Congress has long taken an interest in infectious disease prevention and control. Measles is a highly contagious virus that is transmitted through droplets emitted from an infected person when coughing and sneezing. The virus can live for up to two hours in the airspace or on a surface where an infected person coughed or sneezed. Other people can contract the disease if they breathe contaminated air or touch their eyes, nose, or mouth after touching a contaminated surface. Up to 90% of those in the proximity of an infected person who are not immune to the disease will be infected. Symptoms usually include high fever, rash, runny nose, and ear infections. Measles can also cause hearing loss, blindness, encephalitis (an infection that causes brain swelling), severe diarrhea, and severe respiratory infections such as pneumonia. The U.S. Centers for Disease Control and Prevention (CDC) estimates that up to two of every 1,000 children infected with measles will die.
Vaccines
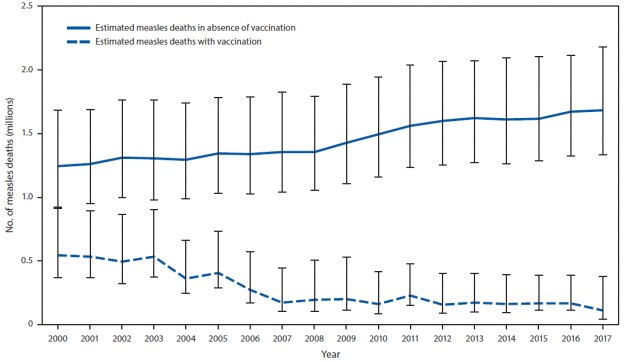
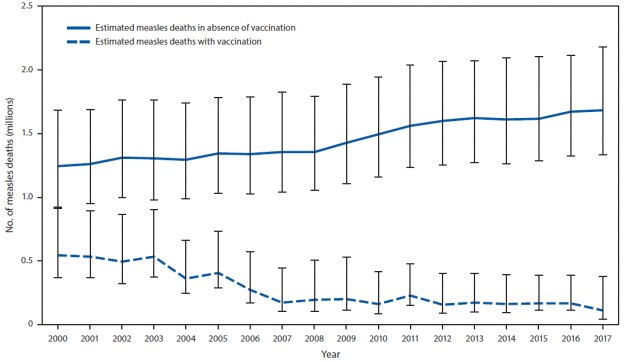
According to the CDC, the measles, mumps, and rubella (MMR) vaccine is 97% effective in preventing infection and related deaths, and routine MMR vaccination is recommended for all children. Figure 1 shows the estimated number of measles deaths globally, disaggregated by MMR immunization status. In countries with high case and death rates, the World Health Organization (WHO) recommends mass immunization campaigns and routine MMR vaccinations for children.
In 2000 the World Health Assembly, the decisionmaking body of the WHO, endorsed the Global Vaccine Action Plan, which aimed to eliminate measles in five WHO regions by 2020. A global measles vaccination campaign ensued, and between 2000 and 2017 it resulted in an 80% drop in deaths from the disease and saved an estimated 21 million lives.
|
Figure 1. CDC Estimate: Annual Number of Measles Deaths, with and Without Vaccination Programs, Worldwide, 2010-2017
|
 |
|
Source: Adapted by CRS from Dabbagh, A. et al., 2017.
Note: Deaths prevented by vaccination are indicated by the area between estimated deaths with vaccination and those without vaccination (cumulative total of 21.1 million deaths prevented during 2000–2017). Error bars represent upper and lower 95% confidence limits around the point estimate.
|
By the end of 2017, 85% of children worldwide had received one MMR dose by their second birthday, while 67% of children received the recommended two MMR doses. A 95% vaccination rate is necessary to achieve herd immunity and stop outbreak spread. Unvaccinated children and pregnant women are at the highest risk of measles and subsequent complications, including death. In 2017, there were 110,000 measles deaths globally, the majority of which were in children under five.
Regional Trends in Measles Cases
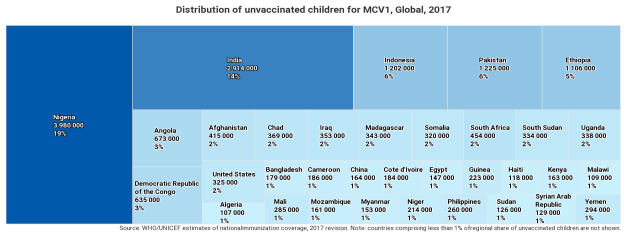
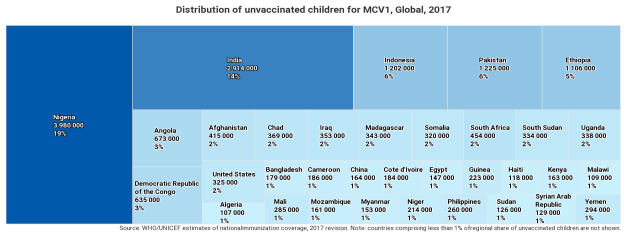
Despite the global increase in vaccination rates, measles outbreaks continue to occur. According to the WHO, one factor driving outbreaks is poverty: medical systems in many afflicted nations remain underfunded and weak, unable to vaccinate enough children to stop the virus' spread. Today, there are an estimated 21 million unvaccinated infants globally, half of whom are in five countries: Nigeria, India, Pakistan, Indonesia, and Ethiopia (see Figure 2).
|
Figure 2. Global Distribution of Children Without Measles Antigen-Containing Vaccines (MCV), 2017
|
 |
|
Source: Adapted by CRS from WHO/UNICEF estimates of national immunization coverage.
Note: Countries comprising less than 1% of regional share of unvaccinated children are not shown.
|
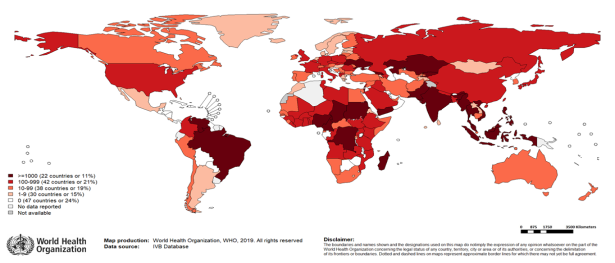
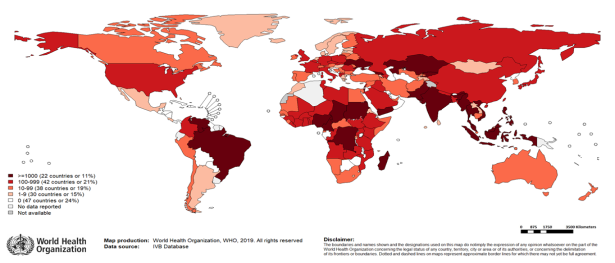
Middle- and high-income countries are experiencing a resurgence of measles, due to a variety of socioeconomic, political, and cultural factors. In April 2019, the WHO reported a 300% increase in global measles cases compared to the same period in 2018. The Americas, the Middle East and Europe had the greatest upsurge in cases. Figure 3 maps out recent measles cases reported to the WHO.
|
Figure 3. Measles Cases Reported to the WHO, September 2018-February 2019
|
 |
|
Source: World Health Organization, 2019.
Notes: Based on September 2018-February 2019 surveillance data received by the WHO in April 2019.
|
In the Americas, the increase in measles cases is concentrated in three countries: the United States, Venezuela, and Brazil. In the United States, the increase in measles cases is largely because of low vaccination coverage in minority religious community pockets, and misinformation related to vaccines that has caused "vaccine hesitancy." The WHO considers vaccine hesitancy, defined as a "delay in acceptance or refusal of vaccines despite availability of vaccination services," to be one of the 10 biggest global public health threats. Venezuela, which had previously eradicated the disease, has seen a resurgence of measles cases, due in part to political and economic instability. The country's health system has collapsed, interrupting basic health services including routine vaccination campaigns. As a result, measles has returned and spread, primarily among vulnerable indigenous communities. Venezuelan refugees have caused an increase in cases throughout the region, with Brazil seeing the largest increase due to the shared Amazonian border with Venezuela.
In Europe, misinformation about vaccines and renewed interest in natural and non-GMO products have also led to vaccine hesitancy. As in the United States, experts believe that vaccine hesitancy is responsible for the increase in measles cases in Europe.
In the Middle East, the largest surge in measles cases has been in Yemen, which experts believe is due to the country's protracted conflict and humanitarian crisis.
Relevant Agencies and U.S. Government Response
Congress has historically recognized the importance of vaccinations and immunizations. Through annual appropriations for the Department of Health and Human Services, and the Department of State, Congress funds CDC and the United States Agency for International Development (USAID) global immunization activities, as well as funding for the Global Alliance for Vaccines and Immunization (GAVI).
USAID and the CDC are the primary U.S. agencies involved in immunization provision and implementation internationally. Guided by the 2016-2020 Strategic Framework for Global Immunization, the agencies work with country governments to strengthen immunization programs through infectious disease surveillance, increasing laboratory capacity, and public health workforce capacity. They also support national routine immunization efforts through enhanced supply chain management and product procurement assistance. Related efforts are implemented bilaterally and through international partnerships with the WHO, UNICEF, the World Bank, and others.