Introduction
The Health Resources and Services Administration (HRSA), of the Department of Health and Human Services (HHS), is the federal agency charged with improving the nation's health safety net. HRSA provides access to health care services for those who are uninsured, isolated, or medically vulnerable, and educates health care providers on maternal and child health issues.1 HRSA's main role in maternal health is through its Maternal and Child Health Bureau (MCHB). The MCHB, in this context, encourages health promotion, promotes risk prevention, and disseminates information to health care professionals with the goal of reducing U.S. cases of severe maternal morbidity (SMM) and maternal mortality. According to the Centers for Disease Control and Prevention (CDC) of HHS
- Severe maternal morbidity refers to a medical condition such as eclampsia and health failure that adversely affects the maternal health outcome of labor and delivery, resulting in either short-term or long-term consequences for pregnant and postpartum women.2
- U.S. maternal death refers to "the death of a woman while pregnant or within 42 days of termination of pregnancy, but excludes those from accidental or incidental causes."3
CDC estimates the U.S. rate of SMM by measuring U.S. cases of SMM per 10,000 delivery hospitalizations. According to the CDC, the overall U.S. SMM rate increased by 190.9% between 1993 and 2014, from 49.5 SMM to 144.0 SMM.4 The CDC estimates the prevalence of U.S. maternal deaths by calculating the U.S. maternal mortality ratio (MMR), which is the number of U.S. maternal deaths per 100,000 live births.5 According to the CDC, the U.S. MMR increased by 32.8% from 13.1 maternal deaths per 100,000 live births in 2004 to 17.4 maternal deaths per 100,000 live births in 2018.6
To address U.S. cases of SMM and maternal mortality, the FY2019 appropriations report language for the Department of Defense and Labor, Health and Human Services, and Education Appropriations Act, 2019, and Continuing Appropriations Act, 2019 (P.L. 115-245), among other things, reserved funds within the Special Projects of Regional and National Significance (SPRANS) for HRSA to administer maternal health programs.7 SPRANS is a competitive grant program for research and training programs and services related to maternal and child health and to children with special health care needs.8
The FY2019 appropriation provided $109.6 million to SPRANS, which explicitly included $26 million for HRSA to maintain and establish new maternal health programs.9 Using the SPRANS authority, HRSA allocated $3 million to the previously existing Alliance for Innovation on Maternal Health (AIM) program and for the establishment of the Alliance for Innovation on Maternal Health (AIM)–Community Care Initiative. Additionally, HRSA allocated $23 million to establish the State Maternal Health Innovation (MHI) program. In FY2019, HRSA also established the Rural Maternity and Obstetrics Management Strategies (RMOMS) program and the Supporting Maternal Health Innovation (MHI) program.10 The appropriations report language authorizes HRSA to use $1 million of the $23 million appropriated, for the purchase and implementation of telehealth11 and to support coordination of rural obstetric care.12
FY2020 Appropriations and FY2021 Budget Request
The FY2020 appropriations report language explicitly provides $5 million to SPRANS for HRSA to carry out the activities through both of the AIM programs and $23 million for the State MHI program; the report language does not explicitly provide funding to the RMOMS program and Supporting MHI program.13 However, Congress appropriated $119.1 million to SPRANS for FY2020—increasing the FY2019 appropriation level by $10.5 million.14
For FY2020, according to HRSA, the federal agency is providing15
- $2 million to the RMOMS program,
- $5 million to carry out the activities through both of the AIM programs, and
- $23 million to the State MHI program.
For FY2021, according to HRSA, the agency is requesting from Congress16
- $12 million for the RMOMS program,
- $15 million to carry out the activities through both of the AIM programs, and
- $53 million for the State MHI program.
HRSA's FY2021 budget documents do not provide information on either prior year or planned funding allocations for the Supporting MHI program.17 HRSA funds the five programs through cooperative agreements. According to HRSA, a cooperative agreement refers to "a financial assistance mechanism where substantial involvement is anticipated between HRSA and the recipient during performance of the contemplated project."18
Overview of the Five Maternal Health Programs
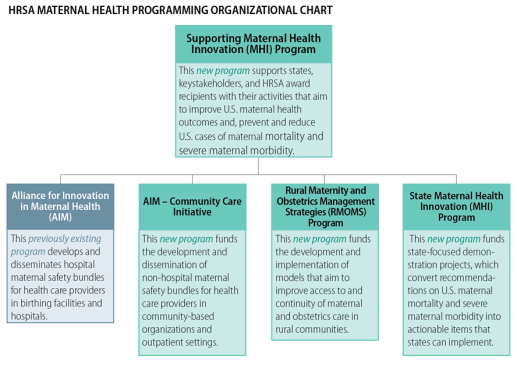
Figure 1 provides an overview of and the coordination between the five maternal health programs.19
|
Figure 1. Overview of the Alliance for Innovation in Maternal Health (AIM) Program and the Four New Maternal Health Programs |
 |
|
Source: CRS prepared this figure using information from (1) Health Resources and Services Administration (HRSA) of the Department of Health and Human Services (HHS), Notice of Funding Opportunity [(NOFO)]: Alliance for Innovation on Maternal Health (AIM), December 18, 2017, https://go.usa.gov/xVk5J; (2) HRSA, NOFO: Alliance for Innovation on Maternal Health (AIM)–Community Care Initiative, May 15, 2019, https://go.usa.gov/xVk5m; (3) HRSA, NOFO: Rural Maternity and Obstetrics Management Strategies Program, March 25, 2019, https://go.usa.gov/xVkQQ; (4) HRSA, NOFO: State Maternal Health Innovation (MHI) Program, May 30, 2019, https://go.usa.gov/xV5Dh; and (5) HRSA, NOFO: Supporting Maternal Health Innovation (MHI) Program, May 30, 2019, https://go.usa.gov/xV5Zd, pp. 30-32. Note: HRSA administers each of the five maternal health programs. |
HRSA is administering the five maternal health programs under the agency's Improving Maternal Health in America initiative.
Report Roadmap
To assist Congress as it considers measures on U.S. maternal health programs, this report provides an overview of the previously existing AIM program and the four new maternal health programs that HRSA established in FY2019. For each of the five maternal health programs, the report
- provides an overview of the program,
- discusses the main core activities or functions of the program,
- provides the program's criteria of eligibility and reporting requirements, and
- discusses the program's funding allocations.
Alliance for Innovation on Maternal Heath (AIM)
The Alliance for Innovation on Maternal Health (AIM) program aims to improve U.S. maternal health outcomes, including maternal safety, by diminishing the number of preventable SMMs and maternal deaths.20 The initiative funds one cooperative agreement to support continuity of care for pregnant and postpartum women who receive maternal health care services at birthing facilities and hospitals. HRSA established the AIM program in 2014. Since 2014, The American College of Obstetricians and Gynecologists (ACOG), which is a medical professional organization for obstetricians and gynecologists, has been the sole grantee of the AIM program.21
During the AIM program's most recent four-year performance period.22 ACOG was responsible for engaging and building partnerships with national stakeholders, promoting the adoption and implementation of hospital-focused maternal safety bundles by state-based teams, and evaluating the delivery of provider education on interconception health.23 According to HRSA, a maternal safety bundle refers to "a set of small, straightforward evidence-based practices, that when implemented collectively and reliably in the delivery setting have improved patient outcomes and reduced maternal mortality and [SMM]."24
|
The Difference Between Evidence-Based Practices and Evidence-Informed Practices Evidence-based practices and evidence-informed practices are two different concepts. The Administration for Children and Families of the Department (ACF) of HHS defines them as follows:
According to ACF, "ideally, evidence-based and evidence-informed programs and practices should be responsive to families' cultural backgrounds, community values, and individual preferences." Source: ACF, Evidence-Based Practice Definitions and Glossaries, https://www.childwelfare.gov/topics/management/practice-improvement/evidence/ebp/definitions/. |
Hospital-focused maternal safety bundles are designed for health care providers in birthing facilities and hospitals. The best practices contained in the maternal safety bundles are grouped into four administrative activities: (1) readiness, (2) recognition and prevention, (3) response, and (4) reporting/systems learning. Listed below are the current eight hospital-focused maternal safety bundles.25
|
1. Maternal Mental Health: Depression and Anxiety |
5. Prevention of Retained [Vaginal] Sponges After Birth |
|
2. Maternal Venous Thromboembolism |
6. Reduction of Peripartum Racial/Ethnic Disparities |
|
3. Obstetric Care for Women with Opioid Disorder |
7. Safe Reduction of Primary Cesarean Birth |
|
4. Obstetric Hemorrhage |
8. Severe Hypertension in Pregnancy |
For example, the text box below describes the Maternal Mental Health: Depression and Anxiety safety bundle.
|
An Example of a Hospital-Focused Maternal Safety Bundle The Maternal Mental Health: Depression and Anxiety maternal safety bundle provides best practices on maternal depression and anxiety to health care professionals. For example, this maternal safety bundle identifies steps that health care professionals can take to improve patient outcomes:
Source: Council on Patient Safety in Women's Health Care, Maternal Mental Health: Depression and Anxiety, https://safehealthcareforeverywoman.org/patient-safety-bundles/maternal-mental-health-depression-and-anxiety/. |
The eight hospital-focused maternal safety bundles, according to HRSA, "include data metrics, are shown to be clinically effective, and are currently being adopted by states for inpatient use."26 As of January 2020, according to HRSA, an estimated 1,300 hospitals in 27 states participate in the initial AIM program.27 The current AIM program has a five-year period of performance of September 1, 2018, through August 31, 2023.
Three Core Activities
Under the AIM program, the award recipient performs three core activities: (1) facilitating multidisciplinary collaborations to reduce the number of preventable SMMs and maternal mortality, (2) guiding the national implementation and adoption of maternal safety bundles, and (3) collecting and analyzing data.28 The overall goal of the core activities is to achieve the program's outcomes. According to HRSA, the program objectives are to do the following:29
- Maintain the existing 10 AIM state-based teams and accept 25 new state-based teams to expand the implementation of the current maternal safety bundles.
- Develop new maternal safety bundles and/or resources that aim to address the quality and safety of maternity care practices.
- Establish a national campaign on SMM and maternal mortality that demonstrates the impact of AIM and maternal safety bundles.
- Prevent 100,000 cases of SMM and 1,000 maternal deaths.
Eligible Applicants
Domestic public and private entities are eligible to apply for the AIM program.30 Eligibility extends to tribes, tribal organizations, community-based organizations, and faith-based organizations.
Reporting Requirements and Performance Measures
The AIM grant recipient is required to provide HRSA with annual progress reports, performances reports, and a final report narrative.31 The recipient is to submit annual reports on progress made toward achieving the program outcomes. The performance reports are to examine measures such as sustainability, depression screening, well-woman visit/preventive care, and health equity in maternal health outcomes, sustainability.32 According to HRSA, "the Project Officer will provide additional information about [the final report narrative] after HRSA makes the award."33
Program Funding
HRSA may annually allocate no more than $2 million to the sole recipient of the AIM–Community Care Initiative.34 This funding is dependent upon the availability of appropriated funds, recipient's satisfactory progress in meeting program's objectives, and the interest of the federal government.35 The AIM program has no cost-sharing or matching requirements. On August 1, 2018, HRSA awarded $2 million to ACOG via a cooperative agreement to continue assisting state-based teams with implementing maternal safety bundles.36
Alliance for Innovation on Maternal Health (AIM)–Community Care Initiative
The Alliance for Innovation on Maternal Health (AIM)–Community Care Initiative is a designed to improve U.S. maternal health and safety. The initiative funds one cooperative agreement to support continuity of care for pregnant and postpartum women who receive maternal health care services at medical facilities outside of birthing facilities and hospitals.37 The AIM–Community Care Initiative builds on the work of the initial AIM program. Together, both AIM programs aim to expand the implementation and adoption of maternal safety bundles to all 50 U.S. states, the District of Columbia, and U.S. territories, as well as tribal entities.38
The AIM–Community Care Initiative focuses on two priority areas:39
- supporting the development and implementation of nonhospital maternal safety bundles for health care providers in outpatient settings and community-based organizations, and
- addressing preventable SMM and maternal deaths among pregnant and postpartum women who receive care outside of birthing facilities and hospitals.
The initial AIM program, which focuses on hospital-based services, began developing two nonhospital maternal safety bundles: (1) Postpartum Care Basics for Maternal Safety: From Birth to the Comprehensive Postpartum Visit, and (2) Postpartum Care Basics for Maternal Safety: Transition from Maternity to Well-Woman Care.40 The AIM–Community Care Initiative is responsible for further developing these two maternal safety bundles. The award recipient is to aim to advance the two nonhospital maternal safety bundles by developing data metrics, testing the bundles' effectiveness in outpatient settings and community-based organizations, and implementing the bundles in medical facilities outside of birthing facilities and hospitals.
The initiative recipient is to collaborate with key stakeholders, including other HRSA grant recipients that address maternal and child health issues, on ways to address preventable SMM and maternal deaths among pregnant and postpartum women who receive care outside of birthing facilities and hospitals. In addition, the awardee is to collaborate with the recipient of the Supporting Maternal Health Innovation Program (discussed in the "Supporting Maternal Health Innovation (MHI) Program" section of this report). The two recipients are to work in partnership to develop resource materials for nonhospital-focused maternal safety bundles.41 After developing the resources, the Supporting MHI recipient is to assist the AIM–Community Care Initiative recipient with disseminating resource materials and other evidence-informed strategies to communities that experience disparities in U.S. maternal morbidity and mortality.42 The AIM–Community Care Initiative has a five-year period of performance of September 30, 2019, through September 29, 2024.
Three Core Activities
Under this program, the recipient of the AIM–Community Care Initiative is to perform three core activities: (1) establishing and convening a maternal safety workgroup, (2) facilitating the national implementation of two maternal safety bundles, and (3) collecting and analyzing data. The overall goal of the core activities is to achieve the program's outcomes. According to HRSA, the program objectives are to do the following:43
- Increase knowledge and awareness of nonhospital-focused maternal safety bundles, and identify how bundle contents are related to best practices among providers, community-based organizations, outpatient clinical settings, etc.
- Increase the capacity to implement and test nonhospital-focused maternal safety bundles.
- Increase the number of nonhospital-focused maternal safety bundles developed that address emerging topics in the provision of maternal care services.
- Increase implementation of the nonhospital-focused maternal safety bundles within nonclinical community-based organizations and outpatient clinical settings across states/communities.
- Increase awareness of staff and providers in both inpatient and outpatient clinical settings regarding the need to address racial/ethnic disparities when implementing all nonhospital-focused maternal safety bundles.
- Increase the evidence base on the implementation of nonhospital-focused maternal safety bundles.
The first core activity requires the AIM–Community Care Initiative award recipient to establish a maternal safety workgroup to guide the activities of the program.44 Members of the maternal safety workgroup must include community-focused public health and clinical experts in the field of maternal health.
The second core activity requires the award recipient to facilitate the national implementation of nonhospital maternal safety bundles at approximately five test sites.45 The test sites, which subrecipients will manage, are to be located at outpatient clinical settings and nonclinical organizations. The test sites must provide health care services to pregnant and postpartum women.
The award recipient is to collaborate with the initial AIM program's state-based teams and other key stakeholders to determine how to best disseminate the nonhospital maternal safety bundles nationwide. Like the test sites, the nonhospital maternal safety bundles are to be adopted by outpatient clinical settings and community-based organizations that provide health care services to pregnant and postpartum women. HRSA expects the recipient of the AIM–Community Care Initiative to collaborate with the current AIM program award recipient.46 The AIM program is to maintain a public website containing materials on non-hospital focused maternal safety bundles. The website would be further developed and maintained by the AIM–Community Care Initiative recipient, who would also support the collaboration of the AIM website and the Supporting MHI program website.47
The third core activity requires the award recipient to collect and analyze structure, process, and outcome data.48 According to HRSA, the recipient will collect and analyze "quality improvement baseline, process, structure, and outcome data on the implementation of non-hospital focused maternal safety bundles, both within test sites and during national rollout."49
Eligible Applicants
Domestic public and private entities are eligible to apply for the AIM–Community Care Initiative.50 Eligibility extends to tribes, tribal organizations, community-based organizations, and faith-based organizations.
Reporting Requirements and Performance Measures
The AIM–Community Care Initiative awardee is required to provide HRSA with annual progress reports, performance reports, and a final report narrative.51 The recipient is to submit annual reports on progress made toward achieving the program outcomes/objectives (as described in the "Three Core Activities" section above). The performance reports would examine measures such as quality improvement, health equity in maternal health outcomes, sustainability, and well-woman visit/preventive care.52 The final performance report must include the project's abstract, expenditure data for the final year of the performance period, and the final scores for the performance measures. According to HRSA, "the Project Officer will provide additional information about [the final report narrative] after HRSA makes the award."53
Program Funding
HRSA may annually allocate approximately $1,830,000 to the sole recipient of the AIM– Community Care Initiative.54 This funding is dependent upon the availability of appropriated funds, recipient's satisfactory progress in meeting program's objectives, and the interest of the federal government.55 The program has no cost-sharing or matching requirements. The recipient may use the funds for direct, indirect, facility, and administrative costs. Annually, approximately 40% to 50% of the award must cover the costs of subrecipients' test sites and travel/meeting compensation for members of the maternal safety workgroup.56 In FY2019, HRSA awarded $1.8 million to one recipient.57
Rural Maternity and Obstetrics Management Strategies (RMOMS) Program
The Rural Maternity and Obstetrics Management Strategies (RMOMS) program is a maternal health care pilot program that funds up to three cooperative agreements for the development, implementation, and testing of models that aim to improve access to and continuity of maternal and obstetrics care in rural communities.58 RMOMS program recipients serve communities based on factors such as disparities in ethnicity/race, socioeconomic status, primary language, access to maternal health care, and coordinated/continuing maternal and obstetrics care.59 According to HRSA, the RMOMS program has four goals:60
- 1. improve maternal and neonatal health care outcomes,
- 2. develop sustainable financing models,
- 3. develop a network whereby coordination of maternal and obstetric care is sustainable within a rural region, and
- 4. increase access to and the delivery of preconception, pregnancy, labor and delivery, and postpartum health care services.
The FY2019 RMOMS program has a four-year performance period, September 1, 2019, through August 31, 2023.
The program occurs in two phases.
Phase one. The first phase occurs during the first year of the performance period. During this year, RMOMS program recipients develop baseline data, models, and work plans.61 In addition, the program recipients participate in the development of network capacity building and infrastructure. RMOMS program recipients collaborate with HRSA to assess the program's impact using specific measures and data elements, including access, workforce proficiency, cost and cost-effectiveness, clinical outcomes, quality of care, and healthy behaviors.62
The models are designed to address the four RMOMS focus areas described below in the "Four RMOMS Focus Areas" section of this report. In addition, each model addresses payment and reimbursement options, workforce skills required of maternal health care providers, and women's access to maternal health care services, including telehealth.63 According to HRSA, telehealth refers to "the use of electronic information and telecommunication technologies to support long-distance clinical health care, patient and professional health-related education, public health, and health administration."64 (Of the $23 million that Congress provided to SPRANS for the establishment of new maternal health grants in FY2019, Congress reserved $1 million for the purchase and implementation of telehealth and to, support coordination of rural obstetric care.)65
RMOMS program award recipients are to develop and submit to HRSA three-year work plans, which include the baseline data and strategic plans to implement the model.66
Phase two. The second phase occurs during the remaining second through fourth years of the pilot program. During these years, RMOMS program award recipients implement the models based on the recipients' work plans.67 In addition, the recipients are to provide mothers and infants with case management and care coordination services. The recipients would collaborate with HRSA to identify the data elements to monitor and measure through the model.
Four RMOMS Focus Areas
Each RMOMS program award recipient creates strategies to address each of the four RMOMS focus areas: (1) rural hospital obstetric service aggregation,68 (2) network approach to coordinating a continuum of care, (3) leveraging telehealth and specialty care, and (4) financial sustainability.69
Eligible Applicants
Domestic public or private and nonprofit or for-profit entities are eligible to apply for the RMOMS program.70 Eligibility extends to tribes, tribal organizations, community-based organizations, and faith-based organizations. Eligible entities, which HRSA refers to as "applicant organizations," are equipped with necessary staff and infrastructure to direct the administrative and programmatic activities of the program.71
The applicant organization may be located in either an urban or a rural area. However, the application organization must serve a population either in HRSA-designated rural counties or rural census tracts in urban counties. (The Office of Rural Health Policy within HRSA funded the development of Rural Urban Area Codes to classify areas within metropolitan areas as HRSA-designated rural counties and rural census tracts in urban counties.)72 An entity could have applied twice for the FY2019 RMOMS program: (1) as an applicant organization and (2) as part of a network organization under a different applicant organization.
RMOMS applicant organizations must be part of either a formal or an established network. HRSA refers to a network as
an organizational arrangement among three or more separately owned domestic public and/or private entities, including the applicant organization. For the purposes of this program, the applicant must have a network of composition that includes: (1) at least two rural hospitals or [critical access hospitals (CAHs)]; (2) at least one health center under section 330 of the Public Health Service Act (Federally Qualified Health Center [FQHC]) or FQHC look-alike; (3) state Home Visiting and Healthy Start Program if regionally available; and (4) the state Medicaid agency.73
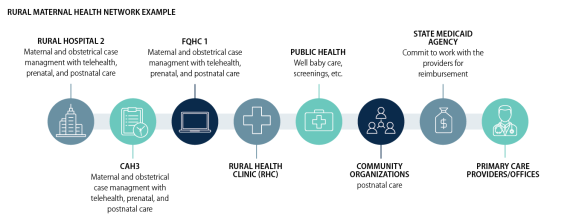
A formal network is a RMOMS Network organization that has signed bylaws, a governing body, and either a memorandum of agreement, memorandum of understanding, or other formal collaborative agreements.74 HRSA identifies a formal network that has a history of working together as an established network. At least one entity, aside from the applicant organization, within the network must be located in an HRSA-designated rural county or rural census tract in an urban county. Each RMOMS applicant organization and the entities that are part of a network must have separate and different Employer Identification Numbers (EINs) from the Internal Revenue Service.75 Separate and different EINs are required in order to receive RMOMS program funds. Figure 2 illustrates an example of a RMOMS network.
|
Figure 2. Example of a Possible Network Under the Rural Maternity and Obstetrics Management Strategies (RMOMS) Program |
 |
|
Source: CRS prepared this figure using information from Health Resources and Services Administration, Notice of Funding Opportunity: Rural Maternity and Obstetrics Management Strategies Program, March 25, 2019, pp. 7-8, https://go.usa.gov/xVkQQ. |
Reporting Requirements and Performance Measures
RMOMS program award recipients are required to provide HRSA with annual progress reports, a performance measure report, a sustainability report, and a final closeout report.76 Recipients are to submit annual reports on progress in achieving the program's four goals (as described in the "Rural Maternity and Obstetrics Management Strategies (RMOMS) Program" section of this report). In addition, the annual reports must specifically include progress toward addressing the third RMOMS focus area, "leveraging telehealth and specialty care." After the end of each budget period, RMOMS program recipients are to submit reports on performance measures. HRSA is to inform the program recipients of the performance measures to report on, during the first year of performance.77 HRSA provides guidance to RMOMS program recipients on how to complete the sustainability report, which is due during the final year of the performance period.
Each RMOMS program award recipient is to provide the MCHB with a final closeout report within 90 days after the end of the performance period.78 The final report must include information and data such as barriers encountered, core performance data, and the impact of the overall project. The Notice of Award provides program recipients with additional information about the final report.
Program Funding
HRSA uses two authorities to administer and fund the RMOMS program, according to the program's Notice of Funding Opportunity (see Table 1).79 Using its authority for SPRANS (SSA Section 501(a)(2)),80 HRSA may provide up to $150,000 to RMOMS program recipients to carry out activities under the RMOMS focus area "leveraging telehealth and specialty care" for each year of the pilot program.81 Using its authority for the Office of Rural Health Policy within HRSA (SSA §711(b)(5)),82 HRSA may provide up to $450,000 for recipients to carry out the activities under each of the four RMOMS focus areas for the first year of the pilot program.83 For each of the remaining years of the pilot program, RMOMS may award recipients receive up to $650,000 to carry those activities. Each RMOMS recipient may receive up to $1.8 million per year.
Table 1. Award Caps for the Rural Maternity and Obstetrics Management Strategies (RMOMS) Program, by Year of Performance
(dollars)
|
RMOMS Focus Area |
Year 1 |
Year 2 |
Year 3 |
Year 4 |
Total |
|
Rural Hospital Obstetrics Service Aggregation |
$450,000 |
$650,000 |
$650,000 |
$650,000 |
$2,400,000 |
|
Network Approach to Coordinating a Continuum of Care |
$450,000 |
$650,000 |
$650,000 |
$650,000 |
$2,400,000 |
|
Leveraging Telehealth and Specialty Care |
$600,000 |
$800,000 |
$800,000 |
$800,000 |
$3,000,000 |
|
Financial Sustainability |
$450,000 |
$650,000 |
$650,000 |
$650,000 |
$2,400,000 |
|
Total |
$1,950,000 |
$2,750,000 |
$2,750,000 |
$2,750,000 |
$10,200,000 |
Source: CRS prepared table using data from HRSA, Notice of Funding Opportunity: Rural Maternity and Obstetrics Management Strategies Program, March 25, 2019, pp. 2 and 20, https://go.usa.gov/xVkQQ.
Notes: For each year of funding for the "leveraging telehealth and specialty care" RMOMS focus area, $150,000 comes from HRSA's SPRANS authority. The remaining funding for each year comes from HRSA's Office of Rural Health Policy.
This funding is dependent upon the availability of appropriated funds, satisfactory recipient performance, and the interest of the federal government.84
RMOMS program award recipients can use funds for direct and indirect costs. In addition, recipients may use funds to cover staff travel expenses to conferences and/or technical assistance workshops. HRSA expects RMOMS program recipients to set-aside funds each year for up to two program staff members to attend a two-and-a-half day technical workshop in Washington, DC.85 There are no cost-sharing or matching requirements for this program. According to HRSA, the total program costs incurred by the supporting MHI satisfies a cost-sharing or matching requirement.86 In FY2019, HRSA awarded $9 million to the RMOMS program.87
State Maternal Health Innovation (MHI) Program
The State Maternal Health Innovation (MHI) program is a maternal health program that funds up to nine cooperative agreements for state-focused demonstration projects, with the goal of improving U.S. maternal health outcomes.88 State MHI award recipients are to establish demonstration projects within a state or group of states. The demonstration projects are responsible for converting recommendations on SMM and maternal mortality into actionable items that can be implemented by the states or groups of states. Recommendations—such as providing maternal women with continuous team-based support, improving quality of maternity health care services, and engaging in productive collaborations—derive from HRSA's Maternal Mortality Summit, held in June 2018.89 State MHI program recipients are required to collaborate with other HRSA program awardees of programs such as AIM, the Healthy Start Program (Healthy Start), and Maternal, Infant, and Early Childhood Home Visiting (MIECHV) programs90 in their state. The FY2019 State MHI program has a five-year performance period, September 30, 2019, through September 29, 2024.
Three Core Functions
Each state-focused demonstration project undertakes three core functions: (1) establishing a state-focused Maternal Health Task Force, (2) improving state-level maternal health data and surveillance, and (3) promoting and executing innovation in maternal health service delivery.91
Maternal Health Task Force
Each State MHI award recipient is responsible for establishing, and each state-focused demonstration project operates through, a state-focused Maternal Health Task Force (Task Force). The Task Force comprises multidisciplinary stakeholders, including representatives from the state legislature and local public health professionals from state and federal programs, such as the State Department of Health and MCH Services Block Grant Program (Title V). The Task Force is responsible for carrying out two main objectives.
First, the Task Force is responsible for identifying maternal health-related gaps at the state level. Examples of such gaps include a state's limited ability to monitor maternal health outcomes and the access barriers that women experience when accessing quality prenatal and maternity care services.
Second, the Task Force is responsible for creating and implementing a maternal health strategic plan. The strategic plan must include the maternal health care activities outlined in the most recent State Title V Needs Assessment of each state or group of states. However, state-focused demonstration projects are encouraged not to duplicate the maternal mortality-related activities of the MCH Services Block Grant program. State MHI award recipients must develop their strategic plans by September 29, 2020, and update the plans by including additional actionable recommendations by September 29, 2021.92
Although not a core function, the Task Force is required to participate in the community of learners' sessions, which are convened by the recipient of the Supporting MHI Program.93 The goal of convening the community is to encourage peer-to-peer learning, including collective problem-solving and brainstorming sessions on ways the State MHI program recipients can effectively implement their program activities.
Maternal Health Data and Surveillance
Each State MHI award recipient is to aim to improve state-level data on maternal health data and surveillance through the state-focused demonstration project. To do so, the award recipient is to identify the leading factors of maternal deaths in the respective state or groups of states. A state-focused demonstration project can address the state or group of states' need for maternal health data and surveillance by conducting at least one of three activities. The demonstration project can coordinate with another state-focused initiative to collect, analyze, and report maternal morbidity and mortality data. The demonstration project may also coordinate with a multidisciplinary state-focused maternal mortality review committee (MMRC).94 An MMRC is a multidisciplinary team composed of maternal clinical health experts.95 Generally, an MMRC team researches and makes recommendations on maternal mortality-related issues such as racial maternal health disparities.
In addition, the demonstration project can analyze valid and reliable data on U.S. maternal health outcomes. For example, the goal of the analysis is to determine the preventability of certain maternal deaths and to establish best practices on how to prevent future deaths. The demonstration project can also publish an annual report on maternal death that includes a discussion on how to prevent such deaths from a policy standpoint.
Maternal Health Service Delivery
Each State MHI award recipient is to promote and execute innovation in maternal health service delivery, for example, by implementing strategies to address gaps in the delivery of maternal health care. State-focused demonstration projects can implement innovative strategies by conducting at least one of the following three activities: (1) identifying critical gaps in access to comprehensive, continuous, and high-quality maternal health care services; (2) identifying critical gaps in maternal health workforce needs; and (3) identifying critical gaps in comprehensive postpartum and interconception care interventions. For example, a state-focused demonstration project can96
- assist state birthing facilities with implementing and adopting AIM maternal safety bundles,
- address access to maternal health care by convening a state advisory panel on innovation payment models for maternal care,
- address maternal health workforce needs by identifying legislative mandates that affect maternal women accessing maternal health care services, and
- address comprehensive postpartum and interconception care intervention by disseminating patient educational information on preventing obstetric emergencies.
HRSA encourages award recipients to include the use of telehealth as a component of their demonstration projects. The Supporting MHI program recipient hosts the web-based platform, which the State MHI program recipients use to consolidate their work.97 In addition, the Supporting MHI recipient plans, hosts, and facilitates the annual in-person meetings for State MHI award recipients.
Eligible Applicants
Domestic public and private entities are eligible to apply for the State MHI Program.98 Eligibility extends to tribes, tribal organizations, community-based organizations, and faith-based organizations.
Reporting Requirements and Performance Measures
State MHI Program award recipients are required to provide HRSA with annual progress reports, performance reports, and a final report narrative.99 By September 29, 2020, award recipients must submit annual reports on the maternal deaths and ways to prevent future maternal deaths in the state. Award recipients must include data in their reports that HRSA can measure under the State Title V Needs Assessment. By that same date, according to HRSA, the award recipients must report the following two sets of performance data to the agency:100
1. Increases within the state from baseline on September 30, 2019, for the following:
- percentage of women covered by health insurance,
- percentage of women who receive an annual well-woman visit,
- percentage of pregnant women who receive prenatal care,
- percentage of pregnant women who receive prenatal care in the first trimester,
- percentage of pregnant women who receive a postpartum visit, and
- percentage of women screened for perinatal depression.
2. Decreases within the state from baseline on September 30, 2019, for the following:
- rate of pregnancy-related deaths, and
- racial, ethnic, and/or geographic disparities in pregnancy-related mortality rates.
The Supporting MHI award recipient is required to help the State MHI award recipients achieve their performance milestones.101 The performance reports examine measures such as quality improvement, state capacity for advancing the health of maternal and child health populations, prenatal care, well-woman visit/preventive care, and adequate health insurance coverage.102 The final performance report must include the project's abstract, expenditure data for the final year of the period of performance, and the final scores for the performance measures. Each State MHI award recipient must submit its final report narrative to HRSA at the end of the project.
Program Funding
HRSA may annually allocate approximately $18,650,000 to fund up to nine cooperative agreements under the State MHI program. This funding is dependent upon the availability of appropriated funds, satisfactory recipient performance, and the interest of the federal government.103 In FY2019, the awards ranged from $1.9 million to $2.1 million.104 State MHI program award recipients can use funds to address state and local priorities.105 There are no cost-sharing or matching requirements for this program.
Supporting Maternal Health Innovation (MHI) Program
The Supporting Maternal Health Innovation (MHI) program funds up to one cooperative agreement to help states, stakeholders, and recipients of HRSA-administered awards reduce and prevent U.S. cases of SMM and maternal mortality, and improve U.S. maternal health outcomes.106 States and stakeholders include state health agencies, community-based organizations, and pregnant and postpartum women and their families. HRSA recipients include those of the initial AIM program, AIM–Community Care Initiative, Healthy Start, and MCH Services Block Grant program. Supporting MHI program award recipients aim to achieve the following three program objectives by calendar year 2024:107
- Ensure that 75% of HRSA award recipients report improvement in their ability to implement evidence-informed strategies, with the goal of reducing and preventing maternal morbidity and mortality.
- Support the State MHI program by ensuring that 75% of HRSA award recipients that aim to improve maternal health outcomes can access the peer-to-peer learning opportunities and resources available through the State MHI program.
- Support the AIM–Community Care Initiative by (1) increasing the dissemination of resource materials to support the adoption of nonhospital-focused maternal safety bundles, and (2) increasing the dissemination of evidence-informed strategies in communities that experience disparities in U.S. maternal morbidity and mortality.
The FY2019 Supporting MHI program has a five-year performance period, September 30, 2019, through September 29, 2024.
Two Core Functions
The State MHI program funds a single project that undertakes two core functions: (1) providing capacity-building assistance, and (2) establishing a national resource center.108
Capacity-Building Assistance
The Supporting MHI project provides capacity-building assistance to the state-focused demonstration projects under the State MHI program and to the recipients under the RMOMS program. In this context, capacity-building assistance refers to technical assistance, training, and dissemination of information.109 The Supporting MHI program grantee provides the State MHI program and the RMOMS program with technical assistance in the form of programmatic, scientific, and mentoring support. Both programs receive training assistance to develop and deliver curricula. The programs also receive support to disseminate evidence-informed strategies to communities that experience disparities in U.S. maternal morbidity and mortality. The Supporting MHI recipient is to provide capacity-building assistance on 10 topic areas, listed below.110
|
1. Data collection and evaluation of innovative and evidence-informed interventions and strategies |
6. Other areas to address emerging maternal health issues, as identified by award recipients |
|
2. Innovative and evidence-informed interventions and strategies to improve maternal health outcomes |
7. Patient and provider education and awareness related to SMM and maternal mortality |
|
3. Maternity care services in medically underserved communities |
8. Postpartum care |
|
4. Maternity care workforce shortages |
9. State maternal mortality review committees |
|
5. Maternal telehealth and telemedicine strategies (e.g., mobile applications, remote pregnancy monitoring of specific conditions) |
10. Use of data in designing and implementing innovative and evidence-informed strategies |
The Supporting MHI program award recipient is to gather the community of learners for the State MHI program recipients.111 The goal of convening the community of learners is to encourage peer-to-peer learning, including collective problem-solving and brainstorming sessions on ways the State MHI program recipients can effectively implement program activities. In addition, the Supporting MHI program recipient is to help the State MHI program recipients assess their progress in meeting program goals and planning and facilitating annual in-person meetings for the recipients.
National Resource Center
The Supporting MHI program recipient is responsible for establishing a national resource center where states, HRSA award recipients, and key stakeholders can access guidance on reducing and preventing U.S. cases of SMM and maternal mortality.112 The resource center offers assistance with trainings/technical issues, partnership building, policy analysis, and dissemination of information. Trainings and technical assistance are provided to stakeholders and HRSA award recipients on topic areas similar to the 10 topic areas described above. HRSA award recipients under this program may include grantees of Healthy Start, the MIECHV program, and the MCH Services Block Grant program.
The Supporting MHI program recipient, through the resource center, would collaborate with stakeholders that serve underserved populations to encourage partnership building. Key stakeholders and HRSA award recipients may reach out to the resource center for assistance with developing partnerships with national maternal health organizations (e.g., ACOG, the Association of Women's Health, Black Mamas Matter Alliance, Society for Maternal Fetal Medicine, and Telehealth Resource Centers).
The resource center offers policy analysis assistance to stakeholders and HRSA award recipients. For example, the AIM–Community Care Initiative award recipient can receive assistance in determining whether any of the nonhospital maternal safety bundles are evidence-informed and could reduce U.S. cases of SMM and maternal mortality.113 In addition, the resource center develops and maintain a public-facing web-based clearinghouse where key stakeholders can access pertinent resources, such as training materials and evidence-informed practices. The website must have the capability to host the State MHI program recipient's online platform.
The Supporting MHI program is also responsible for creating and implementing national guidance on reducing U.S. cases of maternal morbidity and mortality. Education and training are the foci of the national guidance. The national guidance provides learning opportunities to key stakeholders on the following nine topic areas:114
|
1. Data collection and evaluation of innovation and evidence-informed interventions and strategies |
6. Other areas to address emerging maternal health issues as identified by award recipients |
|
2. Innovation and evidence-informed interventions and strategies to improve maternal health outcomes |
7. Patient and provider education and awareness related to SMM and maternal mortality |
|
3. Maternal telehealth and telemedicine strategies |
8. Postpartum care |
|
4. Maternity care services in medically underserved communities |
9. State maternal mortality review committees |
|
5. Maternity care workforce shortages |
The national guidance is intended to help key stakeholders with related activities, such as creating tools for collaborations, disseminating information about the project, and providing culturally competent technical assistance to key stakeholders that provide maternal health services to populations that experience disparities in U.S. maternal morbidity and mortality.115
Eligible Applicants
Domestic public and private entities are eligible to apply for the Supporting MHI Program.116 Eligibility extends to tribes, tribal organizations, community-based organizations, and faith-based organizations. Eligible applicants must be aware of the different HRSA award recipients that address U.S. maternal health outcomes.
Reporting Requirements and Performance Measures
The Supporting MHI Program awardee is required to provide HRSA with annual progress reports, performance reports, and a final report narrative.117 By 2024, according to HRSA, the award recipient must submit annual reports on progress made toward achieving the three program objectives listed under the "Supporting Maternal Health Innovation (MHI) Program" section in this report. The performance reports must examine measures such as technical assistance, health equity in maternal health outcomes, state capacity for advancing the health of maternal and child health populations, perinatal and postpartum care, depression screening, and adequate health insurance coverage.118 The final performance report must include the project's abstract, expenditure data for the final year of the performance period, and the final scores for the performance measures. Each State MHI awardee must submit its final report narrative to HRSA within 90 days from the end of the performance period.
Program Funding
HRSA may annually award approximately $2.6 million to the sole recipient, as the agency did in FY2019.119 This funding is dependent upon the availability of appropriated funds, satisfactory recipient performance, and the interest of the federal government.120 The Supporting MHI program recipient can use the funds for administrative and facility costs. There are no cost-sharing or matching requirements for this program. According to HRSA, the total program costs incurred by the Supporting MHI satisfies a cost-sharing or matching requirement.121