reforms took effect in 2014, dialysis providers and nonprofit groups that receive donations from dialysis firms have provided premium assistance and other cost-sharing subsidies to ESRD patients who enroll in individual plans in the private market.
According to the Centers for Medicare & Medicaid Services (CMS), the number of ESRD patients enrolled in individual market commercial plans doubled between 2014 and 2015 and increased as much as fivefold in some states over that period. CMS expressed concern that dialysis facilities and nonprofit organizations supported by dialysis firms were using premium and other assistance for "the inappropriate 'steering' of individuals eligible for or entitled to Medicare or Medicaid into individual market plans" so that the providers could bill at higher rates than were allowed under Medicare. Specific concerns noted by CMS included the following:
- Some third-party payers discontinued premium assistance for ESRD patients if the patients received a kidney transplant, creating a potential loss in insurance coverage for such individuals. The policy of ending premium assistance upon receipt of a transplant also could make it harder for patients to qualify for a transplant, because health care providers require proof that a patient will have insurance coverage after a transplant to cover the cost of immunosuppressive drugs and other related health expenses.
- ESRD patients who accepted premium assistance to enroll in private health plans were not always informed that private insurers could refuse to accept the third-party assistance, possibly exposing the patients to a loss of coverage during a plan year.
In December 2016, CMS issued a final interim rule to provide additional protections to patients with ESRD who received premium support to enroll in private health care plans rather than in Medicare.64 Under the rule, ESRD patients receiving premium support from dialysis providers—either directly or through a third party—would have had a right to comprehensive information about their health care options, comparative costs of coverage under Medicare and other health care plans, and information about the providers' contributions to third parties subsidizing the patients' premiums. In addition, dialysis providers and third-party entities providing premium assistance to ESRD patients would have had to inform enrolling health care plans of their assistance and receive assurances from the insurer that premium contributions would be accepted for the course of a plan year.65
Commercial dialysis providers and the nonprofit group Dialysis Patient Citizens challenged the CMS rule in court.66 In their lawsuit, the organizations said that CMS did not follow proper notice and comment procedures in publishing the rule and claimed that the rule would cause immediate harm to dialysis patients by disrupting their care, exposing them to additional costs, and potentially denying them access to health insurance. In February 2017, the court issued an injunction stopping the rule from taking effect.67 In April 2018, a coalition of health insurers and businesses wrote a letter asking the Secretary of Health and Human Services (HHS) to take action to end what they also called the steering of ESRD patients into commercial coverage.68
Medicare Reimbursement for ESRD Services
When the ESRD benefit was first implemented, Medicare paid health care providers separate amounts for tests, supplies, drugs, and covered services billed to ESRD patients.69 Over the years, Congress has made a number of changes to the payment system in an effort to control costs. Most recently, as part of the Medicare Improvements for Patients and Providers Act of 2008 (P.L. 110-275), Congress required CMS to implement a prospective payment system (PPS) for Medicare dialysis services.70 A PPS is a method of payment in which amounts or rates of payment are established in advance for a defined period and generally are based on an episode of care, regardless of the actual amount of care used.
Since CMS began the phase-in of the PPS in 2011, annual increases in Medicare fee-for-service spending have been modest, relative to historic trends. Medicare fee-for-service spending for beneficiaries with ESRD was $33.9 billion in 2015, an increase of 2.4% from $33.1 billion in 2014.71 Medicare ESRD spending, when measured on a per-beneficiary rather than an aggregate basis, has decreased or has increased minimally from 2010 to 2015.72 So, most of the growth in Medicare spending over the period has been due to the increase in covered lives. Following is information about current ESRD payment systems, including payment for dialysis and transplants.73
Reimbursement for Outpatient Dialysis Facilities
CMS defines an ESRD facility as an entity that provides outpatient maintenance dialysis services, home dialysis training and support services, or both. ESRD facilities can be hospital based or independently operated.74 To receive Medicare reimbursement for routine dialysis services, ESRD facilities must be certified by CMS as meeting safety and quality standards.75
The ESRD PPS, which was phased in over a four-year period starting in 2011, provides a single, bundled payment for each dialysis treatment in a certified ESRD facility. Patients generally are allowed up to three dialysis treatments per week, either in a dialysis center or at a patient's home. Additional treatments may be covered on the basis of medical necessity. The PPS bundled payment covers dialysis and necessary support services, such as training, laboratory tests, drugs related to ESRD treatment, and ESRD-related supplies (primarily erythropoiesis-stimulating agents, vitamin D, and iron).76 Beneficiaries pay coinsurance equal to 20% of the Medicare-approved amount for each dialysis treatment.
PPS Formula
The ESRD PPS per treatment payment is determined by adjusting the base rate by a number of factors. The base rate, which applies to both adult and pediatric patients, is updated each year based on a market-basket index designed to capture changes in the costs of dialysis-related goods and services.77
In determining the per treatment payment, CMS adjusts the PPS base rate to account for differences in the health profile of patients and operating costs among dialysis providers:
- Patient Characteristics. For adult patients, the PPS base rate is adjusted to account for factors including how long a patient has been undergoing dialysis; age; body surface area; low-body-mass index; and four co-morbidity, or associated disease, categories.78 For pediatric patients, the adjustments include two age categories and two types of dialysis.
- Facility-Level Characteristics. CMS uses three adjustments: (1) a low-volume adjustment for ESRD facilities that provide a smaller number of dialysis treatments, (2) a geographic wage index adjustment, and (3) a rural adjustment for facilities in rural areas.79 For pediatric patients, only the wage index applies.
- Patient Training. CMS provides a home or self-dialysis training add-on payment.
- High-Cost Outliers. CMS provides additional reimbursement for facilities that treat high-cost outlier patients, based on variations in the type or amount of medically necessary care.
- New Drugs. CMS also adjusts the base payment to provide a transitional add-on reimbursement for new injectable or intravenous drugs that do not fit into existing categories under the PPS base rate.80 Under the bundled payment, ESRD facilities are responsible for furnishing renal dialysis services either directly or under arrangement. An exception to the policy is oral-only drugs and biologicals, which are not paid under the ESRD PPD until January 1, 2025.
When initially implementing the PPS, CMS set the bundled payment rate at 98% of the existing cost of dialysis services. In the American Taxpayer Relief Act of 2012 (P.L. 112-240), Congress authorized CMS to gradually reduce, or rebase, the PPS base rate to take into account cost savings from a sharp decrease in the use of intravenous drugs for treating anemia, along with other payment revisions.81 Congress has included provisions in the Protecting Access to Medicare Act of 2014 (P.L. 113-93) and other statutes making further adjustments to the PPS.82
Quality Incentive Program
The ESRD Quality Incentive Program (QIP) ties a portion of the Medicare PPS reimbursement to providers' success in meeting specific quality-of-care measures.83 Under the QIP, CMS annually evaluates whether outpatient dialysis facilities meet a detailed set of standards. Facilities that fall short of the CMS requirements can have their Medicare reimbursement reduced by up to 2%.84
Dialysis facilities are evaluated on both clinical and data reporting factors.85 Clinical factors include the effectiveness of dialysis treatments, the number of unplanned patient readmissions to a hospital, and the rate of infections incurred by in-center hemodialysis outpatients. CMS makes QIP scores available online.86 Dialysis centers must display documents detailing their overall QIP score and their performance on each quality measure identified for that year. The documents must be in English and Spanish.
Acute Kidney Injury
Medicare covers services for individuals with AKI who already were eligible for Medicare. Since January 2017, CMS has reimbursed providers for dialysis services administered to AKI patients in both Medicare-certified hospitals and outpatient facilities.87 Previously, Medicare covered AKI dialysis services as part of hospital-based care. Under the Trade Preferences Extension Act of 2015 (P.L. 114-27), Congress expanded the reimbursement to outpatient centers to reduce the amount of time that AKI patients must remain in the hospital and to provide transitional services to patients, such as those who have had kidney transplants and are waiting for their new kidney to begin functioning.88
Medicare ESRD Comprehensive Care Model
CMS is overseeing a five-year pilot program to evaluate coordinated care models for serving ESRD beneficiaries.89 Under the CMS Comprehensive ESRD Care (CEC) model, which is to run from 2015 through 2020, physicians, dialysis clinics, and other providers have formed ESRD Seamless Care Organizations (ESCOs) to care for ESRD patients. ESCOs are accountable for clinical and financial outcomes, including spending on dialysis services, for the ESRD beneficiaries they treat. According to CMS, the model aims to encourage dialysis providers to broadly address beneficiaries' health needs. There are 37 ESCOs.90
Practitioner Payments
CMS pays physicians, who typically are nephrologists, and other practitioners a monthly per-patient rate for most outpatient dialysis-related services.91 Services covered under the provider payments include analyzing the type of dialysis best suited to a patient, assessing whether a patient requires a special diet, making an initial determination regarding whether a patient is a candidate for a kidney transplant, ordering required tests, performing physical assessments, and reviewing diagnostic and other data. The payment does not include related surgical services, administration of the hepatitis B vaccine, interpretation of certain tests, and performance of a complete (as opposed to initial) evaluation of whether a patient meets the criteria for a kidney transplant.92
Practitioner services can be provided in an office or another covered setting, such as a dialysis facility. For patients receiving treatment in a dialysis facility, the payment rate varies based on the number of patient visits during a month and the ESRD beneficiary's age. Physicians and practitioners managing ESRD patients who perform home-based dialysis are paid a single monthly rate based on the ESRD beneficiary's age. A physician or practitioner is required to have at least one face-to-face visit with a home dialysis patient each month.
In February 2018, Congress enacted the Bipartisan Budget Act of 2018 (BBA 2018; P.L. 115-123). BBA 2018 expands the use of telehealth services for ESRD patients undergoing home dialysis.93 Beginning in 2019, BBA will allow ESRD beneficiaries undergoing home dialysis to receive monthly face-to-face clinical assessments via telehealth services, so long as the individual receives a face-to-face assessment without the use of telehealth (1) at least monthly for the initial three months of home dialysis and (2) after the initial three months, at least once every three consecutive months.
Transplantation
Medicare provides reimbursement for medical services associated with a kidney transplant performed in a hospital that is an approved Medicare transplant facility. Medicare Part A covers the cost of hospital inpatient services for the ESRD patient, as well as the full cost of laboratory tests and pre-surgery, surgical, and post-surgical care for a kidney donor, including any necessary care for complications directly tied to the transplant.94 Medicare Part B covers physicians' services for the ESRD patient and donor, as well as the cost of immunosuppressive drugs.95 (See "Medicare Coverage of Immunosuppressive Drugs.") Medicare also reimburses approved medical facilities for costs connected to the acquisition of a cadaver kidney.
Certain costs are not covered by Medicare, including travel and room-and-board expenses by a donor or a transplant recipient. If an individual has ESRD and requires a pancreas transplant, Medicare will cover the transplant if it is done at the same time as or after a kidney transplant.96
Issues in Medicare ESRD Coverage
Medicare Advantage Enrollment
Medicare Part C (MA) plans cover Part A and Part B services and also may offer supplemental benefits to their enrollees. CMS provides MA plans with monthly per-patient payments that cover the cost of basic health care services but do not cover supplemental services. The CMS payment is risk adjusted, meaning MA plans receive higher payments from CMS for individuals with identified, underlying health conditions, such as heart disease or diabetes, that make them more costly to cover. MA plans may charge enrollees higher premiums for plans that offer extra benefits. Plans may earn higher payments from CMS if they meet certain specified quality measures each year.
Currently, ESRD beneficiaries may enroll in MA plans only in limited circumstances. ESRD beneficiaries may be in MA plans if they (1) developed ESRD while already enrolled in an MA plan, (2) received health benefits through the same organization (such as a group health plan) that offers the MA plan, (3) had a kidney transplant and no longer require dialysis but are entitled to Medicare due to age or disability, or (4) have a Medicare special-needs plan in their geographic area.97 An ESRD beneficiary who is enrolled in an MA plan that is later discontinued has a one-time right to join another MA plan.98
Section 17006 of the 2016 CURES Act (P.L. 114-255) will allow all Medicare-eligible individuals who have been diagnosed with ESRD to enroll in MA plans, beginning in 2021. The CURES Act adjusts the MA payment system to account for the higher expected costs of ESRD enrollees.
Under the CURES Act,
- If an MA enrollee with ESRD undergoes a kidney transplant, the costs of kidney acquisition, including Medicare-covered expenses for kidney donors, will be covered through the fee-for-service provisions of Medicare Parts A and B rather than by a specific MA plan.
- The HHS Secretary must evaluate the impact of including CKD in the MA risk-adjustment payment model. Any changes to MA risk adjustment as a result of the evaluation are to be phased in over a three-year period, beginning in 2019, with such changes being fully implemented for 2022 and subsequent years.
- The HHS Secretary must evaluate whether the current MA quality rating system should be adjusted to account for ESRD enrollees.
MA plans often have networks of providers from whom beneficiaries must receive care. Beneficiaries may be required to see a primary caregiver before being referred to a specialist. As such, ESRD beneficiaries who enroll in MA plans may have access to a more limited network of physicians and dialysis centers, as well as other health care providers, than those enrolled in fee-for-service Medicare. At the same time, MA plans may have more ability to coordinate care for ESRD patients across their network of providers and may have lower cost sharing for many services. MA plans, which pay charge premiums, are subject to an annual cap on enrollee out-of-pocket costs, such as co-payments and deductibles. For 2018, the MA out-of-pocket maximum is $6,700, although plans may offer enrollees a lower cap. The MA limit on out-of-pocket spending could benefit ESRD beneficiaries under the age of 65 who are not able to purchase Medigap coverage, for example.
Medicare Coverage of Immunosuppressive Drugs
Individuals who have had a successful kidney transplant usually take immunosuppressive drugs for the rest of their lives to minimize the risk that their immune systems will reject the donor kidney.99 Medicare covers immunosuppressive drugs under Part B if a kidney transplant was covered by Medicare and performed in a CMS-approved facility. Under Part B, beneficiaries pay 20% of the cost of the drugs. If a Medicare ESRD beneficiary has Part B coverage for immunosuppressive drugs, he or she may not file a claim for the drugs under the Part D outpatient drug benefit. (However, if a Medicare beneficiary does not qualify for Part B coverage, he or she may obtain coverage under Part D.)100
Medicare will cover the lifetime cost of immunosuppressive drugs for individuals who (1) were eligible for Medicare based on age or disability before their ESRD diagnosis or (2) qualified for Medicare due to age or disability after receiving a transplant in a Medicare-approved facility that was covered by Medicare or by a private insurance policy that paid primary to Medicare Part A. Beneficiaries who qualify for Medicare solely on the basis of ESRD are limited to 36 months of Medicare coverage following a successful kidney transplant.101 Once ESRD-only beneficiaries exhaust their 36 months of Medicare eligibility, they lose Part B coverage for immunosuppressive drugs and must pay for the medications out of pocket, through other insurance, or with third-party assistance.
Lawmakers in the past have introduced legislation to expand Medicare Part B coverage of immunosuppressive drugs for ESRD-only enrollees beyond the current 36-month limit. For example, a bill introduced in the 114th Congress, S. 3487, would have allowed individuals who have undergone a transplant, who are under the age of 65, and who do not have Social Security Disability Insurance or a private group health plan to pay a reduced Medicare Part B premium for immunosuppressive drug coverage.