Introduction
This report provides background on Department of Defense's legacy Electronic Health Record (EHR) systems, reviews previous EHR modernization efforts, and describes DOD's process to acquire and implement a new EHR system known as MHS Genesis. DOD's new EHR system presents several potential issues for Congress, including how to conduct oversight on a program that spans three federal departments, how to ensure an adequate governance structure for the program, and how to monitor the program's cost and effectiveness.
Although this report mentions EHR modernization efforts by the Department of Veterans Affairs (VA) and U.S. Coast Guard (USCG), as well as DOD's Joint Operational Medical Information System (JOMIS); it does not provide an in-depth discussion of these programs.
Appendix A provides a list of acronyms used throughout this report.
Background
For decades, the Department of Defense (DOD) has developed, procured, and sustained a variety of electronic systems to document the health care services delivered to servicemembers, military retirees, and their family members. DOD currently operates a number of legacy EHR systems and is, at the direction of Congress, in the process of implementing a new EHR called MHS Genesis. DOD's new EHR system is to be integrated with other EHR systems utilized by the VA, USCG, and civilian health care providers.
DOD operates a Military Health System (MHS) that delivers to military personnel, retirees, and their families certain health entitlements under chapter 55 of Title 10, U.S. Code. The MHS administers the TRICARE program,1 which offers health care services worldwide to over 9.5 million beneficiaries in DOD hospitals and clinics – also known as military treatment facilities (MTFs) – or through participating civilian health care providers (i.e., TRICARE providers).2 There are currently 723 MTFs located in the United States and overseas that provide a range of clinical services depending on size, mission, and level of capabilities.3
Health care services delivered in MTFs or by TRICARE providers are documented in at least one of the following components of the DOD health record:
- service treatment record (STR) – documentation of all medical and dental care received by a servicemember through their military career;
- nonservice treatment record (NSTR) – documentation of all medical and dental care received by a nonservicemember beneficiary (i.e., military retiree, family member); and
- occupational health civilian employee treatment record (OHTR) – documentation of all occupational-related care provided by DOD (typically to DOD civilian or contractor employees).4
DOD maintains numerous legacy EHR systems that allow health care providers to input, share, and archive all documentation required to be in a beneficiary's health record.5 MTF or TRICARE providers can document medical and dental care directly in a DOD legacy EHR system, or can scan and upload paper records. Servicemembers and their families frequently change duty stations; the DOD health record can be accessed at most MTFs. However, sometimes beneficiaries are relocated to an area that lacks access to DOD's legacy EHR systems. In such cases, beneficiaries are required to maintain a paper copy of the health record.6
Brief History of DOD's Electronic Health Record (EHR)
Since 1968, DOD has used various electronic medical information systems that automate and share patient data across its MTFs. Between 1976 and 1984, DOD invested $222 million to "acquire, implement, and operate various stand-alone and integrated health-care computer systems."7 Over the next three decades, DOD continued to invest and to implement numerous electronic medical information systems to allow health care providers to input and review patient data across all MTFs, regardless of military service or geographic location. In 1998, DOD began to incorporate a series of efforts to increase interoperability with the VA's EHR systems (see Figure 1).
|
Figure 1. Recent Highlights in DOD's Electronic Health Record Systems Deployment 1998-2018 |
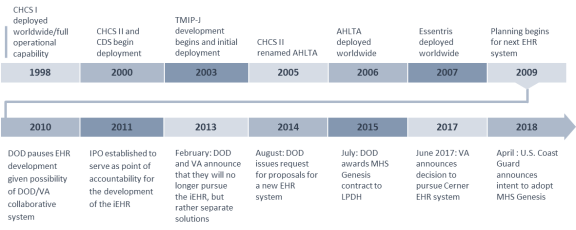 |
|
Source: CRS graphic based on information from CRS Report R42970, Departments of Defense and Veterans Affairs: Status of the Integrated Electronic Health Record (iEHR), by Sidath Viranga Panangala and Don J. Jansen (out of print, available to congressional clients on request); Secretary of Defense Memorandum, "Integrated Electronic Health Records," OSD005932-13, May 21, 2013, https://health.mil/Reference-Center/Policies/2013/05/21/Memorandum-on-the-Integrated-Electronic-Health-Record; Department of Veterans Affairs, "VA Secretary announces decision on next-generation Electronic Health Record," press release, June 5, 2017, https://www.va.gov/opa/pressrel/includes/viewPDF.cfm?id=2914; and U.S. Coast Guard, "Electronic Health Records Acquisition," accessed October 10, 2019, https://www.dcms.uscg.mil/Our-Organization/Assistant-Commandant-for-Acquisitions-CG-9/Programs/C4ISR-Programs/Electronic-Health-Records-Acquisition/. Notes: AHLTA = Armed Forces Health Longitudinal Technology Application; CDS = Corporate Dental System; CHCS = Composite Health Care System; iEHR = Integrated Electronic Health Record; IPO = Interagency Program Office; LPDH = Leidos Partnership for Defense Health; TMIP-J = Theater Medical Information Program – Joint. |
DOD Legacy EHR Systems
DOD operates numerous legacy EHR systems as described below. Together, health care data documented and archived in the legacy EHR systems contribute to a beneficiary's overall medical and dental record, also known as the DOD health record. MHS Genesis is intended to replace these legacy systems and produce one comprehensive EHR.
Composite Health Care System (CHCS)
CHCS is a medical information system that has been in operation since 1993.8 CHCS primarily functions as the outpatient component of the EHR, with additional capabilities to order, record, and archive data for laboratory, radiology, and pharmacy services. Administrative functions such as patient appointment and scheduling, medical records tracking, and quality assurance checks, were also incorporated into CHCS. In March 1988, DOD awarded Science Applications International Corporation (SAIC) a contract to "design, develop, deploy, and maintain CHCS."9 SAIC continues to provide ongoing sustainment and technical support for CHCS. The estimated life-cycle cost of CHCS is $2.8 billion.10
Armed Forces Health Longitudinal Technology Application (AHLTA)
After deploying CHCS, DOD identified a need for integrated health care data that could be portable and accessible at any MTF. CHCS was developed as a facility-specific system that archived its data using regional network servers. However, accessing data across each server became a "time- and resource-intensive activity."11 In 1997, DOD began planning for a new "comprehensive, lifelong, computer-based health care record for every servicemember and their beneficiaries."12 The program would be known as CHCS II, later renamed the Armed Forces Health Longitudinal Technology Application (AHLTA).13
DOD intended to replace CHCS with AHLTA and initially planned to deploy the new system in 1999. However, the program sustained several delays resulting from "failure to meet initial performance requirements" and changes to technical and functional requirements.14 The implementation plan was later revised to reflect AHTLA deployment from July 2003 to September 2007. In 2010, the Government Accountability Office (GAO) reported that DOD's AHLTA life-cycle cost estimate through 2017 would be $3.8 billion.15
Essentris
Essentris is the inpatient component of the current EHR that has been used in certain military hospitals since 1987.16 As a commercial-off-the-shelf (COTS) product developed by CliniComp International, Inc. (CliniComp), Essentris allows health care providers to document clinical care, procedures, and patient assessments occurring in the inpatient setting, as well as in emergency departments. In 2009, DOD selected CliniComp to deploy Essentris at all military hospitals.17 This deployment was completed in June 2011.18 DOD maintains an ongoing contract with CliniComp and LOUi Consulting Group, Inc. to provide sustainment, technical and customer support, training, and ongoing updates for Essentris.19
Corporate Dental System (CDS)
CDS, formerly named the Corporate Dental Application, is a web-based application that serves as DOD's current electronic dental record system. CDS allows DOD dental providers to document, review, and archive clinical information. The system also serves several administrative functions, such as tracking dental readiness of servicemembers, patient appointments and scheduling, and data reporting.20 CDS was initially developed as the Army's alternative dental solution to the AHLTA dental module.21 In 2000, all Army dental clinics implemented CDS.22 By 2016, Navy and Air Force dental clinics also transitioned to CDS as their electronic dental record system.23 In the same year, DOD awarded a four-year, $30 million contract to the Harris Corporation to sustain CDS.24
Paper Medical Records
Paper medical records are another component of the DOD health record. While certain health care data are recorded and archived electronically, some administrative processes and clinical documentation exist only on paper forms. For example, clinical documentation from TRICARE providers, accession medical records, or medical evacuation records are usually in paper form. In such cases, DOD policy requires the scanning and archiving of paper medical records in an electronic repository called the Health Artifact and Image Management Solution (HAIMS).25 After being digitized, certain paper medical records are submitted to the National Archives and Records Administration while other documents are disposed of locally.
Other DOD legacy systems document and archive various administrative and clinical data, such as:
- Referral Management System (RMS). An administrative information system that allows MTF staff to create and track referrals between health care providers.
- HAIMS. An electronic repository that stores DOD health care data, including digitally transmitted or scanned medical documentation.26 Data housed in HAIMS is also incorporated into a servicemember's official service treatment record, which is accessible to the VA.27
- Medical Readiness Tracking Systems. Each military department utilizes an electronic information system that documents and tracks certain medical and dental readiness requirements, such as periodic health assessments, immunizations, dental exams, and laboratory tests.28
- Theater Medical Information Program–Joint (TMIP-J). A suite of electronic systems, including modules for health care documentation and review, patient movement, and medical intelligence used in deployed or austere environments.29
- Joint Legacy Viewer (JLV). A web-based, read-only application that allows DOD and VA health care providers to review certain real-time medical data housed in each department's EHR systems.30
- Armed Forces Billing and Collection Utilization Solution (ABACUS). A web-based electronic system that allows MTFs to bill and track debt collection for health care services provided to certain beneficiaries.31
Developing an EHR Modernization Solution
After Operation Desert Storm concluded in 1991, concern about deficient interoperability between DOD and VA health record systems began to grow. A number of committees and commissions issued reports highlighting the need for DOD and VA to standardize record-keeping; to improve health data sharing; and to develop a comprehensive, life-long medical record for servicemembers. Table 1 summarizes their recommendations.
|
Commission |
Relevant Report Recommendations |
|
President's Advisory Committee on Gulf War Veterans' Illnesses (1996)a |
"DOD officials … should assign a high priority to dealing with the problems of lost or missing medical records. A computerized central database is important. Specialized databases must be compatible with the central database. Attention should be directed toward developing a mechanism for computerizing medical data (including classified information, if and when it is needed) in the field. DOD and VA should adopt standardized recordkeeping to ensure continuity." |
|
Congressional Commission on Service Members and Veterans Transition Assistance (1999)b |
"Require DOD and VA to ensure joint IT system replacements and enhancements in the future and maximize commercial off-the-self technology." "Require DOD and VA to jointly offer a single solicitation for replacement of DOD's and VA's legacy medical systems with integrated and interoperable systems." |
|
President's Task Force to Improve Health Care Delivery for Our Nation's Veterans (2003)c |
DOD and VA should develop and deploy "interoperable bidirectional standard space electronic medical records … by the year 2005." |
|
President's Commission on Care for America's Returning Wounded Warriors (2007)d |
"Make patient information available to all personnel who need it, initially in readable form." "Continue efforts for fully interoperable information system." "Develop a user-friendly single web portal for service members and veterans." |
Notes
a. Presidential Advisory Committee on Gulf War Veterans' Illnesses: Final Report, December 1996, p. 19.
b. Congressional Commission on Servicemembers and Veterans Transition Assistance: Final Report, January 14, 1999, p. 20.
c. Testimony of Co-Chair Gail R. Wilensky, President's Task Force to Improve Health Care Delivery for our Nation's Veterans, in U.S. Congress, House Veterans Affairs Committee, Report of the President's Task Force to Improve Health Care Delivery for our Nation's Veterans, hearings, 108th Cong., 1st sess., June 3, 2003.
d. Serve, Support, Simplify: Report of the President's Commission on Care for America's Returning Wounded Warriors, July 1, 2007, p. 28.
Between 1998 and 2009, DOD and VA established various methods to exchange limited patient health information across both departments, including:
- Federal Health Information Exchange (FHIE). Completed in 2004, the FHIE enables monthly data transmissions from DOD to VA comprised of patient demographics, laboratory/radiology results, outpatient pharmacy, allergies, and hospital admission data.32
- Bidirectional Health Information Exchange (BHIE). Completed in 2004, the BHIE enables real-time, two-way data transmissions (DOD-to-VA and VA-to-DOD) comprised of FHIE information, additional patient history and assessments, theater clinical data, and additional inpatient data.33
- Clinical Data Repository/Health Data Repository (CHDR). Completed in 2006, CHDR enables real-time, two-way data transmissions comprised of pharmacy and drug allergy information and a capability to add information to the patient's permanent medical record in the other department's repository.34
- Virtual Lifetime Electronic Record (VLER). Initiated in 2009, the VLER enables real-time, health information exchange between DOD and VA, as well as certain civilian health care providers.35
While these information exchange systems enable DOD and VA health care providers to view or modify limited health care data, both departments continue to operate separate, disparate health record systems.
Congress Mandates Interoperability
In 2008, Congress began legislating mandates for DOD and VA to establish fully interoperable EHR systems that would allow for health care data sharing across departments. Section 1635 of the National Defense Authorization Act (NDAA) for Fiscal Year (FY) 2008 (P.L. 110-181) directed DOD and VA to jointly: (1) "develop and implement electronic health record systems or capabilities that allow for full interoperability of personal health care information," and (2) "accelerate the exchange of health care information" between both departments. Additionally, Congress directed the establishment of an interagency program office (IPO) that would serve as a "single point of accountability" for rapid development and implementation of EHR systems or capabilities to exchange health care information.36
The FY2008 NDAA also directed the IPO to implement the following, no later than September 30, 2009:
"…electronic health record systems or capabilities that allow for full interoperability of personal health care information between the Department of Defense and Department of Veterans Affairs, which health records shall comply with applicable interoperability standards, implementation specifications, and certification criteria (including for the reporting quality measures) of the Federal Government."37
In the conference report accompanying the Department of Defense Appropriations Act, 2008 (H.Rept. 110-434, P.L. 110-116), Congress also directed DOD and VA to "issue a joint report" by March 3, 2008, that describes the "actions being taken by each department to achieve an interoperable electronic medical record (EMR)."38
On April 17, 2008, the IPO was established with temporary staff from DOD and VA.39 On December 30, 2008, the Deputy Secretary of Defense delegated oversight authority for the IPO to the Under Secretary of Defense for Personnel and Readiness (USD[P&R]). The FY2008 NDAA also directed the Secretary of Defense (SECDEF) to appoint the IPO Director, with concurrence of the Secretary of Veterans Affairs (SECVA); and the SECVA to appoint the IPO Deputy Director, with concurrence of the SECDEF.40
Establishing Interoperability Goals
To meet Congress's mandate on interoperability, the IPO established a mutual definition of interoperability. They posited it as the "ability of users to equally interpret (understand) unstructured or structured information which is shared (exchanged) between them in electronic form."41 Shortly after, both departments identified and adopted six areas of interoperability capabilities intended to meet the requirements and deadline established by Congress:
- Expand Essentris implementation across DOD.
- Demonstrate the operation of the Partnership Gateways in support of joint DOD and VA health information sharing.42
- Enhance sharing of DOD-captured social history with VA.
- Demonstrate an initial capability for DOD to scan medical documents into the DOD EHR and forward those documents electronically to VA.
- Provide all servicemembers' health assessment data stored in the DOD EHR to the VA in such a fashion that questions are associated with the responses.
- Provide initial capability to share with the VA electronic access to separation physical exam information captured in the DOD EHR.43
As a result of each department's work on interoperable capabilities, DOD and VA reported to Congress in 2010 that all requirements for "full" interoperability were met.44
The Integrated EHR Initiative
DOD and VA continued to work on integrating their respective EHR systems through individual initiatives, while considering a larger EHR modernization strategy. Three strategy options were considered:
- 1. develop a new, joint EHR;
- 2. upgrade and adopt an existing legacy system across both departments (i.e., AHLTA or VistA);45 or
- 3. pursue separate solutions that would have "common infrastructure with data interoperability."46
In March 2011, the SECDEF and SECVA agreed to work cooperatively to develop an integrated electronic health record (called the iEHR) that would eventually replace each department's legacy systems.47 The IPO was assigned the oversight role for the iEHR initiative, which was then set to begin implementation no later than 2017.
In February 2013, SECDEF and SECVA announced that they would no longer pursue the iEHR initiative. In making this decision, DOD and VA determined that the initial cost estimates for implementing the iEHR would be "significant," given the "constrained Federal Budget environment."48 After reevaluating their approach and considering alternatives, both departments decided to pursue other ongoing efforts to "improve data interoperability" and to preserve and develop separate EHR systems with a core set of capabilities that would allow for integrated sharing of health care data between DOD, VA, and private sector providers.49
Congressional Mandate for an EHR
|
National Defense Authorization Act for Fiscal Year 2014 (P.L. 113-66) Section 713(b) The Secretary of Defense and the Secretary of Veterans Affairs – (1) shall each ensure that the electronic health record system of the Department of Defense and the Department of Veterans Affairs are interoperable with an integrated display of data, or a single electronic health record, by complying with the national standards and architectural requirements identified by the Interagency Program Office of the Departments … in collaboration with the Office of the National Coordinator for Health Information Technology of the Department of Health and Human Services; and (2) shall each deploy modernized electronic health record software supporting clinicians of the Departments by no later than December 31, 2016, while ensuring continued support and compatibility with the interoperability platform and full standards-based interoperability. |
After DOD and VA announced their change to the iEHR strategy in 2013, Congress expressed its sense that both departments had "failed to implement a solution that allows for seamless electronic sharing of medical health care data."50 Given some Members' apparent frustration, Congress established a new deadline for both departments to deploy a new EHR solution. Section 713(b) of the NDAA for FY2014 (P.L. 113-66) directed DOD and VA to implement an interoperable EHR with an "integrated display of data, or a single electronic health record" by December 31, 2016 (see text box below).
The law also required DOD and VA to "jointly establish an executive committee" to support development of systems requirements, integration standards, and programmatic assessments to ensure compliance with Congress's direction outlined in Section 713(b).51
MHS Genesis
Given Congress's new mandate for both departments to implement an interoperable EHR, DOD conducted a 30-day review of the iEHR program in order to "determine the best approach" to meeting the law.52 While conducting its review, DOD identified two EHR modernization options that would support healthcare data interoperability with the VA: (1) adopt VistA and (2) acquire a commercial EHR system.53
DOD Acquisition Strategy
On May 21, 2013, the Secretary of Defense issued a memorandum directing the department's pursuit of "a full and open competition for a core set of capabilities for EHR modernization."54 The directive also delegated certain EHR responsibilities to various DOD leaders.
- Under Secretary of Defense for Acquisition, Technology, and Logistics (USD[AT&L]), whose office was later reorganized as the Under Secretary of Defense for Acquisition and Sustainment (USD[A&S]).55 Responsible for exercising milestone decision authority (MDA) and also holds technical and acquisition responsibilities for health records interoperability and related modernization programs;56
- Under Secretary of Defense for Personnel and Readiness (USD[P&R]). Lead coordinator on DOD health care interactions with the VA.
- Assistant Secretary of Defense for Health Affairs (ASD[HA]). Responsible for functional capabilities of the EHR.
Given the significant investments required to modernize DOD's EHR, MHS Genesis is a designated Defense Business System (DBS).57 Because it is a DBS, certain decision reviews and milestones are required as part of the overall acquisition process. DBS programs are subject to significant departmental and congressional oversight activities.
Requirements Development and Solicitation
From June 2013 to June 2014, USD(AT&L) directed the Defense Healthcare Management Systems Modernization Program Management Office (DHMSM PMO) to oversee the EHR requirements development process, draft an acquisition strategy and request for proposal (RFP), and conduct activities required by DOD policy for DBS acquisitions. The ASD(HA) directed the Defense Health Agency (DHA) to establish various working groups to identify and develop the clinical and nonclinical functional requirements for the new EHR. The DHA led each working group, which included representatives from each military service medical department. Keeping in alignment with DOD's guiding principles for EHR modernization (see Figure 2), the working groups identified approximately 60 overarching capabilities to be required of a new EHR. An initial draft RFP incorporated functional capability requirements with certain technical requirements for interoperability, information security, and suitability with DOD infrastructure.
 |
|
Source: Department of Defense, "EHR Guiding Principles," accessed May 2019, https://health.mil/Military-Health-Topics/Technology/Military-Electronic-Health-Record/EHR-Modernization-Interoperability/EHR-Guiding-Principles. |
The DHMSM PMO published three draft RFPs between January and June 2014 for interested contractors to review, provide comments, and submit questions for clarification on functional requirements. Additionally, the DHMSM PMO hosted four industry days that allowed interested contractors to "enhance their understanding of the DHMSM requirement," gain insight on DOD's requirements development process, and provide feedback on particular aspects of the draft RFP.58 These activities also allowed the DHMSM PMO to conduct market research that would inform further revision of MHS Genesis functional requirements or its overall acquisition strategy.
Between June 2014 and August 2014, DOD leaders certified that certain acquisition milestones had been achieved, allowing DOD to proceed with the solicitation process, including finalizing and approving all user-validated function requirements, approving the overall acquisition strategy, and issuing an authority to proceed.59 On August 25, 2014, DOD issued its official solicitation for proposals.60 The solicitation period concluded on October 9, 2014.
Source Selection Process
The source selection process took place from October 2014 to July 2015. DOD reportedly had received five proposals during the solicitation period.61 Most of the proposals were from partnered vendors consisting of health information management, electronic medical records, information technology, and program management organizations. These partnerships included:
- Allscripts, Computer Sciences Corporation, and Hewlett-Packard;
- IBM and Epic Systems;
- Cerner, Leidos, and Accenture Federal;
- PricewaterhouseCoopers, General Dynamics, DSS, Inc., MedSphere; and
- InterSystems.62
Consistent with DOD source selection procedures, DOD experts were assigned to review and apply the evaluation criteria published in the RFP, to each proposal.63 Figure 3 illustrates a general overview of the evaluation and source selection process.
|
Figure 3. Overview of the Source Selection Process for MHS Genesis |
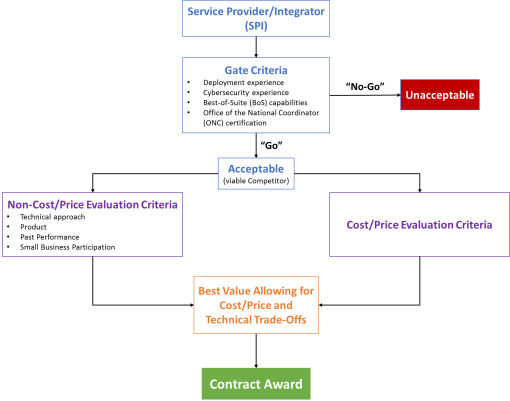 |
|
Source: PEO DHMS Presentation, "DoD EHR Modernization Effort: Acquisition Lessons Learned," HIMSS 2016 Conference and Exhibition, March 2, 2016, p. 17, https://www.himssconference.org/sites/himssconference/files/pdf/162.pdf. Notes: Graphic adapted by CRS. Service Provider/Integrator means the vendor and their submitted proposal. ONC = Office of the National Coordinator for Health Information Technology. |
Contract Award
On July 29, 2015, DOD awarded the MHS Genesis contract to Leidos Partnership for Defense Health (LPDH) to replace its legacy EHR systems with a commercial-off-the-shelf (COTS) EHR system.64 The contract has a potential 10-year ordering period that includes a two-year base period, two three-year optional ordering periods, and an award term period of up to two years.65 The initial total award ceiling for MHS Genesis was $4.3 billion.66
On June 15, 2018, DOD approved a contract modification to increase the award ceiling by $1.2 billion.67 According to the Justification and Approval for Other than Full and Open Competition documentation, the purpose of this increase was to "support the incorporation of the United States Coast Guard (USCG) into the [DOD] MHS Genesis Electronic Health Record (EHR) implementation" and "establish a common standardized EHR baseline with the USCG and the [VA]."68 The current award ceiling for MHS Genesis is more than $5.5 billion.
Leidos Partnership for Defense Health (LPDH)
Leidos leads LPDH with its core partners: Accenture Federal Services, Cerner, and Henry Schein One. The full partnership, through sub-contracts of the core partners, is comprised of over 34 businesses (see Figure 4).69
 |
|
Source: LPDH, "Our Partners," accessed May 23, 2019, http://leidosdefensehealth.com/about-us/meet-the-team/our-partners/. |
Capabilities
According to a redacted version of DOD's contract award documents, LPDH is required to meet the following overarching contract requirements:
- "unify and increase accessibility of integrated, evidence-based healthcare delivery and decision making";
- "support the availability of longitudinal medical records for 9.6 million DoD beneficiaries and approximately 153,000+ MHS personnel globally";
- "enable the application of standardized workflows, integrated healthcare delivery, and data standards for improved and secure electronic exchange of medical and patient data between the DoD and its external partners, including the [VA] and other Federal and private sector healthcare providers"; and
- "leverage data exchange capabilities in alignment with the [IPO] for standards-based health data interoperability and secure information sharing with external partners to include the VA."70
Additionally, there are over 95 specific capability requirements across four concepts of operations (i.e., health service delivery, health system support, health readiness, and force health protection) that MHS Genesis must support (see Appendix B).71
Governance
Ultimately, the Secretary of Defense is accountable for MHS Genesis. Various DOD entities, described below, have assigned responsibilities for MHS Genesis oversight, implementation, and sustainment (see Figure 5). While each entity has a separate chain of command, DOD chartered numerous governance groups to synchronize efforts across the department, delegate certain decisionmaking authorities, and provide direction on implementation and use of MHS Genesis.
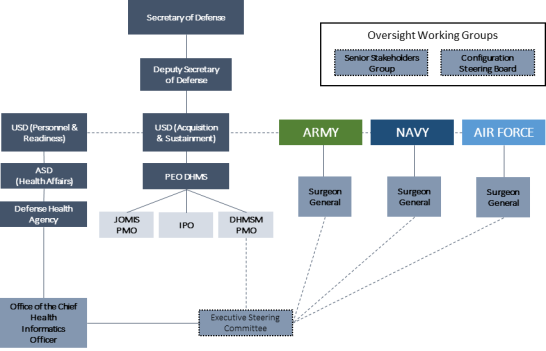 |
|
Source: CRS graphic based on Email communication with DOD officials, January 2019, and DHMS, "Fiscal Year 2018 Annual Report," p. 8, https://health.mil/Reference-Center/Reports/2019/02/22/Defense-Healthcare-Management-Systems-Fiscal-Year-2018-Annual-Report. Notes: USD = Under Secretary of Defense. ASD = Assistant Secretary of Defense. PEO DHMS = Program Executive Office for the Defense Healthcare Management Systems. JOMIS PMO = Joint Operational Medical Information Systems Program Management Office. IPO = Interagency Program Office. DHMSM PMO = Defense Healthcare Management Systems Modernization Program Management Office. |
Program Executive Office, Defense Healthcare Management Systems (PEO DHMS)
PEO DHMS was established in 2013.72 Its mission is to "transform the delivery of healthcare and advance data sharing through a modernized electronic health record for service members, veterans, and their families."73 It responsible for implementing MHS Genesis as the assigned acquisition authority and currently reports to the Under Secretary of Defense for Acquisition and Sustainment (USD[A&S]).74
Under the PEO DHMS, three program management offices (PMOs) are tasked with modernizing DOD's EHR system and ensuring health data interoperability with the VA.
- DOD Healthcare Management System Modernization (DHMSM) PMO. "Oversees the deployment of MHS Genesis and the operations and sustain of the Joint Legacy Viewer."
- DOD/VA Interagency Program Office (IPO). "Oversees the efforts of the DOD and VA to implement national health data standards for interoperability."
- Joint Operational Medicine Information Systems (JOMIS) PMO. "Develops, deploys, and sustains MHS Genesis and other integrated operational medicine information systems to deployed forces."75
Defense Health Agency (DHA)
In 2013, the Secretary of Defense established the DHA to manage the TRICARE program; execute appropriations for the Defense Health Program; coordinate management of certain multi-service health care markets and MTFs in the National Capital Region; exercise management responsibility for shared services, functions, and activities within the Military Health System; and support DOD's medical mission.76 DHA is a designated Combat Support Agency77 that is scheduled to soon administer and manage all MTFs.78
DHA serves as the lead entity for MHS Genesis requirements development, in coordination with the military service medical departments, and currently reports to the ASD(HA).79
Military Service Medical Departments
The military service medical departments are established under each respective military department to organize, train, and equip military medical personnel, maintain medical readiness of the Armed Forces, and administer, manage and provide health care in MTFs. The medical departments are led by a Surgeon General, who also functions as the principal advisor to their respective military service secretary and service chief for all health and medical matters.80 The three service medical departments are the Army Medical Command (MEDCOM), the Navy Bureau of Medicine and Surgery (BUMED), and the Air Force Medical Service (AFMS).
Each service medical department provides subject-matter expertise, functional support, and consultation to the DHMSM PMO.81
Senior Stakeholders Group (SSG) and the Configuration Steering Board (CSB)
The SSG and the CSB are DOD-chartered working groups established to provide oversight, recommendations, and "direction on health-related acquisition programs," including those within PEO DHMS.82 The SSG is chaired by the USD(A&S) and is responsible for receiving updates on DHMS acquisition programs, ensuring adherence to DOD's EHR guiding principles, and providing recommendations and feedback on key EHR and interoperability decisions. The CSB is co-chaired by the USD(A&S) and the USD(P&R) and is specifically responsible for oversight on DHMSM and JOMIS programs. Figure 6 outlines the membership of each group.
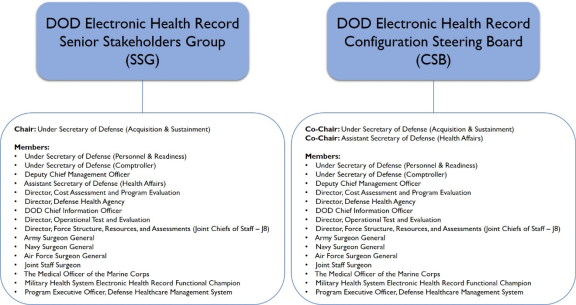 |
|
Source: DOD, "Department of Defense Electronic Health Record Senior Stakeholders Group and Defense Healthcare Management Systems Configuration Steering Board Charter," April 8, 2018. |
Executive Steering Board (ESB)
The ESB, previously named the Functional Champion Leadership Group (FLCG), is a governance body led by the DHA's Chief Health Informatics Officer with representation from each service medical department.83 The ESB's role is to:
- consider changes to standardized clinical, business, or technical processes;
- serve as a forum to validate, prioritize, and recommend modifications or new functional requirements for MHS Genesis; and
- oversee numerous working groups of subject matter experts and end-users.84
Office of the Chief Health Informatics Officer (OCHIO)
The OCHIO represents the "voice of the customer" to PEO DHMS.85 The office solicits input and recommendations from the ESB and coordinates with PEO DHMS to revise or modify MHS Genesis contract requirements. OCHIO is also responsible for "change management, early adoption activities, standardization of functional workflows, functional collaboration with the [VA], management of configuration changes to MHS Genesis, adjudication of functional trouble tickets, sustainment training, current state workflow assessments, and coordination of DHA policy to support the use of MHS Genesis."86
Deployment
DOD is using a phased implementation strategy to deploy MHS Genesis. Deployment began with its initial operational capability (IOC) sites in 2017. After the IOC sites, MHS Genesis is to be deployed at over 600 medical and dental facilities, grouped geographically into 23 waves (see Appendix F).87 DOD anticipates "full operational capability" and implementation of MHS Genesis at all MTFs by the end of 2024.88
Pre-Deployment Activities
During the approximately 17 months between the July 2015 contract award date and Congress's December 2016 deadline to implement a new EHR system, DOD conducted certain pre-deployment activities (e.g., systems engineering, systems integration, and testing prior to deploying MHS Genesis). DOD acquisition policies and certain contract requirements mandate these activities. Some of the initial requirements include:
- contractor site visits to "analyze operations, infrastructure, and detailed information for EHR System design and testing";
- gap analyses between existing site infrastructure, system requirements, and the contractor's system architecture;
- development of solutions to fill identified infrastructure gaps;
- testing interoperability with legacy systems;
- delivering various contractor plans to the government (e.g., integrated master plan, risk management plan, data management plan, disaster recovery plan, and cybersecurity vulnerability management plan);
- EHR system testing in government approved labs, including those conducted by the contractor, government independent testing and evaluation teams, and operational test agencies; and
- receiving authorization to proceed (ATP) with limited fielding at the IOC sites and to conduct an Initial Operational Test and Evaluation (IOT&E).89
Concurrently, the DOD Inspector General (DODIG) conducted a performance audit on the DHMSM PMO. The purpose of the audit was to determine if DOD had approved system requirements and if the MHS Genesis acquisition strategy was "properly approved and documented."90 The audit was conducted from June 2015 through January 2016, with a final report issued on May 31, 2016. Overall, the DODIG found that the MHS Genesis requirements and acquisition strategy were properly approved and documented. However, the report raised concerns about the program's execution schedule (i.e., implementation timeline) not being "realistic" to meet Congress's deadline.91 The DODIG recommended that the PEO DHMS conduct a "schedule analysis" to determine if IOC would be achievable by December 2016, and to continue monitoring program risks and report progress to Congress quarterly.92 In response to the DODIG's recommendation, the PEO DHMS asserted, "we remain confident we will achieve [IOC] later this year in accordance with the NDAA."93
Initial Deployment
As part of the implementation strategy, DOD selected MTFs in the Pacific Northwest as its IOC sites (see Table 2). On February 9, 2017, MTFs at Fairchild Air Force Base, Washington, were the first sites to transition to MHS Genesis.
|
Medical Facility |
Location |
Go-Live Date |
|
92nd Medical Group |
Fairchild Air Force Base, WA |
February 9, 2017 |
|
92nd Aeromedical-Dental Squadron |
Fairchild Air Force Base, WA |
February 9, 2017 |
|
Naval Health Clinic Oak Harbor |
Oak Harbor, WA |
July 21, 2017 |
|
Naval Hospital Bremerton |
Bremerton, WA |
September 22, 2017 |
|
Naval Branch Health Clinic Bangor |
Silverdale, WA |
September 22, 2017 |
|
Naval Health Clinic Everett |
Everett, WA |
September 22, 2017 |
|
Madigan Army Medical Center |
Joint Base Lewis-McChord, WA |
October 21, 2017 |
Source: DHMSM, "Attachment 12: Segment 1 MTF List and MTF Codes," Contract Award No. N00039-15-D-0044, p. 13; Madigan Army Medical Center presentation at the American College of Emergency Physicians' Government Services Symposium, March 2018, p. 4, http://www.gsacep.org/aws/GSACE/asset_manager/get_file/189215?ver=2.
Note: Go-Live Date is the day an MTF began using MHS Genesis in day-to-day operations.
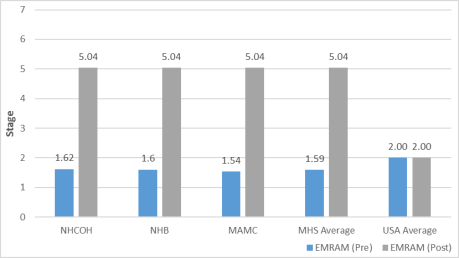
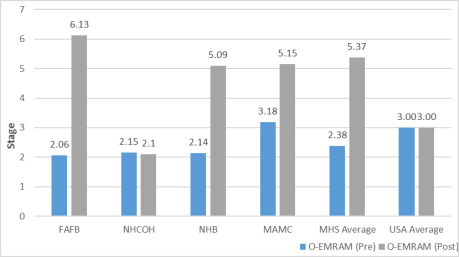
The purpose of fielding MHS Genesis at the IOC sites before full deployment was to observe, evaluate, and document lessons-learned on whether the new EHR was usable, interoperable, secure, and stable. DOD used several evaluation methods to measure MHS Genesis success at the IOC sites, including the Health Information Management Systems Society's (HIMSS) Electronic Medical Record Adoption Models (EMRAM) and the DOD IOT&E. The results of these assessments would later inform PEO DHMS in its decision to proceed with further deployments.
EMRAM Findings
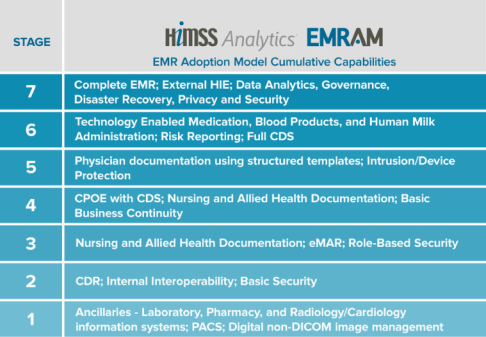
The EMRAM includes two commercially developed assessment tools that health systems and facilities can use to measure adoption of an electronic medical record (EMR) system. The general EMRAM is for inpatient facilities and O-EMRAM is for outpatient facilities. Both tools consist of a self-administered survey, which is then analyzed by HIMSS to produce an EMRAM score. The score, ranging from Stage 0 to Stage 7, describes the level of adoption and utilization of an EMR within a health care organization (see Appendix C). Generally, Stage 0 indicates minimal or no EMR adoption in a health care facility or clinic, whereas Stage 7 indicates complete EMR adoption, including demonstrated data sharing capabilities and eliminated use of paper charts.
Prior to the go-live dates at the IOC sites and while using its legacy systems, DOD's average score was 1.59 for the EMRAM and 2.38 for the O-EMRAM.94 After all IOC sites transitioned to MHS Genesis, DOD reassessed each IOC site and observed increased EMRAM scores (see Figure 7 and Figure 8). MTFs at Fairchild Air Force Base received a score of 6.13 on the O-EMRAM, whereas all other IOC sites scored 5.04.95 In comparison to U.S. civilian hospitals, the IOC sites scored higher than the national average for the EMRAM (2.00) and O-EMRAM (3.00).96 However, media reports on EMRAM scoring trends at the end of 2017 note that 66.7% of U.S. hospitals participating in the EMRAM reached "either Stage 5 or Stage 6."97 For the O-EMRAM, most participating outpatient facilities remained at Stage 1.98
|
Before and After Deployment |
 |
|
Source: PEO DHMS presentation at the HIMSS 2019 Conference, "MHS Genesis: Transforming the Delivery of Healthcare," February 12, 2019, p. 17, https://365.himss.org/sites/himss365/files/365/handouts/552803344/handout-43.pdf. Notes: Graphic adapted by CRS. NHOH = Naval Health Clinic Oak Harbor. NHB = Naval Hospital Bremerton. MAMC = Madigan Army Medical Center. |
|
Before and After Deployment |
 |
|
Source: PEO DHMS presentation at the HIMSS 2019 Conference, "MHS Genesis: Transforming the Delivery of Healthcare," February 12, 2019, p. 17, https://365.himss.org/sites/himss365/files/365/handouts/552803344/handout-43.pdf. Notes: Graphic adapted by CRS. NHOH = Naval Health Clinic Oak Harbor. NHB = Naval Hospital Bremerton. MAMC = Madigan Army Medical Center. |
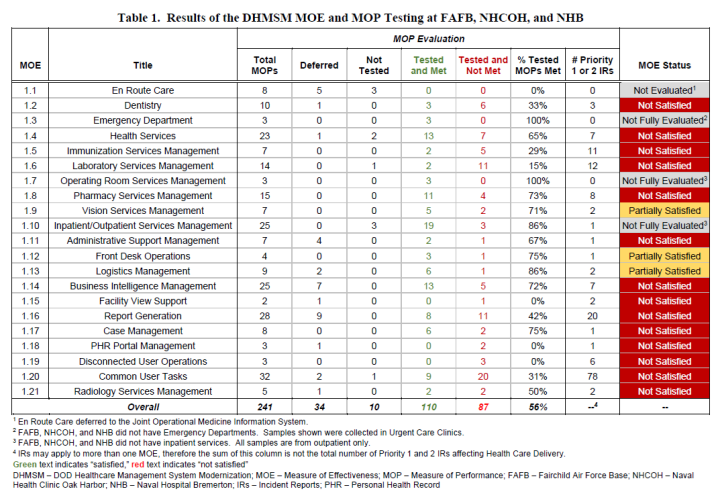
IOT&E Findings
DOD policy requires DBS programs to undergo an IOT&E to determine program or systems effectiveness and suitability.99 IOT&E findings provide the USD(A&S) and relevant acquisition or functional leadership with recommendations on whether a program, generally those with total contract values exceeding certain thresholds, should proceed with further implementation. Between September 2017 and December 2017, the Joint Interoperability Test Command (JITC) conducted an IOT&E at each IOC site, with the exception of Madigan Army Medical Center (MAMC).100 PEO DHMS postponed the MAMC IOT&E to 2018 in order to resolve issues identified at the other IOC sites.
While at each site, the JITC conducted initial cybersecurity testing, evaluated interoperability data, observed MTF staff performing day-to-day tasks using MHS Genesis, and administered user surveys on performance and suitability. The Director of Operational Test and Evaluation (DOT&E) reviewed JITC's IOT&E findings and applied them to the following criteria:
- Does MHS Genesis provide the capabilities to manage and document health-related services?
- Do MHS Genesis interfaces support or enable accomplishment of mission activities and tasks?
- Does MHS Genesis usability, training, support, and sustainment ensure continuous operations?
On April 30, 2018, DOT&E issued a partial IOT&E report asserting that MHS Genesis was "neither operationally effective nor operationally suitable."101 DOT&E found that:
MHS Genesis is not operationally effective because it does not demonstrate enough workable functionality to manage and document patient care. Users successfully performed only 56 percent of the 197 tasks used as Measures of Performance. MHS Genesis is not operationally suitable because of poor system usability, insufficient training, and inadequate help desk support. Survivability is undetermined because cybersecurity testing is ongoing.102
See Appendix D for IOT&E summary results by measure of effectiveness and measure of performance evaluation.
Based on these preliminary findings, DOT&E recommended to the USD(A&S) a delay in further deployment of MHS Genesis until a full IOT&E was completed and the DHMSM PMO corrected "outstanding deficiencies."103 Additional recommendations for the DHMSM PMO included:
- "Fix all Priority 1 and 2 [incident reports] with particular attention given to those that users identified as potential patient safety concerns, and verify fixes through operational testing.
- Improve training and system documentation for both users and Adoption Coaches.
- Increase the number of Adoption Coaches and leave them on site until users are more comfortable with the new processes.
- Complete cybersecurity operational testing and continue to fix known deficiencies.
- Work with users to document, reduce, and standardize operational workarounds.
- Improve interoperability, focusing on interfaces identified as problematic during IOT&E.
- Monitor reliability and availability throughout the system lifecycle.
- Work with the Defense Health Agency and DISA to isolate network communications problems and reduce latency.
- Conduct operational testing at MAMC to evaluate untested functionality and corrective actions taken by the [DHMSM] PMO.
- Conduct follow-on operational testing at the next fielding site to evaluate revised training and Go-Live process improvements."104
On November 30, 2018, DOT&E issued a final IOT&E report, incorporating results from delayed testing at MAMC. DOD has not made the final report publicly available. DOT&E acknowledges ongoing improvements, but maintains that MHS Genesis is "not yet effective or operationally suitable."105 A summary of the IOT&E released by the department describes several ongoing issue themes previously identified and described in the partial IOT&E report (e.g., continued incident reports, staff training, change management, and workflow adoption).106 With regard to cybersecurity, DOT&E described MHS Genesis as "not survivable in a cyber-contested environment."107 In conjunction with the IOT&E, DOD "successfully executed" three cyberspace test attacks against MHS Genesis, highlighting potential security gaps and vulnerabilities with the new EHR system.108
Notwithstanding DOT&E's findings and recommendations, the DOD Chief Information Officer issued a conditional Authorization to Operate, valid for 12 months.109 Additionally, PEO DHMS concurred with DOT&E's recommendation for a follow-on operational test and evaluation "at the next fielding to evaluate corrective actions and revised training, to inform future fielding decisions."110
Selected Initial Deployment Issues
Since February 2017, DOD has documented numerous issues requiring mitigation strategies prior to deploying the first wave. Selected issues reported by various DOD entities, LPDH, MHS Genesis users, and media outlets are summarized below.
Trouble Ticket Backlog
During the initial deployment, DHMSM PMO established a single process for all IOC sites to identify, document, and report MHS Genesis issues. Users encountering system inconsistencies, technical errors, or clinical inaccuracies must submit a "trouble ticket" to a global service center (GSC). Users can also submit recommendations for changes to current workflows or system configurations to the GSC, as well as through their chain of command. The GSC is a contracted service that reviews, sorts, and assigns technical trouble tickets to LDPH or its sub-contractors for resolution. The GSC also assigns trouble tickets relating to functional capabilities, requirements, or workflows to DHMSM PMO or DHA for further review and adjudication.111
In April 2018, PEO DHMS reported that 1,000 of approximately 7,000 total trouble tickets generated by users throughout all IOC sites from January 2018 to that point had been resolved.112 Of the remaining trouble tickets, DHMSM PMO approved 2,000 for "work by the Leidos Partnership," while 2,500 were in review for further adjudication. CRS is unable to ascertain the status of the remaining 1,500 trouble tickets and the timeline in which they may have been resolved. In December 2018, PEO DHMS estimated that 3,607 open trouble tickets remained for resolution.113 As of October 14, 2019, PEO DHMS estimated 3,238 open trouble tickets from the IOC sites and 787 open trouble tickets from the first wave sites remained for resolution.114
Lengthy Issue Resolution Process
MHS Genesis users at IOC sites described the issue resolution process as lengthy and lacking transparency.115 User concerns included: (1) tickets submitted to the GSC were resolved in a period of time that was "not acceptable for all issues"; (2) the length of time for decisionmakers to determine a solution; and (3) discovering that a solution had been implemented during a periodic system update, rather than being notified by DHMSM PMO, DHA, or LPDH.116 Unlike DOD's legacy systems, MHS Genesis is to be a standardized EHR platform across all military treatment facilities and is not customizable for each site. Technical or functional changes to MHS Genesis require DHA-led working groups and DHMSM PMO to review and approve such changes before directing LPDH to implement a solution. Changes exceeding the scope of the MHS Genesis contract require additional review, resourcing, and approval by the acquisition authority.117
Inadequate Staff Training
Users reported that initial training provided four months prior to go-live was inadequate and did not allow super users to "absorb/fully grasp one role before being introduced to the next role."118 Staff members were required to complete computer-based training, followed by instructor-led courses. Course curricula varied by user roles (e.g., clinician, clinical support, administrative staff). Users reported that the LPDH training focused primarily on navigating the various modules and features of MHS Genesis and did not include training on clinical or administrative workflows.119 For example, primary care clinic nurses were trained on the applicable MHS Genesis modules that would likely be found in the primary care setting. They said they were not trained on accessing other modules that would typically be used outside of the primary care setting, as part of a patient assessment or development of a treatment plan.
Capability Gaps and Limitations
Users reported having little or no ability to track military medical and dental readiness requirements in MHS Genesis.120 Pre-built reports to monitor certain health care quality and access metrics were available to MTF staff. Users defaulted to developing local, "home-grown" work-around tools in Microsoft Office products in order to meet specific DOD and military service requirements for tracking medical and dental readiness.121 For example, certain dental data documented in MHS Genesis were not available for data-mining or viewing in legacy dental readiness reporting systems. To compensate for this, dental clinic staff at each IOC site transcribed or manually maintained dental readiness reports by reviewing dental data in both Dentrix (MHS Genesis' dental module) and CDS (the legacy dental system).
Future Deployments
In reviewing the experience and challenges documented during MHS Genesis deployment at the IOC sites, DOD noted that they "captured lessons learned, collaborated with our stakeholders, and optimized the system to enhance user adoption. Specific areas of improvement include network optimization, change management, and training enhancements."122 As such, DOD commenced the first wave of MHS Genesis deployments in September 2019. The deployment began with four MTFs in California and Idaho.123 Each wave is to last 18 months and is to include three major phases: pre-deployment planning with each MTF (3 months), deployment activities (12 months), and post go-live activities (3 months).124 As outlined in DOD's deployment schedule (see Appendix F), a new wave is to begin every three months at designated MTFs through late 2022, with wave 23 scheduled to conclude in 2024.
Issues for Congress
Congressional Oversight
Since mid-1980s, Congress has kept abreast of DOD's efforts to implement, sustain, or modernize its EHR systems.125 Previous congressional oversight activities have primarily focused on (1) understanding DOD's EHR modernization strategy and how the strategy would integrate interoperability and improve coordination with the VA, or (2) describing certain barriers that delayed previous modernization initiatives.
Currently, 12 congressional committees may exercise oversight authority of the broader EHR modernization efforts taking place in DOD, VA and USCG. The committees include:
- House Appropriations Committee.
- House Armed Services Committee.
- House Committee on Oversight and Reform.
- House Committee on Transportation and Infrastructure.
- House Veterans Affairs Committee.
- Senate Appropriations Committee.
- Senate Armed Services Committee.
- Senate Committee on Commerce, Science, and Transportation.
- Senate Committee on Homeland Security and Governmental Affairs.
Given the complexity, size, and timeline of DOD's EHR modernization effort, as well as parallel efforts by the USCG and VA, a coordinated oversight strategy may be necessary. Such a strategy could allow Congress to conduct a wide range of oversight activities without creating redundancies for committee staff and executive branch officials and could facilitate information-sharing among congressional stakeholders.
Since the initial deployment of MHS Genesis, there have been no congressional oversight hearings held solely on DOD's EHR modernization effort. On June 20, 2018, the House Committee on Veterans' Affairs established the Subcommittee on Technology Modernization.126 The role of the new subcommittee is to "focus on conducting oversight of the EHR Modernization program and other major technology projects at the Department of Veterans Affairs."127 Both DOD and VA officials testified before the subcommittee at its June 2019 oversight hearing.128
Interagency Governance
In September 2018, then-SECDEF James Mattis and current SECVA Robert Wilkie signed a joint statement (see Appendix G) that outlined each department's commitment to "implementing a single, seamlessly integrated [EHR] that will accurately and efficiently share health data … and ensure health record interoperability with our networks of supporting community healthcare providers."129 On April 3, 2019, DOD announced plans to re-charter the IPO into the "Federal Electronic Health Record Modernization (FEHRM)" program office.130 The new office would serve as an interagency governance group that provides oversight on DOD and VA's EHR modernization efforts and would have the "authority to direct each Department to execute joint decisions for technical, programmatic, and functional functions."131 DOD stated that the FEHRM Director and Deputy Director will be appointed positions and will report to both the Deputy SECDEF and Deputy SECVA.
While Congress directed the creation of the IPO in 2008, neither DOD nor VA has indicated if additional authorities, funding, or changes to current law are required to sustain the FEHRM program office. Congress may also examine the relationships between existing interagency governance groups (e.g., Joint Executive Committee), PEO DHMS, VA EHR Modernization Office, and the newly established FEHRM program office.
Limited Competition in Future Procurement
Because MHS Genesis is being deployed across all MTFs and all USCG sites, as well as VA sites transitioning to a Cerner-based EHR system, observers have noted that this is the "largest EHR undertaking in the country."132 Implementing a single EHR platform across three federal departments can produce certain economies of scale and standardization. However, the scale of these efforts can also result in future acquisition challenges particularly with conducting a full and open competition to procuring new requirements, or with follow-on contracts to sustain each EHR system. Congress may seek to understand how DOD and VA exercised their statutory authorities, provided through the Competition in Contracting Act of 1984 (P.L. 98-369), to procure their EHR systems, as well as the possible impact of limited competition in future procurement activities needed to sustain both MHS Genesis and the VA's new EHR system.133
Generally, all federal departments procuring property, goods, or services are required to employ an acquisition process that allows for full and open competition.134 This process permits all potential vendors to "submit sealed bids or competitive proposals on the procurement."135 For MHS Genesis, DOD's initial acquisition process included full and open competition. However, the process was not employed for subsequent requirements that were discovered after the initial award to LPDH. These additional requirements included upgrading DOD network infrastructure; incorporating USCG-specific requirements and clinic sites; and establishing common standards among DOD, VA, and USCG. The estimated value of the additional requirements was over $1.2 billion.136 DOD exercised its statutory authority to award a sole source contract modification to LPDH, citing that contracting with any other vendor would potentially "create significant redundancies, inefficiencies, and other issues."137
DOD's acquisition strategy anticipates "one or more competitive follow-on contracts to sustain the EHR solution, for which the Government owns a perpetual license, at the conclusion of the performance of the basic contract."138 However, Cerner declined DOD's request to enter into negotiations regarding the rights of its intellectual property.139 If DOD does not retain certain intellectual property rights on MHS Genesis, the Department may be limited in what EHR vendors it can consider when it becomes necessary to solicit for an MHS Genesis sustainment contract.
Glossary of Acronyms
|
AFMS |
Air Force Medical Service |
FHIE |
Federal Health Information Exchange |
|
AHLTA |
Armed Forces Health Longitudinal Technology Application |
FEHRM |
Federal Electronic Health Record Modernization |
|
ASD(HA) |
Assistant Secretary of Defense for Health Affairs |
GAO |
Government Accountability Office |
|
ASIMS |
Aeromedical Services Information Management Systems |
GSC |
Global Service Center |
|
BHIE |
Bidirectional Health Information Exchange |
HAIMS |
Health Artifact and Image Management System |
|
BUMED |
Navy Bureau of Medicine and Surgery |
HEC |
Health Executive Council |
|
CDS |
Corporate Dental System |
HIMSS |
Health Information Management Systems Society |
|
CHCS |
Composite Health Care System |
iEHR |
Integrated Electronic Health Record |
|
CHCS II |
Composite Health Care System II (i.e., AHLTA) |
IOC |
Initial Operational Capability |
|
CHDR |
Clinical Data Repository/Health Data Repository |
IOT&E |
Initial Operational Test and Evaluation |
|
COTS |
Commercial-Off-the-Shelf |
IPO |
Interagency Program Office |
|
CRS |
Congressional Research Service |
JEC |
Joint Executive Committee |
|
CSB |
Configuration Steering Board |
JITC |
Joint Interoperability Test Command |
|
DHA |
Defense Health Agency |
JLV |
Joint Legacy Viewer |
|
DHMSM PMO |
Defense Healthcare Management Systems Modernization Program Management Office |
JOMIS |
Joint Operational Medical Information System |
|
DOD |
Department of Defense |
LPDH |
Leidos Partnership for Defense Health |
|
DODIG |
Department of Defense Inspector General |
MAMC |
Madigan Army Medical Center |
|
DOT&E |
Director, Operational Test & Evaluation |
MDA |
Milestone Decision Authority |
|
EHR |
Electronic Health Record |
MEDCOM |
U.S. Army Medical Command |
|
EMR |
Electronic Medical Record |
MEDPROS |
U.S. Army Medical Protection System |
|
EMRAM |
Electronic Medical Record Adoption Model |
MHS |
Military Health System |
|
ESB |
Executive Steering Committee |
MRRS |
Medical Readiness Reporting System |
|
FCLG |
Functional Champion Leadership Group |
MTF |
Military Treatment Facility |
|
NDAA |
National Defense Authorization Act |
SSG |
Senior Stakeholder Group |
|
NSTR |
Non-Service Treatment Record |
STR |
Service Treatment Record |
|
OCHIO |
Office of the Chief Health Informatics Officer |
TMIP-J |
Theater Medical Information Program-Joint |
|
O-EMRAM |
Federal Health Information Exchange |
USCG |
U.S. Coast Guard |
|
OHTR |
Occupational Health Civilian Employee Treatment Record |
USD(A&S) |
Under Secretary of Defense for Acquisition and Sustainment |
|
PEO DHMS |
Program Executive Officer for the Defense Healthcare Management Systems |
USD(AT&L) |
Under Secretary of Defense for Acquisition, Technology, and Logistics |
|
SAIC |
Science Applications International Corporation |
USD(P&R) |
Under Secretary of Defense for Personnel and Readiness |
|
SECDEF |
Secretary of Defense |
VA |
Department of Veterans Affairs |
|
SECVA |
Secretary of Veterans Affairs |
VistA |
Veterans Information Systems and Technology Architecture |
Appendix B. MHS Genesis Functional Capability Requirements
|
Health Service Delivery |
||
|
|
|
|
Health System Support |
||
|
|
|
|
Health Readiness |
||
|
|
|
|
Force Health Protection |
||
|
|
|
Source: DHMSM, "Attachment 8: Health Service Delivery Concept of Operations (CONOPS)," Contract Award No. N00039-15-D-0044, p. 3; DHMSM, "Attachment 9: Health System Support Concept of Operations (CONOPS)," Contract Award No. N00039-15-D-0044, p. 2; DHMSM, "Attachment 10: Health Readiness Concept of Operations (CONOPS)," Contract Award No. N00039-15-D-0044, pp. i-ii; DHMSM, "Attachment 11: Force Health Protection Concept of Operations (CONOPS)," Contract Award No. N00039-15-D-0044, p. 2.
Appendix C. Stages of Electronic Medical Record Adoption and Utilization
|
Figure C-1. Stages of Electronic Medical Record (EMR) Adoption Health Information Management Systems Society |
 |
|
Source: HIMSS Analytics, "EMRAM Information Sheet," accessed June 4, 2019, http://www.himssanalytics.org/sites/himssanalytics/files/North_America_EMRAM_Information_2018.pdf. Notes: EMR = Electronic Medical Record; HIE = Health Information Exchange; CDS = Clinical Decision Support; CPOE = Computerized Practitioner Order Entry; eMAR = Electronic Medication Administration; PACS = Picture Archiving and Communication System; DICOM = Digital Imaging and Communications in Medicine. |
Appendix D. IOT&E Summary Results
Appendix E. Methodology for CRS Focus Groups on MHS Genesis
Background
On July 8-13, 2018, analysts from the Congressional Research Service (CRS) participated in a congressional staff delegation visit to various DOD facilities in the Puget Sound area of Washington State. DOD facilities visited were Madigan Army Medical Center, Naval Hospital Bremerton, and the Puyallup Community Medical Home. The purpose of the visit was to:
- review milestones, achievements, and challenges associated with the implementation of MHS Genesis; and
- understand implementation and continuous improvement processes utilized at initial operational capability sites.
Methodology
At each site, CRS conducted numerous focus groups comprised of various MTF staff members. Each focus group was comprised of 5–15 staff members selected by the MTF commander or his/her designee.
Madigan Army Medical Center
- Focus Group #1: Patient Administration Division, Managed Care and Scheduling, and Patient Satisfaction Department representatives
- Focus Group #2: Health care providers (e.g., physicians, dentists, psychologists, physicians assistants)
- Focus Group #3: Nurses
Naval Hospital Bremerton
- Focus Group #1: Nurses
- Focus Group #2: Health care providers (e.g., physicians, dentists, psychologists, physicians assistants)
- Focus Group #3: Enlisted personnel
- Focus Group #4: Patient Administration, Referral Management, and Patient Relations representatives
Puyallup Community Medical Home
- Focus Group #1: Health care providers, nurses, health care administrators, enlisted personnel
Prior to each site visit, CRS provided each MTF with questions for discussion during each focus group. CRS documented the themes and responses to each of the following questions:
- What challenges have you experienced with implementing MHS Genesis?
- How have you locally mitigated these issues?
- Are the mitigation processes in place working?
- Have these challenges impacted force readiness, access to care, quality of care, cost of care, or patient experience?
Appendix F. MHS Genesis Deployment Schedule
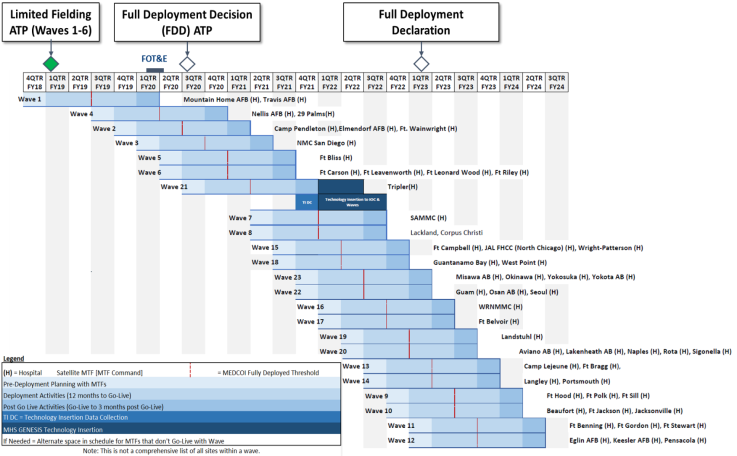 |
|
Source: Defense Healthcare Management Systems, May 2019. Notes: Not all MTFs are listed within a wave. |
Appendix G. DOD and VA EHR Joint Commitment Statement
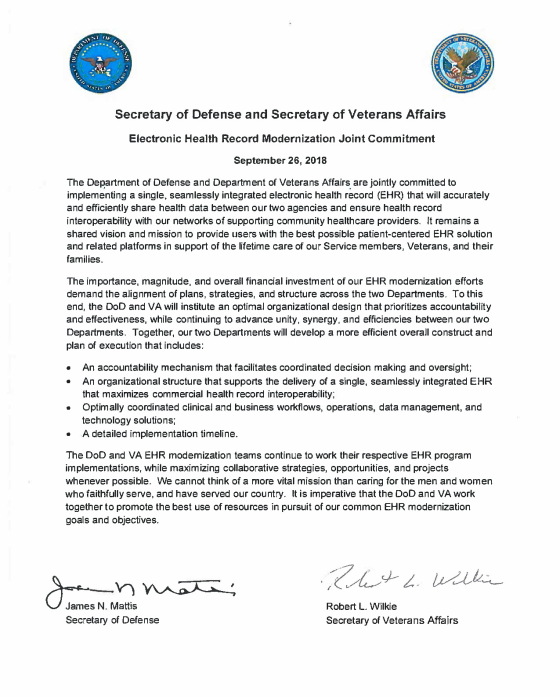 |
|
Source: Department of Defense and Department of Veterans Affairs, "Electronic Health Record Modernization Joint Commitment," September 26, 2018, https://www.va.gov/opa/publications/docs/EHRM-Joint-Commitment-Statement.pdf. |
Background
On July 8-13, 2018, analysts from the Congressional Research Service (CRS) participated in a congressional staff delegation visit to various DOD facilities in the Puget Sound area of Washington State. DOD facilities visited were Madigan Army Medical Center, Naval Hospital Bremerton, and the Puyallup Community Medical Home. The purpose of the visit was to:
- review milestones, achievements, and challenges associated with the implementation of MHS Genesis; and
- understand implementation and continuous improvement processes utilized at initial operational capability sites.
Methodology
At each site, CRS conducted numerous focus groups comprised of various MTF staff members. Each focus group was comprised of 5–15 staff members selected by the MTF commander or his/her designee.
Madigan Army Medical Center
- Focus Group #1: Patient Administration Division, Managed Care and Scheduling, and Patient Satisfaction Department representatives
- Focus Group #2: Health care providers (e.g., physicians, dentists, psychologists, physicians assistants)
- Focus Group #3: Nurses
Naval Hospital Bremerton
- Focus Group #1: Nurses
- Focus Group #2: Health care providers (e.g., physicians, dentists, psychologists, physicians assistants)
- Focus Group #3: Enlisted personnel
- Focus Group #4: Patient Administration, Referral Management, and Patient Relations representatives
Puyallup Community Medical Home
- Focus Group #1: Health care providers, nurses, health care administrators, enlisted personnel
Prior to each site visit, CRS provided each MTF with questions for discussion during each focus group. CRS documented the themes and responses to each of the following questions:
- What challenges have you experienced with implementing MHS Genesis?
- How have you locally mitigated these issues?
- Are the mitigation processes in place working?
- Have these challenges impacted force readiness, access to care, quality of care, cost of care, or patient experience?